Ewing's Sarcoma: Difference between revisions
No edit summary |
No edit summary |
||
| Line 6: | Line 6: | ||
== Definition/Description == | == Definition/Description == | ||
[[File:Bone 1.jpg|right|299x299px]] | [[File:Bone 1.jpg|right|299x299px]] | ||
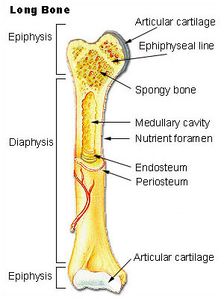
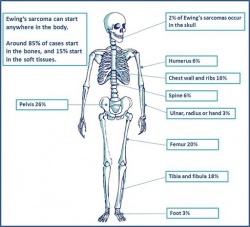
Ewing’s Sarcoma is the second most high grade malignant primary tumour that can arise in soft tissue or bone. The tumour is named after James Ewing who first discovered the small, blue round cell that was distinctly different from osteogenic sarcoma<ref name="p1">Paulussen, Michael. Frohlich, Brigit, Jurgens, Herbert. [https://link.springer.com/article/10.2165%2F00128072-200103120-00003 Ewing Tumour: Incidence, Prognosis, and Treatment Options]. Pediatric Drugs 2001; 3(12); 899-913.(accessed 28 Feb 2011).</ref>. It is often referred to as a family of tumours known as ''Ewing family of tumours (EFT'')<ref name="p1" /><ref name="p2">Goodman, Boissonnault, Fuller. Pathology: Implications for the Physical Therapist. Pennsylvania: Saunders, 2003.</ref><ref name="p3">Medline Plus. Ewing’s Sarcoma. http://www.nlm.nih.gov/medlineplus/ency/article/001302.htm (accessed Feb 2011).</ref> <ref name="p4">Gerrand C, Athanasou N, Brennan B, Grimer R, Judson I, Morland B, Peake D, Seddon B, Whelan J. [https://link.springer.com/article/10.1186/s13569-016-0047-1 UK guidelines for the management of bone sarcomas. Clinical Sarcoma Research]. 2016 Dec 1;6(1):7.</ref>The Ewing family of tumours include Ewing’s Sarcoma, Extraosseous Ewing Sarcoma, Askin's Tumor, and Primitive Neuroectodermal Tumor. Although any [[bone]] can be involved, the most common are the [[pelvis]], [[Hip Anatomy|hip]], [[femur]], [[tibia]] and [[fibula]] <ref name="p5">Elaine Lonnemann’s Powerpoint, [https://soar.usa.edu/dissertations/5/ Oncology. Pathophysiology of Complex Patient Problems]. Bellarmine University 2011.</ref>. Less common sites include the [[ribs]] and vertebral column<ref name="p4" />. The most common sites for secondary tumours include the [[Lung Anatomy|lungs]], bone marrow and other bones; rarely does Ewing’s Sarcoma metastasize to the [[Lymphatic System|lymphatic system]], [[Brain Anatomy|brain]] or liver | Ewing’s Sarcoma is the second most high grade malignant primary tumour that can arise in soft tissue or bone. The tumour is named after James Ewing who first discovered the small, blue round cell that was distinctly different from osteogenic sarcoma<ref name="p1">Paulussen, Michael. Frohlich, Brigit, Jurgens, Herbert. [https://link.springer.com/article/10.2165%2F00128072-200103120-00003 Ewing Tumour: Incidence, Prognosis, and Treatment Options]. Pediatric Drugs 2001; 3(12); 899-913.(accessed 28 Feb 2011).</ref>. It is often referred to as a family of tumours known as ''Ewing family of tumours (EFT'')<ref name="p1" /><ref name="p2">Goodman, Boissonnault, Fuller. Pathology: Implications for the Physical Therapist. Pennsylvania: Saunders, 2003.</ref><ref name="p3">Medline Plus. Ewing’s Sarcoma. http://www.nlm.nih.gov/medlineplus/ency/article/001302.htm (accessed Feb 2011).</ref> <ref name="p4">Gerrand C, Athanasou N, Brennan B, Grimer R, Judson I, Morland B, Peake D, Seddon B, Whelan J. [https://link.springer.com/article/10.1186/s13569-016-0047-1 UK guidelines for the management of bone sarcomas. Clinical Sarcoma Research]. 2016 Dec 1;6(1):7.</ref>The Ewing family of tumours include Ewing’s Sarcoma, Extraosseous Ewing Sarcoma, Askin's Tumor, and Primitive Neuroectodermal Tumor. Although any [[bone]] can be involved, the most common are the [[pelvis]], [[Hip Anatomy|hip]], [[femur]], [[tibia]] and [[fibula]] <ref name="p5">Elaine Lonnemann’s Powerpoint, [https://soar.usa.edu/dissertations/5/ Oncology. Pathophysiology of Complex Patient Problems]. Bellarmine University 2011.