Introduction to Spinal Orthotics: Difference between revisions
Carin Hunter (talk | contribs) No edit summary |
Kim Jackson (talk | contribs) m (Text replacement - "[[Orthotics" to "[[Introduction to Orthotics") |
||
| (39 intermediate revisions by 5 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> '''Original Editor '''- [[User:Carin Hunter|Carin Hunter]] based on the course by [https://members.physio-pedia.com/course_tutor/donna-fisher/ Donna Fisher]<br> '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> | <div class="editorbox"> '''Original Editor '''- [[User:Carin Hunter|Carin Hunter]] based on the course by [https://members.physio-pedia.com/course_tutor/donna-fisher/ Donna Fisher]<br>'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> | ||
== Introduction == | == Introduction == | ||
In the early days of making orthoses, materials such as metal and leather were predominantly used. However, these materials were heavy, hot and uncomfortable, so materials have been developed and progressed over time. Now, lightweight foams and thermoplastics are used, which facilitates new designs and more comfort for the user. | |||
A spinal orthosis is an external aid that is used to correct and support the spine. The spine is a complex anatomical structure and is key to our function. It is not possible to treat all spinal conditions with orthotics alone. However, a multidisciplinary team approach that includes orthotists, surgeons, and physiotherapists and considers the patient's perspectives can have positive results. A thorough assessment, appropriate goal setting and clear expectations will result in a well-designed and appropriate orthotic device which is comfortable and functional and meets the user's needs.<ref name=":0" /> Unlike other orthotic devices, many spinal braces are off-the-shelf, although certain situations call for a custom-made device.<ref name=":0" /> | |||
== | == Four Principles of Spinal Bracing == | ||
== | ===== Assessment ===== | ||
* Medical diagnosis | |||
* Knowledge of anatomy / physiology | |||
* Subjective assessment | |||
** Medical history | |||
** Social history | |||
** Underlying conditions | |||
** X-ray reports and findings | |||
* Objective assessment | |||
** [[Range of Motion|Range of motion]] | |||
** [[Muscle Strength Testing|Muscle strength]] | |||
** [[Sensation#Sensory Examination|Sensation testing]] | |||
* Determination of which motions should be restricted by the device: | |||
** Sagittal [[Cardinal Planes and Axes of Movement|plane]] | |||
** Frontal / coronal plane | |||
** Transverse plane | |||
** Combination of directional control | |||
* Functional goals of the orthotic device and patient<ref name=":0" /> | |||
===== Aims ===== | |||
* Provides support and stabilisation | |||
* Maintains alignment of spine | |||
* | * Prevention / correction of deformity | ||
* | * Reduce pain by limiting motion | ||
* | * Assist with healing post-surgery | ||
* | * Restriction of motion | ||
* | * Reduction of axial loading of the spine | ||
* Reduction of axial loading of the spine | |||
* Increasing intra-abdominal pressure may reduce axial loading of spine | * Increasing intra-abdominal pressure may reduce axial loading of spine | ||
* May provide heat and kinesthetic feedback | * May provide heat and kinesthetic feedback and act as a reminder for the patient<ref name=":0" /> | ||
== | ===== Manufacturing ===== | ||
* Materials | |||
** Soft fabric | |||
** Flexible plastic | |||
** Polyethylene | |||
** Rigid plastic polypropylene | |||
* Construction | |||
** Off-the-shelf | |||
** Custom made | |||
* Suspension / strapping should be anchored above the iliac crests or over the shoulders | |||
* For cosmetic purposes, the device should be worn under clothing around the trunk<ref name=":0" /> | |||
===== Fitting and Evaluation ===== | |||
* '''Comfort'''. | |||
** Rejection due to discomfort is common as there are high forces applied when applying a spinal brace. This is important for patient compliance and efficacy of the brace. | |||
* '''Good anatomical fit''' | |||
* '''Good biomechanical function.''' | |||
** When assessing function, there may be a requirement for an x-ray both in and out of the brace. | |||
* '''Easy to don / doff''' | |||
* | * '''Cosmesis'''<ref name=":0" /> | ||
* | |||
* | |||
* Good anatomical fit | |||
* Good biomechanical function | |||
* Easy to don/doff | |||
* Cosmesis | |||
== Anatomy == | == Anatomy == | ||
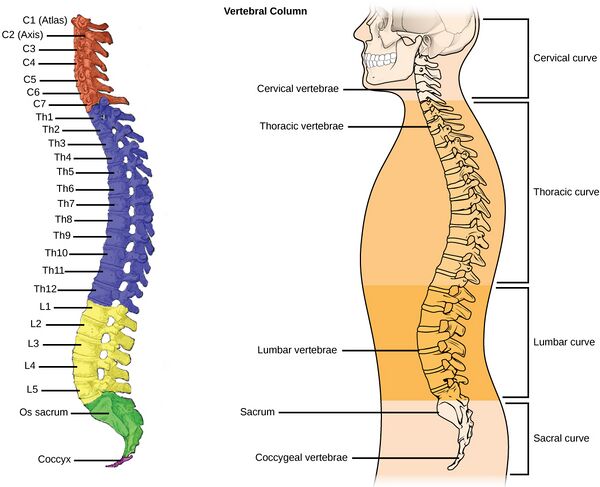
