Medial ankle ligament: Difference between revisions
No edit summary |
No edit summary |
||
| Line 60: | Line 60: | ||
First and second degree sprains are typically managed with conservative treatment. In the early stages, the conservative treatment consists of [http://www.physio-pedia.com/RICE RICE] (rest, ice, compress, elevate) and mobilization to prevent range of motion loss. When pain and inflammation are controlled, we can start with therapeutic exercises to increase the range of motion stability, strength proprioception and function. | First and second degree sprains are typically managed with conservative treatment. In the early stages, the conservative treatment consists of [http://www.physio-pedia.com/RICE RICE] (rest, ice, compress, elevate) and mobilization to prevent range of motion loss. When pain and inflammation are controlled, we can start with therapeutic exercises to increase the range of motion stability, strength proprioception and function. | ||
{{#ev: youtube |3TYj_ugUM7w}} | {{#ev: youtube |3TYj_ugUM7w}} | ||
For third degree sprains, structural damage has most likely occurred mostly needing surgical interventions. After the surgery, the [http://www.physio-pedia.com/Ankle_%26_Foot ankle] is immobilized. In case there is pain or oedema after | For third degree sprains, structural damage has most likely occurred mostly needing surgical interventions. After the surgery, the [http://www.physio-pedia.com/Ankle_%26_Foot ankle] is immobilized. In case there is pain or oedema after immobilization, the first treatment protocol is to attend to the pain and oedema. This will follow the same guidelines same as for the first and second degree sprains conservative management as above. | ||
After two weeks or as and when the pain and swelling allows, strengthening exercises for the medial muscles and ligaments of the [http://www.physio-pedia.com/Ankle_%26_Foot ankle] can be started. The strengthening programme can be started with low resistance exercises. For example, the patient sits on a chair or massage table with his/her leg extended (log sitting). The physiotherapist stabilises the leg with one hand just below the knee. With the other, the lateral side of the[http://www.physio-pedia.com/Ankle_%26_Foot ankle] is held. The physiotherapist moves the foot into inversion, and provides some manual resistance. The patient then has to perform eversion movement, against this resistance. The resistance is held for 3 to 5 seconds. The exercise is repeated for 10 to 12 times. <ref>Carl G. Mattacola et al, Rehabilitation of the ankle after acute sprain or chronic instability, Journal of Athletic Training, 2002 (level of evidence 2A)</ref>(level of evidence 2A) | After two weeks or as and when the pain and swelling allows, strengthening exercises for the medial muscles and ligaments of the [http://www.physio-pedia.com/Ankle_%26_Foot ankle] can be started. The strengthening programme can be started with low resistance exercises. For example, the patient sits on a chair or massage table with his/her leg extended (log sitting). The physiotherapist stabilises the leg with one hand just below the knee. With the other, the lateral side of the [http://www.physio-pedia.com/Ankle_%26_Foot ankle] is held. The physiotherapist moves the foot into inversion, and provides some manual resistance. The patient then has to perform eversion movement, against this resistance. The resistance is held for 3 to 5 seconds. The exercise is repeated for 10 to 12 times. <ref>Carl G. Mattacola et al, Rehabilitation of the ankle after acute sprain or chronic instability, Journal of Athletic Training, 2002 (level of evidence 2A)</ref>(level of evidence 2A) | ||
<br> | <br>This exercise can also be done without the resistance of a physiotherapist. The patient sits on a chair. An elastic tubing or resistance band is put around the foot, and the other foot is placed on the elastic tubing, while holding the elastic tubing in the contralateral hand. The same exercise as above is performed but with out a therapist, but using the band as the resistance. The patient pushes the foot outward, with the footpad away from the midline of the body. | ||