</ref>. Less common sites include the [[ribs]] and vertebral column<ref name="p4" />. The most common sites for secondary tumours include the [[Lung Anatomy|lungs]], bone marrow and other bones; rarely does Ewing’s Sarcoma metastasize to the [[Lymphatic System|lymphatic system]], [[Brain Anatomy|brain]] or liver<ref name="p6">[https://www.bcrt.org.uk/information/information-by-type/ewing-sarcoma/ Ewing sarcoma. Bone Cancer Research Trust]. Accessed April 5, 2017.</ref>. It represents 10-15% of malignant bone tumour, and up to 45% for pediatric bone tumours<ref>Ben Kridis W, Toumi N, Chaari H, Khanfir A, Ayadi K, Keskes H, Boudawara T, Daoud J, Frikha M. A review of Ewing sarcoma treatment: is it still a subject of debate?. Reviews on recent clinical trials. 2017 Mar 1;12(1):19-23.</ref>.[[Image:Ewings 1.jpg|250px|Bone Cancer Research Trust|right]] | ||
==== '''Locations''': ==== | ==== '''Locations''': ==== | ||
Lower limbs: 45%(femur most common) | Lower limbs: 45%(femur most common) | ||
| Line 13: | Line 12: | ||
Pelvis: 20% | Pelvis: 20% | ||
Upper limbs: 13% | Upper limbs: 13% | ||
Spine and ribs: 13%(sacrococcygeal) | |||
Skull/face: 2%<ref name="p6" />. | Skull/face: 2%<ref name="p6" />. | ||
== Prevalence == | == Prevalence == | ||
| Line 25: | Line 26: | ||
== Incidence == | == Incidence == | ||
The incidence of Ewing’s Sarcoma has relatively been unchanged for the past 30 years and occurs 2.93 children per 1 million in the United States. Currently, in the United States, the incidence rate is currently nine-fold greater in Caucasian males and females than in African Americans, and intermediate recurrence in Asian Americans<ref name="p0">Ewing’s SarcomaTreatment. National Cancer Institute. https://www.cancer.gov/types/bone/hp/ewing-treatment-pdq#link/_153_toc.</ref>. In the United States about 200-250 from children and adolescent diagnosed with EFT each year. | The incidence of Ewing’s Sarcoma has relatively been unchanged for the past 30 years and occurs 2.93 children per 1 million in the United States. Currently, in the United States, the incidence rate is currently nine-fold greater in Caucasian males and females than in African Americans, and intermediate recurrence in Asian Americans<ref name="p0">Ewing’s SarcomaTreatment. National Cancer Institute. https://www.cancer.gov/types/bone/hp/ewing-treatment-pdq#link/_153_toc.</ref>. In the United States, about 200-250 from children and adolescent diagnosed with EFT each year. | ||
== Prognosis == | == Prognosis == | ||
| Line 44: | Line 45: | ||
== Differential Diagnosis == | == Differential Diagnosis == | ||
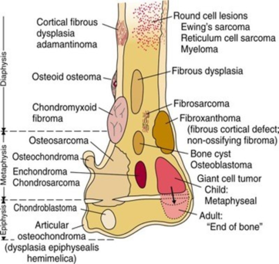
Osteomyelitis and Ewing's Sarcoma may both present with swelling, redness, low-grade fever, and flu-like symptoms. The patient will typically experience intermittent pain with Ewing's Sarcoma versus the constant pain seen with osteomyelitis<ref name="p5" />. The patient may also experience extreme fatigue, weight loss, and loss of appetite with a tumour. Antibiotics will not affect Ewing's Sarcoma but should help with osteomyelitis. X-rays and Lab values are utilized to distinguish Ewing’s Sarcoma and Osteomyelitis. Ewing’s Sarcoma’s symptoms are very general and differential diagnosis of this condition include | [[Osteomyelitis]] and Ewing's Sarcoma may both present with swelling, redness, low-grade fever, and flu-like symptoms. The patient will typically experience intermittent pain with Ewing's Sarcoma versus the constant pain seen with osteomyelitis<ref name="p5" />. The patient may also experience extreme fatigue, weight loss, and loss of appetite with a tumour. [[Antimicrobial Resistance|Antibiotics]] will not affect Ewing's Sarcoma but should help with osteomyelitis. [[X-Rays|X-rays]] and Lab values are utilized to distinguish Ewing’s Sarcoma and Osteomyelitis. | ||