The vertebral column consists of 24 individual bones called vertebrae. The spinal column consists of this vertebral column and | The [[Spinal cord anatomy#Spinal Cord: External|vertebral column]] consists of 24 individual bones called vertebrae. The spinal column consists of this vertebral column and two sections of naturally fused vertebrae, the sacrum and the coccyx, located at the very bottom of the spine. Vertebrae are separated by intravertebral discs, which are fluid-filled cushions between vertebrae.<ref name=":0" /><br />'''The vertebral column can be divided into 5 regions:''' | ||
# Cervical spine: 7 vertebrae of the neck (C1-C7) | # Cervical spine: 7 vertebrae of the neck (C1-C7) | ||
| Line 73: | Line 69: | ||
# Sacrum | # Sacrum | ||
# Coccyx | # Coccyx | ||
[[File:Vertebral Column (1).jpg|thumb|600x600px]] | |||
'''<u>Cervical Region:</u>''' | '''<u>Cervical Region:</u>''' | ||
There are 7 cervical vertebrae | * There are [[Cervical Anatomy#Vertebrae|7 cervical vertebrae]] - two vertebrae are considered atypical: the Atlas and Axis | ||
* Movements: | |||
Cervical flexion/ | ** Cervical flexion / extension – Atlas (nodding) | ||
** Cervical rotation – Axis (shaking head) | |||
Cervical | ** Lateral flexion<ref name=":0" /> | ||
Lateral | |||
'''<u>Thoracic Region:</u>''' | '''<u>Thoracic Region:</u>''' | ||
* There are 12 thoracic vertebrae | * There are [[Thoracic Anatomy#Bones .28vertebrae and ribs.29|12 thoracic vertebrae]] | ||
* | * Movements: | ||
** Rotation | ** Rotation | ||
** Flexion/extension | ** Flexion / extension | ||
** Side / | ** Side / lateral flexion | ||
* | * The thoracic vertebral motion is limited by the facets and ribs | ||
* | ** The largest motion segment is at T12/L1 | ||
*** This is due to the lack of rib stabilisation at this level and because the facets have a more medial to lateral orientation | |||
* Thoracic injuries are often associated with injury, trauma and degenerative changes<ref name=":0" /> | |||
'''<u>Lumbar Region:</u>''' | '''<u>Lumbar Region:</u>''' | ||
* There are 5 lumbar vertebrae: | * There are [[Lumbar Anatomy|5 lumbar vertebrae]] | ||
** Primarily flexion and extension | * Movements: | ||
** | ** Primarily flexion and extension | ||
** Limited rotation | ** Partial lateral flexion | ||
** Limited rotation<ref name=":0" /> | |||
== Common Spinal Disorders == | |||
'''<u>1. Fractures:</u>''' There are three types of [[Fracture|fractures]] that are commonly treated with spinal orthotics: compression, dislocation and compression / dislocation. 5-10% of these occur in the cervical (neck) region while up to 65% occur in the thoracolumbar region, commonly at T12-L1 levels. Common causes include [[osteoporosis]], trauma and tumours.<ref name=":0" /> | |||
'''<u>2. Intravertebral Disc Complications:</u>''' There are many complications associated with the intervertebral disc. Often complications are caused by a prolapsed or [[Disc Herniation|herniated disc]] or are degenerative in nature. Disc degeneration can be due to ageing, trauma, repetitive strains or wear and tear.<ref name=":0" /> | |||
'''<u>3. Spondylolisthesis:</u>''' This is a Latin term which means 'slipped vertebral body'. Typically, the L4 vertebral body slips forward on the L5 vertebral body. Under normal circumstances, the L4-L5 segment is the one in the lumbar spine with the most movement. [[Spondylolisthesis]] in the lumbar spine is most commonly caused by degenerative spinal disease, and is referred to as degenerative spondylolisthesis. It is caused by degeneration of the intervertebral discs and ligaments. [[Spinal Osteoarthritis|Osteoarthritis]] of the facet joints can also contribute to the development of instability and slippage. Degenerative spondylolisthesis usually occurs in people over 60 years of age.<ref name=":0" /> | |||
'''<u>4. Lordosis:</u>''' A lordosis is classified as an excessive convex curvature of the lumbar spine.<ref name=":0" /> | |||
'''<u>5. Kyphosis:</u>''' Kyphosis is characterised by concave curvature of the upper spine (abnormal > 50 degrees of curvature).<ref name=":0" /> | |||
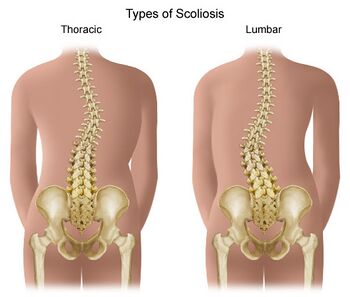
'''<u>6. [[Scoliosis]]:</u>''' More simply known as a lateral bend in the spine. The curve can be S-shaped or C-shaped. The cause can be varied, but is often congenital, degenerative, or due to trauma or tumours. Occasionally they are idiopathic in nature. Scoliosis is discussed in more detail below.<ref name=":0" /> | |||
'''<u>7. Soft Tissue Injuries:</u>''' Soft tissues include the muscles, tendons, ligaments, and nerves. Injury to these tissues can often cause stress on the spine.<ref name=":0" /> | |||
'''<u>8. Sprains / strains:</u>''' A sprain or strain is often due to poor posture or lifting a heavy object, whether it be poor lifting techniques or inadequate strength.<ref name=":0" /> | |||