<br>Proprioceptive exercises can be commenced after 5 weeks.<br>Exercise for training the proprioception, the double-leg right/left condition, the subjects had to sit on a chair, with their feet on a kinaesthetic ankle board. They had to keep their knees at a 90° angle, while maintaining contact with the top of the KAB with their respective extremities. Then they had to rotate the board to the left side and then back to the right (=clockwise and counter clockwise). The subjects had to keep the side of the board in the floor each time they moved the board to the left or the right. Each exercise had to be done 3x25 times. <ref>Carl G. Mattacola et al, Effects of a 6-week strength hand proprioception training program on measures of dynamic balance: a single-case design, Journal of Athletic Training, 1997 (level of evidence 2B)</ref>(level of evidence 2B) | |||
<br> | |||
The next exercise had to be done in stance. First they had to stand flat floor and then on a balance board. The subjects had to stand on one leg on the floor, first with their eyes open and thereafter with their eyes closed. Each exercise had to be done 3x15 times. After this exercise the subject had to stand with both feet on a balance board or wobble board. They had to make circular movements to train eversion, but also inversion, dorsiflexion and plantar flexion. <br> | The next exercise had to be done in stance. First they had to stand flat floor and then on a balance board. The subjects had to stand on one leg on the floor, first with their eyes open and thereafter with their eyes closed. Each exercise had to be done 3x15 times. After this exercise the subject had to stand with both feet on a balance board or wobble board. They had to make circular movements to train eversion, but also inversion, dorsiflexion and plantar flexion. <br> | ||
Revision as of 14:32, 29 September 2020
Top Contributors - Saumya Srivastava, Mariam Hashem, Venugopal Pawar, Priyanka Chugh, Nicolas D'Hondt and George Prudden
Introduction[edit | edit source]
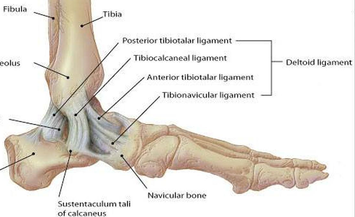
The Deltoid ligament (or the medial ligament of talocrural joint) is a strong, flat and triangular band. It is made up of 4 ligaments that form the triangle, connecting the tibia to the navicular, the calcaneus, and the talus[1] .It is attached above to the apex and anterior and posterior borders of the medial malleolus. The plantar calcaneonavicular ligament can be considered as part of the medial ligament complex.
The Deltoid ligament is composed of superficial and deep components.
The superficial components:
- The tibiocalcaneal ligament descends almost vertically to the entire length of the sustentaculum tali to attach to the calcaneus inferiorly
- The tibionavicular ligament passes forwards to the navicular tuberosity (to attach to it anteriorly [1]) behind which they blend with the medial margin of the plantar calcaneonavicular ligament
- The posterior superficial tibiotalar ligament passes posterolaterally to the medial side of the talus and its medial tubercle
- The tibiospring ligament descends vertically and blends with the fibres of the spring ligament
The deep components:
- The anterior tibiotalar ligament (ATTL) passes from the tip of the medial malleolus to the non-articular part of the medial talar surface. It is crossed by the tendons of the tibialis posterior and flexor digitorum longus
- The posterior deep tibiotalar ligament (PDTL) from the medial malleolus to the talus and is covered by the superficial posterior tibiotalar and tibiocalcaneal ligaments
The anterior and posterior tibiotalar ligaments attach the tibia to the talus [1].
Clinically Relevant Anatomy[edit | edit source]
The deltoid ligament attaches the medial malleolus to multiple tarsal bones. Unlike the superficial layer of this ligament, the deep layer is intraarticular and is covered by synovium. Anatomically, in general, the superficial components arise from the anterior colliculus of the medial malleolus, and the deep components arise from the intercollicular groove (malleolar groove) and the posterior colliculus of the medial malleolus.