[[Osteosarcoma]], most common bone cancer about 60% of cases presented in children and adolescent, long bones of arm and leg are most affected. Its symptoms according to the location of the lesion. | |||
Eosinophilic granuloma, it is one of the rare disorders known as Langerhans cell histiocytosis (LCH). There is overproduction and accumulation of histiocytes in different organs, associated with bone pain, swelling of adjacent tissue, and/or osteolysis, in some cases, it may be asymptomatic<ref>https://rarediseases.org/rare-diseases/langerhans-cell-histiocytosis/</ref>. | |||
Ewing’s Sarcoma’s symptoms are very general and differential diagnosis of this condition include [[tendinopathy]], [[Osgood-Schlatter's Disease|Osgood Schlatter's disease]], trauma, and slipped epiphysis of a long bone<ref name="p6" />. | |||
Review an excellent Presentation on Ewings Sarcoma by Jen Son and Gillian Lieberman MD | |||
<span>http://eutils.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=1VsHRGSo3HX0CgCh0yQTDe7FwEqMdcz0ZoLhJtVqvvv0fjjM7M|charset=UTF-8|short|max=10</span> | <span>http://eutils.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=1VsHRGSo3HX0CgCh0yQTDe7FwEqMdcz0ZoLhJtVqvvv0fjjM7M|charset=UTF-8|short|max=10</span> | ||
| Line 53: | Line 62: | ||
== Diagnostic Tests/Lab Tests/Lab Values == | == Diagnostic Tests/Lab Tests/Lab Values == | ||
The diagnosing Ewing’s Sarcoma depends on full patient history, symptoms, clinical presentation and diagnostic methods as following, the first test most commonly used is X-Ray over the painful area if there is a palpable mass. Other tests that may be performed to rule in Ewing’s Sarcoma and determine staging are bone scans, [[CT Scans|CT scans]], [[MRI Scans|MRI]], [[Blood Tests|blood tests]] (elevated lactate dehydrogenase and red blood cell sedimentation rate) and biopsy for bone marrow, for example, to know whether it spreads to bone marrow or not. These tests in combination are important to find the location of the tumour and to determine if the tumour is localized or has diffused to other areas of the body to help guide treatment. the Biopsy is considered the gold standard test for diagnosis of Ewing’s Sarcoma.<ref name="p1" /><ref name="p5" /><ref name="p4" /> | |||
[[Image:Ewings 6.jpg|left]][[Image:Ewings 7.jpg|263x263px]] | [[Image:Ewings 6.jpg|left]][[Image:Ewings 7.jpg|263x263px]] | ||
== Medical Management (current best evidence) == | == Medical Management (current best evidence) == | ||
Depending upon the location of the tumour and metastases, doctors in many specialities help treat EFT. Medical management is considered a multidisciplinary effort which includes orthopaedic surgical oncologists, pediatric or adult medical oncologists, radiation oncologists, pathologists, and radiologists. Most patients are treated at major hospital institutions or cancer centres.<ref name="p4" /><ref name="p1" /> | Depending upon the location of the tumour and metastases, doctors in many specialities help treat EFT. Medical management is considered a multidisciplinary effort which includes orthopaedic surgical oncologists, pediatric or adult medical oncologists, radiation oncologists, pathologists, and radiologists. Most patients are treated at major hospital institutions or cancer centres.<ref>Bouaoud J, Temam S, Cozic N, Galmiche‐Rolland L, Belhous K, Kolb F, Bidault F, Bolle S, Dumont S, Laurence V, Plantaz D. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6308064/#cam41801-bib-0005 Ewing’s Sarcoma of the Head and Neck]: Margins are not just for surgeons. Cancer medicine. 2018 Dec;7(12):5879-88.