'''<u>9. Muscle injury:</u>''' These types of injuries are often caused by lifting or sport.<ref name=":0" /> | |||
'''<u>10. Trauma:</u>''' Commonly associated with [[Whiplash Associated Disorders|whiplash]].<ref name=":0" /> | |||
'''<u> | |||
== Types of Spinal Orthoses == | |||
# '''Cervical Orthosis (CO)''' | |||
# '''Cervicothoracic Orthosis (CTO), e.g. HALO, SOMI, Minerva''' | |||
# '''Cervico-Thoraco-Lumbosacral Orthosis (CTLSO), e.g. Milwaukee''' | |||
# '''Thoracolumbosacral Orthosis (TLSO), e.g. CASH, Jewett, custom TLSO''' | |||
# '''Lumbosacral Orthosis (LSO), e.g. Corsets, Chairback O''' | |||
# '''Sacral Orthosis (SO), e.g. Sacro-iliac bands'''<ref name=":0" /> | |||
* | ==== 1. Cervical Orthosis (CO) ==== | ||
* | '''<u>1. Soft Collars</u>'''[[File:Pp.png|thumb|300x300px|alt=]]The most basic collar is a soft cervical collar. It is made using construction foam and coated with cotton wool.<ref>Xu Y, Li X, Chang Y, Wang Y, Che L, Shi G, Niu X, Wang H, Li X, He Y, Pei B. D[https://www.hindawi.com/journals/abb/2022/8243128/ esign of Personalized Cervical Fixation Orthosis Based on 3D Printing Technology]. Applied Bionics and Biomechanics. 2022 Apr 30;2022.</ref> It provides partial support of the head, reducing paraspinal contraction and spasm. While it offers NO structural cervical spine support, it offers proprioceptive input, psychological reassurance and can provide relief through heat retention.<ref name=":0" /> | ||
* Movement limitations:<ref name=":0" /> | |||
** Flexion / extension limited by ~ 8-26% | |||
** Lateral bending is limited by ~8% | |||
** Rotation is limited by ~10-17% | |||
* Assists with:<ref name=":0" /> | |||
** Muscular strains / sprains | |||
** Trauma | |||
'''<u>2. Hard Collars</u>''' | '''<u>2. Hard Collars</u>''' | ||
* | Hard collars are rigid / semirigid and are made of hard foam combined with plastic. The main function of this collar is support.<ref name=":0">Fisher, D. Introduction to Spinal Orthoses Course. Plus. 2022</ref> Hard collars such as the Philadelphia collar may be used initially with unstable fractures until a decision is made regarding treatment. These collars can be used for 6-8 weeks when non-operative treatment is recommended.<ref>Ghosh JC. Review of Management of Type-2 Odontoid [https://www.scirp.org/journal/paperinformation.aspx?paperid=106768 Fracture in Elderly]. Open Journal of Orthopedics. 2021 Jan 11;11(1):12-21.</ref> | ||
* | * Types of hard collars:<ref name=":0" /> | ||
* | ** Miami J Collar | ||
** VISTA Collar | |||
** Aspen | |||
** Headmaster | |||
** Philadelphia | |||
* Movement / function limitations:<ref name=":0" /> | |||
** Flexion / extension limited by ~69-90% | |||
** Lateral bending is limited by ~34-48% | |||
** Rotation is limited by ~74% | |||
* Features:<ref name=":0" /> | |||
** Tracheostomy opening | |||
** Height around chin and occiput can be adjusted | |||
** Due to their construction, most individuals report less sweating than those wearing a soft collar and increased comfort | |||
* Indications:<ref name=":0" /> | |||
** Cervical trauma in unconscious patients | ** Cervical trauma in unconscious patients | ||
** Jefferson’s Fracture (C1) Hangman’s fracture | **[[Jefferson fracture|Jefferson’s Fracture]] (C1), [[Hangman's Fracture|Hangman’s fracture]] | ||
** Traumatic spondylolisthesis of C2 on C3 | ** Traumatic spondylolisthesis of C2 on C3 | ||
** Dens type I fracture | **[[Odontoid fractures|Dens type I fracture]] | ||
** Post | ** Post-operative care | ||
** Anterior discectomy | **[[Anterior cervical discectomy and fusion|Anterior discectomy]] | ||
** Cervical | ** Cervical strain<ref name=":0" /> | ||
==== 2. Cervicothoracic Orthosis (CTO) ==== | ==== 2. Cervicothoracic Orthosis (CTO) ==== | ||
* Types of CTO: | |||
** Halo | |||
** Sterno-occipital mandibular orthosis (SOMI) | |||
** Minerva | |||
* | |||
* | |||
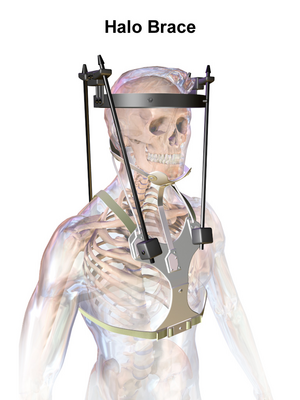
'''<u>1. Halo</u>''' | '''<u>1. Halo</u>''' | ||
* Indications: | A Halo brace is an extensive brace which is surgically applied. It is a 4-post brace that is attached by pins which are placed in the cranial table with a jacket fitted to the torso.<ref name=":0" /> Indications for a halo fixated brace range from: pre-surgical correction to post-operative fusion support. Additionally, a halo brace can be used as an alternative to surgery to conserve neck mobility.<ref>Banat M, Vychopen M, Wach J, Salemdawod A, Scorzin J, Vatter H. [https://link.springer.com/article/10.1007/s00068-021-01849-z Use of halo fixation therapy for traumatic cranio-cervical instability in children: a systematic review]. European Journal of Trauma and Emergency Surgery. 2021 Dec 9:1-7.</ref> The halo brace is more efficacious than a hard collar at limiting motion in the upper cervical spine.<ref>Kumar GR. [https://www.isjonline.com/article.asp?issn=2589-5079;year=2022;volume=5;issue=1;spage=10;epage=23;aulast=Vijay Approach to upper cervical trauma. Indian Spine Journal]. 2022 Jan 1;5(1):10.</ref>[[File:Halo Brace.png|thumb|Halo brace]] | ||