The superficial deltoid originates from the anterior & inferior aspects of medial malleolus fanning out & sending 3 bands to navicular and along plantar calcaneonavicular (spring) ligament, to sustenaculum tali of calcaneus and to medial tubercle. It is also partially covered by tendon sheaths & crural fascia. It primarily resists eversion of hindfoot; Tibionavicular portion suspends spring lig & prevents inward displacement of head of talus, while tibiocalcaneal portion prevents valgus displacement.
The deep deltoid originates on posterior border of anterior colliculus, intercollicular groove, & posterior colliculus. It is oriented transversely & inserts into the entire non articular surface of the medial talus. Deep deltoid extends the function of the medial malleolus, prevents lateral displacement and external rotation of the talus (this is mostly significant in plantar flexion, when deep deltoid tends to pull talus into internal rotation).
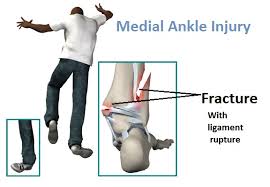
Medial ankle stability is provided by the strong deltoid ligament, the anterior tibiofibular ligament and the bony mortise. Because of the bony articulation between the medial malleolus and the talus, medial ankle sprains are less common than lateral sprains. In medial ankle sprains, the mechanism of injury is excessive eversion and dorsiflexion. [2][3]
Isolated deltoid ligament injuries are extremely rare and usually occur in combination with fractures of the lateral malleolus. These are treated by recognizing the injury complex and stabilizing the lateral side, being sure that the mortise is reduced. [4]
Physical Examination[edit | edit source]
Eversion Test-
In neutral, it evaluates superficial deltoid ligament complex.
External rotation stress test evaluates syndesmotic ligaments and additionally - the deep deltoid ligament;
The test is performed by everting and abducting the heel with one hand, while stabilizing the tibia (and fibula) with the other. Increased laxity or pain indicates a positive test [5].
Radiographic Diagnosis of Injury[edit | edit source]
Deltoid is usually avulsed from tibial attachment, frequently with small flake of bone visible on x-rays;
- disruption of deltoid ligament can be diagnosed with relative confidence when medial clear space between talus & med malleolus is increased;
- lateral shift of talus, with increased medial joint space ( > 3 mm), but this may be apparent only on stress view or in post casting films, after swelling has subsided;
- presence of medial tenderness & > 5 mm of visible space indicates substantial injury to the deltoid ligament;
Treatment of Deltoid Tear[edit | edit source]
- such injuries should be treated as bimalleolar fractures w/ ORIF of lateral malleolus;
- routine exploration of medial side of ankle is not necessary unless there is evidence that portion of deltoid lig has entered joint & is blocking reduction of talus.
Physical Therapy Management[edit | edit source]
To avoid ankle sprains, or ankle instabilities there are rehab exercises which re enforce or retrain the medial ligaments of the ankle. These ligaments are important as they prevent excessive eversion of the ankle (eversion trauma).
First and second degree sprains are typically managed with conservative treatment. In the early stages, the conservative treatment consists of RICE (rest, ice, compress, elevate) and mobilization to prevent range of motion loss. When pain and inflammation are controlled, we can start with therapeutic exercises to increase the range of motion stability, strength proprioception and function.
For third degree sprains, structural damage has most likely occurred mostly needing surgical interventions. After the surgery, the ankle is immobilized. In case there is pain or oedema after immobilization, the first treatment protocol is to attend to the pain and oedema. This will follow the same guidelines same as for the first and second degree sprains conservative management as above.
After two weeks or as and when the pain and swelling allows, strengthening exercises for the medial muscles and ligaments of the ankle can be started. The strengthening programme can be started with low resistance exercises. For example, the patient sits on a chair or massage table with his/her leg extended (log sitting). The physiotherapist stabilises the leg with one hand just below the knee. With the other, the lateral side of the ankle is held. The physiotherapist moves the foot into inversion, and provides some manual resistance. The patient then has to perform eversion movement, against this resistance. The resistance is held for 3 to 5 seconds. The exercise is repeated for 10 to 12 times. [6](level of evidence 2A)
This exercise can also be done without the resistance of a physiotherapist. The patient sits on a chair. An elastic tubing or resistance band is put around the foot, and the other foot is placed on the elastic tubing, while holding the elastic tubing in the contralateral hand. The same exercise as above is performed but with out a therapist, but using the band as the resistance. The patient pushes the foot outward, with the footpad away from the midline of the body.