</ref><ref name="p4" /><ref name="p1" /><ref name="p2" /><br>The first line of recommended treatment is chemotherapy, also referred to as cytostatic drug therapy, which is given through an indwelling intravenous catheter. Chemotherapy medications most commonly used are vincristine (Oncovin), dactinomycin (Actinomycin D), cyclophosphamide (Cytoxan), ifosfamide (Ifex), etoposide (VePeside, VP-16), and doxorubicin (Adriamycin)<ref name="p1" /><ref name="p9">Karosas AO. [https://academic.oup.com/ajhp/article-abstract/67/19/1599/5130749?redirectedFrom=PDF#133506114 Ewing’s sarcoma]. American Journal of Health-System Pharmacy. 2010 Oct 1;67(19):1599-605.</ref><ref name="p2" />Chemotherapy treatment is typically performed in cycles to let the blood cell count recover. The second line of treatment, which can be done before or during chemotherapy, is a local treatment. Local treatment includes radiation and/or surgery. Surgery is used to treat localized tumour when the tumour is easily assessable. When the localized tumour is not assessable as in the pelvis or spine, surgery is not an option and radiation is used to treat the localized tumour. A detrimental side effect that can result from radiation is structural deformities in children. Surgery can also be performed to rebuild a body part or limb. As the child grows, reconstruction therapy will be necessary to lengthen the bone.<ref name="p4" /><ref name="p1" /><ref name="p2" /><br>Follow up intervals of 2-4 months for the first 3 years after completion of therapy is recommended for high-grade tumours such as EFT. Follow up every 6 months for year 4 and 5 and annually after that<ref name="p4" />. Due to the recent availability of multi-agent cytostatic approaches and local therapy, the 5-year survival rate has increased from 10% to 70%<ref name="p1" /><ref name="p8">Goodman C, Snyder T. Differential Diagnosis for Physical Therapists: Screening for Referral. St. Louis, MO: Saunders Elsevier: 2007</ref>.<br>Immunological approaches, such as the use of cytokines (interleukins, and interferon), are still being researched.<ref name="p7">Burningham Z, Hashibe M, Spector L, Schiffman JD. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3564705/ The epidemiology of sarcoma]. Clinical sarcoma research. 2012 Dec 1;2(1):14.</ref><ref>Yu H, Ge Y, Guo L, Huang L. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5354928/ Potential approaches to the treatment of Ewing's sarcoma]. Oncotarget. 2017 Jan 17;8(3):5523.</ref> | ||
== Physical Therapy Management (current best evidence) == | == Physical Therapy Management (current best evidence) == | ||
Physical therapy (PT) can be beneficial for those diagnosed with EFT for many reasons and at different stages during the management process. The most common limitations for patients undergoing chemotherapy include fatigue, paralysis, or weakness, cognition, and weight loss/ gain <ref name="p5" /><br>Pre-operative PT is beneficial when feasible. Plan of care should include strengthening of the affected limb and aerobic conditioning (precaution: avoid weight bearing on an extremity or placing weight distal to the extremity in which tumour is located).<ref name="p6" /><br>Post-operative PT is essential but caution must be taken because of the impaired healing process due to chemotherapy. Precautions include: stretching the skin in the area of the incision, weight-bearing status and lab values (especially platelet count). Some general guidelines include aerobic conditioning, strengthening, continuous passive range of motion, and aquatic therapy<ref name="p6" />.