* Movement / function limitations:<ref name=":0" /> | |||
** Flexion / extension limited by 96% | |||
** Lateral bending is limited by 96% | |||
** Rotation is limited by 99% | |||
** It offers maximum motion control to T3 level | |||
* Indications:<ref name=":0" /> | |||
** Occipital condyle fractures | ** Occipital condyle fractures | ||
** C1 ring injuries | ** C1 ring injuries | ||
** Odontoid fractures | ** Odontoid fractures | ||
** Hangman fractures (C2) | ** [[Hangman's Fracture|Hangman's fractures (C2)]] | ||
** | ** Facet subluxations | ||
** | ** Spinal infections | ||
** Extradural | ** Extradural tumour involvement that compromises the spinal alignment or bony stability | ||
** Subaxial spine injuries | ** Subaxial spine injuries<ref name=":0" /> | ||
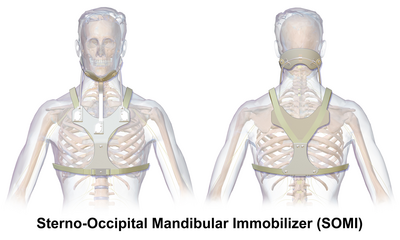
'''<u>2. Sterno- | '''<u>2. Sterno-Occipital Mandibular Orthosis (SOMI)</u>''' | ||
A SOMI is a 3-post, anterior chest plate that extends to the [[Sternum|xiphoid]] process. It has a removeable chin strap.<ref name=":0" /> | |||
[[File:SOMI Brace.png|thumb|400x400px|SOMI brace|alt=]] | |||
* Movement / function limitations:<ref name=":0" /> | |||
** Flexion / extension limited by ~60-70% | |||
** Lateral bending is limited by ~20-35% | |||
** Rotation is limited by ~30-65% | |||
** Offers flexion control of C1-3, but controls extension less than with other cervical orthotics | |||
* | * Indications:<ref name=":0" /> | ||
** Atlanto-axial instability such as in [[Rheumatoid Arthritis|rheumatoid arthritis]] | |||
** | ** Neural arch fractures of C2 due to flexion instability<ref name=":0" /> | ||
** | |||
'''<u>3. Minerva</u>''' | '''<u>3. Minerva</u>''' | ||
* | The Minerva orthosis is a removable version of the Halo. This type of orthosis is offered to compliant patients who will not just remove the brace.<ref name=":0" /> | ||
** Flexion/ | * [[File:Minerva Cervico Thoracic Brace - Ottobock Image.jpg|thumb|Minerva brace]]Movement / function limitations:<ref name=":0" /> | ||
** Lateral | ** Flexion / extension limited by ~96% | ||
** Rotation limited 99% | ** Lateral bending is limited by ~96% | ||
* Indications | ** Rotation is limited by ~99% | ||
** | ** This brace offers control of motion down to T3 level | ||
** | * Indications:<ref name=":0" /> | ||
** Can be used with skull fractures | ** Mid-to-lower cervical spine injuries | ||
** Children due to its decreased weight and increased comfort | ** Stable upper cervical spine injuries | ||
** Can be used with skull fractures when a Halo Fixator is contraindicated | |||
** Children due to its decreased weight and increased comfort<ref name=":0" /> | |||
* | * | ||
==== 3. Cervico- | ==== 3. Cervico-Thoracolumbarsacral Orthosis (CTLSO) ==== | ||
The Milwaukee Brace is the classic CTLSO. It comprises of a metal vertical superstructure that has a pelvic foundation, with a rigid plastic pelvic girdle connected to the neck with a ring. It has two posterior paraspinal bars. The cervical ring has a mandibular and occipital bar which rests 20-30 mm inferior to the chin. The pads are positioned to apply forces in order to correct curvature.<ref name=":0" /> | |||
* | * Indications:<ref name=":0" /> | ||
* | ** Treatment of kyphosis | ||
* | ** Treatment of high thoracic curves | ||
* | |||
==== 4. Thoracolumbosacral Orthosis (TLSO) ==== | |||
* Types of Thoracolumbosacral Orthoses:<ref name=":0" />[[File:TLSO.jpg|thumb|TLSO brace]] | |||
** CASH | |||
** Jewett | |||
** Knight Taylor TLSO | |||
** Custom-molded Spinal/Body Jacket | |||
** Providence Night Brace | |||
** Charleston Bending Brace | |||
* Off-the-shelf (CASH, Jewett, Knight Taylor):<ref name=":0" /> | |||
** Comfortable design | |||
** Easy to don and doff | |||
** Limited movement control | |||
** Flexion from T6-L1 | |||
** No limitation of lateral flexion or rotation | |||
** Indications:<ref name=":0" /> | |||
*** Thoracic and lumbar vertebral body fracture | |||
*** Kyphosis reduction in osteoporosis | |||
*** Cervical trauma in unconscious patients | |||
* Off-the-shelf moulded plastic Spinal Jacket: | |||
** Indications:<ref name=":0" /> | |||
*** Immobilisation for thoracic compression fractures from osteoporosis | |||
*** Immobilisation after surgical stabilisation for spinal fractures | |||
*** Immobilisation for unstable spinal disorders of T3-L3 | |||
* Custom made Spinal Jacket: | |||