Proprioceptive exercises can be commenced after 5 weeks.
Exercise for training the proprioception, the double-leg right/left condition, the subjects had to sit on a chair, with their feet on a kinaesthetic ankle board. They had to keep their knees at a 90° angle, while maintaining contact with the top of the KAB with their respective extremities. Then they had to rotate the board to the left side and then back to the right (=clockwise and counter clockwise). The subjects had to keep the side of the board in the floor each time they moved the board to the left or the right. Each exercise had to be done 3x25 times. [7](level of evidence 2B)
The next exercise had to be done in stance. First they had to stand flat floor and then on a balance board. The subjects had to stand on one leg on the floor, first with their eyes open and thereafter with their eyes closed. Each exercise had to be done 3x15 times. After this exercise the subject had to stand with both feet on a balance board or wobble board. They had to make circular movements to train eversion, but also inversion, dorsiflexion and plantar flexion.
The next exercise was the same as the first one, but now the subject had to stand on the balance board. They were instructed to stand on one leg in the middle of the balance board, and then they had to maintain the stance on the balance board. First they had to do it with their eyes open, thereafter with their eyes closed. Each exercise was performed during 30 seconds. [8](level of evidence 2B)
To make these exercises more difficult we could vary the surfaces, on the floor, a balance board, and an instable underground. Another way to increase the difficulty was to open or close the eyes while performing the exercises. The physiotherapist could also increase the exercise by giving light perturbations while the subject balanced on the balance board.
Refrences[edit | edit source]
- ↑ 1.0 1.1 1.2 Manganaro D, Alsayouri K. Anatomy, Bony Pelvis and Lower Limb, Ankle Joint. 2020 Aug 16. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan–. PMID: 31424742.
- ↑ Wolfe MW, Uhl TL, Mattacola CG, McCluskey LC. Management of ankle sprains. Am Fam Physician. 2001 Aug 1;64(3):386. (level of evidence 3A)
- ↑ Wolfe MW, Uhl TL, Mattacola CG, McCluskey LC. Management of ankle sprains. Am Fam Physician. 2001 Aug 1;64(3):386. (level of evidence 3A)fckLRUrl: http://www.aafp.org/afp/2001/0101/afp20010101p93-f4.jpgfckLR Brand RL, Collins MD. Operative management of ligamentous injuries to the ankle. Clin Sports Med. 1982 Mar;1(1):117-30.
- ↑ Brand RL, Collins MD. Operative management of ligamentous injuries to the ankle. Clin Sports Med. 1982 Mar;1(1):117-30.
- ↑ de Vries JS, Kerkhoffs GM, Blankevoort L, van Dijk CN. Clinical evaluation of a dynamic test for lateral ankle ligament laxity. Knee Surg Sports Traumatol Arthrosc. 2010 May;18(5):628-33. doi: 10.1007/s00167-009-0978-7. Epub 2009 Nov 19. PMID: 19924401; PMCID: PMC2855027.
- ↑ Carl G. Mattacola et al, Rehabilitation of the ankle after acute sprain or chronic instability, Journal of Athletic Training, 2002 (level of evidence 2A)
- ↑ Carl G. Mattacola et al, Effects of a 6-week strength hand proprioception training program on measures of dynamic balance: a single-case design, Journal of Athletic Training, 1997 (level of evidence 2B)
- ↑ K. Söderman et al, Balance board training: prevention of traumatic injuries of the lower extremities in female soccer players, Knee Surgery, Sports Traumatology, Arthroscopy, 2000 ((level of evidence 2B)