** Indications:<ref name=":0" /> | |||
*** Scoliosis | |||
*** Severe spinal abnormalities | |||
*** Night bracing | |||
=== Scoliosis === | |||
[[File:Scoliosis.jpg|thumb|350x350px|scoliosis|alt=]] | |||
* Types of [[scoliosis]]:<ref name=":0" /> | |||
* | ** Neuromuscular scoliosis | ||
** [[Congenital Spine Deformities|Congenital skeletal scoliosis]] | |||
** [[Idiopathic Scoliosis|Idiopathic scoliosis]] | |||
* Indications for bracing in scoliosis:<ref name=":0" /> | |||
** Flexible curves with [[Cobb's angle]] (10°- 40°) | |||
*** 10°- 20° observe initially, if curve progresses by 5° then brace | |||
*** 30°- 40° prompt use of orthosis | |||
*** > 40◦ generally surgery | |||
*** Risser sign for remaining growth | |||
*'''Boston Brace'''<ref name=":0" />[[File:Boston Brace - Donna's Own Image.jpg|thumb|alt=]] | |||
** In the 1970s, this was the most researched and widely used brace | |||
** Module from measurements, type of curve | |||
** Blueprint created from x-rays | |||
** | ** Determine apex of curve and position of pads ([[Foundations for Ankle Foot Orthoses#Three-Point Force System|three-point pressure system]]) | ||
** | |||
** | |||
* Indications for | |||
* | |||
* Boston Brace | |||
** | |||
** Module from | |||
** Blueprint created from x rays | |||
** Determine apex of curve and position of pads ( | |||
** Cut outs to allow body to move | ** Cut outs to allow body to move | ||
** Difficult to control rotation | ** Difficult to control rotation | ||
** Maximum curve 45 degrees below T8 | ** Maximum curve 45 degrees below T8 | ||
** Cheneau Brace | ** ** A symmetrical Boston brace has a consistent success rate of over 70%<ref>Weiss HR, Turnbull D. [https://www.intechopen.com/chapters/71257 Brace treatment for children and adolescents with scoliosis]. InSpinal deformities in adolescents, adults and older adults 2020 Feb 27. IntechOpen.</ref> | ||
* '''Cheneau Brace'''<ref name=":0" />[[File:Cheneau.jpg|thumb|199x199px|Cheneau brace|alt=]] | |||
** Relatively new type, limited research but possibly better results due to rotational control | |||
** Fully custom made | |||
** Type of curve, assessment, x rays | |||
** | ** Pads and cut outs | ||
** Severe looking | |||
** Controls rotation with extensions at the shoulders | |||
[[File:Neuromuscular Scoliosis - Donna's Own Images.jpg|thumb|450x450px|alt=]]Prescription criteria for '''Neuromuscular Scoliosis''':<ref name=":0" /> | |||
*Generally not Boston or Cheneau | |||
* Different aetiology, muscle weakness, underlying condition, severity | |||
* Corrects flexible curves | |||
* Provides stability | |||
* Accommodates fixed deformities | |||
* Can prevent further deformity | |||
==== 5. Lumbo- | ==== 5. Lumbo-Sacral Orthosis (LSO) ==== | ||
[[File:Fabric Lumbosacral Orthosis - Ottobock Image.jpg|thumb|279x279px|alt=]] | |||
Two types of lumbosacral orthoses are prescribed to patients: a soft fabric lumbar support, often constructed with metal or plastic struts to provide support for the lumbar region of the spine; or a moulded plastic Spinal Jacket. These can be off-the-shelf or custom made to suit the patient needs. | |||
Indications: Pain relief | * Indications:<ref name=":0" /> | ||
** Pain relief | |||
** Postural support | |||
** | ** Reduces excessive lumbar lordosis | ||
** | ** Vasomotor and respiratory support in the spinal cord patient | ||
** Increase intra-abdominal pressure | |||
** Heat | |||
** Kinesthetic feedback | |||
==== 6. Sacral Orthosis (SO) ==== | ==== 6. Sacral Orthosis (SO) ==== | ||
[[File:SIJ Belt - Ottobock Image.jpg|thumb|200x200px|alt=]] | |||
* | A sacral orthosis is a fabric, often elasticated support.<ref name=":0" /> | ||
* Indications:<ref name=":0" /> | |||
** Sacro-iliac joint pain | |||
* | * | ||
== | == Resources == | ||
* [[Introduction to Ankle Foot Orthoses]] | |||
* [[Introduction to Complex Orthoses]] | |||
* [[Introduction to Orthotics]] | |||
* [[Milwaukee brace|Milwaukee Brace]] | |||
== References == | |||
[[Category:Course Pages]] | [[Category:Course Pages]] | ||
[[Category: | <references /> | ||
[[Category:ReLAB-HS Course Page]] | |||
[[Category:Rehabilitation]] | |||
Latest revision as of 12:46, 12 December 2022
Top Contributors - Robin Tacchetti, Carin Hunter, Jess Bell, Kim Jackson and Tarina van der Stockt
Introduction[edit | edit source]
In the early days of making orthoses, materials such as metal and leather were predominantly used. However, these materials were heavy, hot and uncomfortable, so materials have been developed and progressed over time. Now, lightweight foams and thermoplastics are used, which facilitates new designs and more comfort for the user.
A spinal orthosis is an external aid that is used to correct and support the spine. The spine is a complex anatomical structure and is key to our function. It is not possible to treat all spinal conditions with orthotics alone. However, a multidisciplinary team approach that includes orthotists, surgeons, and physiotherapists and considers the patient's perspectives can have positive results. A thorough assessment, appropriate goal setting and clear expectations will result in a well-designed and appropriate orthotic device which is comfortable and functional and meets the user's needs.[1] Unlike other orthotic devices, many spinal braces are off-the-shelf, although certain situations call for a custom-made device.[1]
Four Principles of Spinal Bracing[edit | edit source]
Assessment[edit | edit source]
- Medical diagnosis
- Knowledge of anatomy / physiology
- Subjective assessment
- Medical history
- Social history
- Underlying conditions
- X-ray reports and findings
- Objective assessment
- Determination of which motions should be restricted by the device:
- Sagittal plane
- Frontal / coronal plane
- Transverse plane
- Combination of directional control
- Functional goals of the orthotic device and patient[1]
Aims[edit | edit source]
- Provides support and stabilisation
- Maintains alignment of spine
- Prevention / correction of deformity
- Reduce pain by limiting motion
- Assist with healing post-surgery
- Restriction of motion
- Reduction of axial loading of the spine
- Increasing intra-abdominal pressure may reduce axial loading of spine
- May provide heat and kinesthetic feedback and act as a reminder for the patient[1]
Manufacturing[edit | edit source]
- Materials
- Soft fabric
- Flexible plastic
- Polyethylene
- Rigid plastic polypropylene
- Construction
- Off-the-shelf
- Custom made
- Suspension / strapping should be anchored above the iliac crests or over the shoulders
- For cosmetic purposes, the device should be worn under clothing around the trunk[1]
Fitting and Evaluation[edit | edit source]
- Comfort.
- Rejection due to discomfort is common as there are high forces applied when applying a spinal brace. This is important for patient compliance and efficacy of the brace.
- Good anatomical fit
- Good biomechanical function.
- When assessing function, there may be a requirement for an x-ray both in and out of the brace.
- Easy to don / doff
- Cosmesis[1]
Anatomy[edit | edit source]
The vertebral column consists of 24 individual bones called vertebrae. The spinal column consists of this vertebral column and two sections of naturally fused vertebrae, the sacrum and the coccyx, located at the very bottom of the spine. Vertebrae are separated by intravertebral discs, which are fluid-filled cushions between vertebrae.[1]
The vertebral column can be divided into 5 regions:
- Cervical spine: 7 vertebrae of the neck (C1-C7)
- Thoracic spine: 12 vertebrae of the mid-back (T1-T12)
- Lumbar spine: 5 vertebrae of the lower back (L1-L5)
- Sacrum
- Coccyx
Cervical Region:
- There are 7 cervical vertebrae - two vertebrae are considered atypical: the Atlas and Axis
- Movements:
- Cervical flexion / extension – Atlas (nodding)
- Cervical rotation – Axis (shaking head)
- Lateral flexion[1]
Thoracic Region:
- There are 12 thoracic vertebrae
- Movements:
- Rotation
- Flexion / extension
- Side / lateral flexion
- The thoracic vertebral motion is limited by the facets and ribs
- The largest motion segment is at T12/L1
- This is due to the lack of rib stabilisation at this level and because the facets have a more medial to lateral orientation
- The largest motion segment is at T12/L1
- Thoracic injuries are often associated with injury, trauma and degenerative changes[1]
Lumbar Region:
- There are 5 lumbar vertebrae
- Movements:
- Primarily flexion and extension
- Partial lateral flexion
- Limited rotation[1]
Common Spinal Disorders[edit | edit source]
1. Fractures: There are three types of fractures that are commonly treated with spinal orthotics: compression, dislocation and compression / dislocation. 5-10% of these occur in the cervical (neck) region while up to 65% occur in the thoracolumbar region, commonly at T12-L1 levels. Common causes include osteoporosis, trauma and tumours.[1]
2. Intravertebral Disc Complications: There are many complications associated with the intervertebral disc. Often complications are caused by a prolapsed or herniated disc or are degenerative in nature. Disc degeneration can be due to ageing, trauma, repetitive strains or wear and tear.[1]
3. Spondylolisthesis: This is a Latin term which means 'slipped vertebral body'. Typically, the L4 vertebral body slips forward on the L5 vertebral body. Under normal circumstances, the L4-L5 segment is the one in the lumbar spine with the most movement. Spondylolisthesis in the lumbar spine is most commonly caused by degenerative spinal disease, and is referred to as degenerative spondylolisthesis. It is caused by degeneration of the intervertebral discs and ligaments. Osteoarthritis of the facet joints can also contribute to the development of instability and slippage. Degenerative spondylolisthesis usually occurs in people over 60 years of age.[1]
4. Lordosis: A lordosis is classified as an excessive convex curvature of the lumbar spine.[1]
5. Kyphosis: Kyphosis is characterised by concave curvature of the upper spine (abnormal > 50 degrees of curvature).[1]
6. Scoliosis: More simply known as a lateral bend in the spine. The curve can be S-shaped or C-shaped. The cause can be varied, but is often congenital, degenerative, or due to trauma or tumours. Occasionally they are idiopathic in nature. Scoliosis is discussed in more detail below.[1]
7. Soft Tissue Injuries: Soft tissues include the muscles, tendons, ligaments, and nerves. Injury to these tissues can often cause stress on the spine.[1]
8. Sprains / strains: A sprain or strain is often due to poor posture or lifting a heavy object, whether it be poor lifting techniques or inadequate strength.[1]
9. Muscle injury: These types of injuries are often caused by lifting or sport.[1]
10. Trauma: Commonly associated with whiplash.[1]
Types of Spinal Orthoses[edit | edit source]
- Cervical Orthosis (CO)
- Cervicothoracic Orthosis (CTO), e.g. HALO, SOMI, Minerva
- Cervico-Thoraco-Lumbosacral Orthosis (CTLSO), e.g. Milwaukee
- Thoracolumbosacral Orthosis (TLSO), e.g. CASH, Jewett, custom TLSO
- Lumbosacral Orthosis (LSO), e.g. Corsets, Chairback O
- Sacral Orthosis (SO), e.g. Sacro-iliac bands[1]
1. Cervical Orthosis (CO)[edit | edit source]
1. Soft Collars
The most basic collar is a soft cervical collar. It is made using construction foam and coated with cotton wool.[2] It provides partial support of the head, reducing paraspinal contraction and spasm. While it offers NO structural cervical spine support, it offers proprioceptive input, psychological reassurance and can provide relief through heat retention.[1]
- Movement limitations:[1]
- Flexion / extension limited by ~ 8-26%
- Lateral bending is limited by ~8%
- Rotation is limited by ~10-17%
- Assists with:[1]
- Muscular strains / sprains
- Trauma
2. Hard Collars
Hard collars are rigid / semirigid and are made of hard foam combined with plastic. The main function of this collar is support.[1] Hard collars such as the Philadelphia collar may be used initially with unstable fractures until a decision is made regarding treatment. These collars can be used for 6-8 weeks when non-operative treatment is recommended.[3]
- Types of hard collars:[1]
- Miami J Collar
- VISTA Collar
- Aspen
- Headmaster
- Philadelphia
- Movement / function limitations:[1]
- Flexion / extension limited by ~69-90%
- Lateral bending is limited by ~34-48%
- Rotation is limited by ~74%
- Features:[1]
- Tracheostomy opening
- Height around chin and occiput can be adjusted
- Due to their construction, most individuals report less sweating than those wearing a soft collar and increased comfort
- Indications:[1]
- Cervical trauma in unconscious patients
- Jefferson’s Fracture (C1), Hangman’s fracture
- Traumatic spondylolisthesis of C2 on C3
- Dens type I fracture
- Post-operative care
- Anterior discectomy
- Cervical strain[1]
2. Cervicothoracic Orthosis (CTO)[edit | edit source]
- Types of CTO:
- Halo
- Sterno-occipital mandibular orthosis (SOMI)
- Minerva
1. Halo
A Halo brace is an extensive brace which is surgically applied. It is a 4-post brace that is attached by pins which are placed in the cranial table with a jacket fitted to the torso.[1] Indications for a halo fixated brace range from: pre-surgical correction to post-operative fusion support. Additionally, a halo brace can be used as an alternative to surgery to conserve neck mobility.[4] The halo brace is more efficacious than a hard collar at limiting motion in the upper cervical spine.[5]
- Movement / function limitations:[1]
- Flexion / extension limited by 96%
- Lateral bending is limited by 96%
- Rotation is limited by 99%
- It offers maximum motion control to T3 level
- Indications:[1]
- Occipital condyle fractures
- C1 ring injuries
- Odontoid fractures
- Hangman's fractures (C2)
- Facet subluxations
- Spinal infections
- Extradural tumour involvement that compromises the spinal alignment or bony stability
- Subaxial spine injuries[1]
2. Sterno-Occipital Mandibular Orthosis (SOMI)
A SOMI is a 3-post, anterior chest plate that extends to the xiphoid process. It has a removeable chin strap.[1]
- Movement / function limitations:[1]
- Flexion / extension limited by ~60-70%
- Lateral bending is limited by ~20-35%
- Rotation is limited by ~30-65%
- Offers flexion control of C1-3, but controls extension less than with other cervical orthotics
- Indications:[1]
- Atlanto-axial instability such as in rheumatoid arthritis
- Neural arch fractures of C2 due to flexion instability[1]
3. Minerva
The Minerva orthosis is a removable version of the Halo. This type of orthosis is offered to compliant patients who will not just remove the brace.[1]
- Movement / function limitations:[1]
- Flexion / extension limited by ~96%
- Lateral bending is limited by ~96%
- Rotation is limited by ~99%
- This brace offers control of motion down to T3 level
- Indications:[1]
- Mid-to-lower cervical spine injuries
- Stable upper cervical spine injuries
- Can be used with skull fractures when a Halo Fixator is contraindicated
- Children due to its decreased weight and increased comfort[1]
3. Cervico-Thoracolumbarsacral Orthosis (CTLSO)[edit | edit source]
The Milwaukee Brace is the classic CTLSO. It comprises of a metal vertical superstructure that has a pelvic foundation, with a rigid plastic pelvic girdle connected to the neck with a ring. It has two posterior paraspinal bars. The cervical ring has a mandibular and occipital bar which rests 20-30 mm inferior to the chin. The pads are positioned to apply forces in order to correct curvature.[1]
- Indications:[1]
- Treatment of kyphosis
- Treatment of high thoracic curves
4. Thoracolumbosacral Orthosis (TLSO)[edit | edit source]
- Types of Thoracolumbosacral Orthoses:[1]
- CASH
- Jewett
- Knight Taylor TLSO
- Custom-molded Spinal/Body Jacket
- Providence Night Brace
- Charleston Bending Brace
- Off-the-shelf (CASH, Jewett, Knight Taylor):[1]
- Comfortable design
- Easy to don and doff
- Limited movement control
- Flexion from T6-L1
- No limitation of lateral flexion or rotation
- Indications:[1]
- Thoracic and lumbar vertebral body fracture
- Kyphosis reduction in osteoporosis
- Cervical trauma in unconscious patients
- Off-the-shelf moulded plastic Spinal Jacket:
- Indications:[1]
- Immobilisation for thoracic compression fractures from osteoporosis
- Immobilisation after surgical stabilisation for spinal fractures
- Immobilisation for unstable spinal disorders of T3-L3
- Indications:[1]
- Custom made Spinal Jacket:
- Indications:[1]
- Scoliosis
- Severe spinal abnormalities
- Night bracing
- Indications:[1]
Scoliosis[edit | edit source]
- Types of scoliosis:[1]
- Neuromuscular scoliosis
- Congenital skeletal scoliosis
- Idiopathic scoliosis
- Indications for bracing in scoliosis:[1]
- Flexible curves with Cobb's angle (10°- 40°)
- 10°- 20° observe initially, if curve progresses by 5° then brace
- 30°- 40° prompt use of orthosis
- > 40◦ generally surgery
- Risser sign for remaining growth
- Flexible curves with Cobb's angle (10°- 40°)
- Boston Brace[1]
- In the 1970s, this was the most researched and widely used brace
- Module from measurements, type of curve
- Blueprint created from x-rays
- Determine apex of curve and position of pads (three-point pressure system)
- Cut outs to allow body to move
- Difficult to control rotation
- Maximum curve 45 degrees below T8
- ** A symmetrical Boston brace has a consistent success rate of over 70%[6]
- Cheneau Brace[1]
- Relatively new type, limited research but possibly better results due to rotational control
- Fully custom made
- Type of curve, assessment, x rays
- Pads and cut outs
- Severe looking
- Controls rotation with extensions at the shoulders
Prescription criteria for Neuromuscular Scoliosis:[1]
- Generally not Boston or Cheneau
- Different aetiology, muscle weakness, underlying condition, severity
- Corrects flexible curves
- Provides stability
- Accommodates fixed deformities
- Can prevent further deformity
5. Lumbo-Sacral Orthosis (LSO)[edit | edit source]
Two types of lumbosacral orthoses are prescribed to patients: a soft fabric lumbar support, often constructed with metal or plastic struts to provide support for the lumbar region of the spine; or a moulded plastic Spinal Jacket. These can be off-the-shelf or custom made to suit the patient needs.
- Indications:[1]
- Pain relief
- Postural support
- Reduces excessive lumbar lordosis
- Vasomotor and respiratory support in the spinal cord patient
- Increase intra-abdominal pressure
- Heat
- Kinesthetic feedback
6. Sacral Orthosis (SO)[edit | edit source]
A sacral orthosis is a fabric, often elasticated support.[1]
- Indications:[1]
- Sacro-iliac joint pain
Resources[edit | edit source]
- Introduction to Ankle Foot Orthoses
- Introduction to Complex Orthoses
- Introduction to Orthotics
- Milwaukee Brace
References[edit | edit source]
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 1.13 1.14 1.15 1.16 1.17 1.18 1.19 1.20 1.21 1.22 1.23 1.24 1.25 1.26 1.27 1.28 1.29 1.30 1.31 1.32 1.33 1.34 1.35 1.36 1.37 1.38 1.39 1.40 1.41 1.42 1.43 1.44 1.45 1.46 1.47 1.48 1.49 1.50 1.51 1.52 1.53 1.54 1.55 1.56 Fisher, D. Introduction to Spinal Orthoses Course. Plus. 2022
- ↑ Xu Y, Li X, Chang Y, Wang Y, Che L, Shi G, Niu X, Wang H, Li X, He Y, Pei B. Design of Personalized Cervical Fixation Orthosis Based on 3D Printing Technology. Applied Bionics and Biomechanics. 2022 Apr 30;2022.
- ↑ Ghosh JC. Review of Management of Type-2 Odontoid Fracture in Elderly. Open Journal of Orthopedics. 2021 Jan 11;11(1):12-21.
- ↑ Banat M, Vychopen M, Wach J, Salemdawod A, Scorzin J, Vatter H. Use of halo fixation therapy for traumatic cranio-cervical instability in children: a systematic review. European Journal of Trauma and Emergency Surgery. 2021 Dec 9:1-7.
- ↑ Kumar GR. Approach to upper cervical trauma. Indian Spine Journal. 2022 Jan 1;5(1):10.
- ↑ Weiss HR, Turnbull D. Brace treatment for children and adolescents with scoliosis. InSpinal deformities in adolescents, adults and older adults 2020 Feb 27. IntechOpen.