<br>If amputation is done, it may take the child several months to learn to use a prosthetic leg or arm. A physical therapist will be able to assist in fitting and donning the prosthesis, teaching the child how to use it, and how to use necessary assistive devices. Children may also have a tissue graft, which the child needs to start moving almost immediately. Physical therapy and rehabilitation is typically recommended for six to twelve weeks post operation<ref name="p2" />. | Physical therapy (PT) can be beneficial for those diagnosed with EFT for many reasons and at different stages during the management process. The most common limitations for patients undergoing chemotherapy include fatigue, paralysis, or weakness, cognition, and weight loss/ gain <ref name="p5" /><br>Pre-operative PT is beneficial when feasible. Plan of care should include strengthening of the affected limb and aerobic conditioning (precaution: avoid weight bearing on an extremity or placing weight distal to the extremity in which tumour is located).<ref name="p6" /><br>Post-operative PT is essential but caution must be taken because of the impaired healing process due to chemotherapy. Precautions include: stretching the skin in the area of the incision, weight-bearing status and lab values (especially platelet count). Some general guidelines include aerobic conditioning, strengthening, continuous passive range of motion, and aquatic therapy<ref name="p6" />.<br>If amputation is done, it may take the child several months to learn to use a prosthetic leg or arm. A physical therapist will be able to assist in fitting and donning the prosthesis, teaching the child how to use it, and how to use necessary assistive devices. Children may also have a tissue graft, which the child needs to start moving almost immediately. Physical therapy and rehabilitation is typically recommended for six to twelve weeks post operation<ref name="p2" />.<br><span style="line-height: 1.5em;"> </span><span style="line-height: 1.5em;"> </span> | ||
{{#ev:youtube|FRcrAieE_TA}}<ref>Joseph Dorrell. Physiopedia Ewing's Sarcoma PT Management. Available from: http://www.youtube.com/watch?v=FRcrAieE_TA[last accessed 25/7/2020]</ref> | {{#ev:youtube|FRcrAieE_TA}}<ref>Joseph Dorrell. Physiopedia Ewing's Sarcoma PT Management. Available from: http://www.youtube.com/watch?v=FRcrAieE_TA[last accessed 25/7/2020]</ref> | ||
| Line 69: | Line 78: | ||
'''Keywords''' | '''Keywords''' | ||
Fatigue, treatment, fever, bone pain, cancer, therapy, symptoms | Fatigue, treatment, fever, bone pain, cancer, therapy, symptoms<br> '''Authors''' | ||
<br> ''' | Jack Tencza and Joseph Dorrell<br> '''Abstract''' | ||
Ewing’s Sarcoma is the 2nd most commonly diagnosed form of primary bone cancer in children and young adults. In this example, a case study of an 18 year old Caucasian female gymnast is examined to help health care professionals identify a possible clinical case of Ewing’s Sarcoma.<br> '''Introduction''' | |||
Ewing’s Sarcoma is the 2nd most commonly diagnosed form of primary bone cancer in children and young adults. In this example, a case study of an 18 year old Caucasian female gymnast is examined to help health care professionals identify a possible clinical case of Ewing’s Sarcoma. | |||
<br> '''Introduction''' | |||
Ewing’s Sarcoma family of tumours are a group of small round cell tumours that include Ewing’s Sarcoma, Extraosseous Ewing Sarcoma, Askin Tumor, and Primitive Neuroectodermal Tumor. This cancer primarily affects children and adolescents, and most often affects soft tissue and bone. The most common sites for Ewing’s Sarcoma is the pelvis, hip, femur, tibia and fibula. | Ewing’s Sarcoma family of tumours are a group of small round cell tumours that include Ewing’s Sarcoma, Extraosseous Ewing Sarcoma, Askin Tumor, and Primitive Neuroectodermal Tumor. This cancer primarily affects children and adolescents, and most often affects soft tissue and bone. The most common sites for Ewing’s Sarcoma is the pelvis, hip, femur, tibia and fibula. | ||
| Line 85: | Line 88: | ||
== Case Presentation == | == Case Presentation == | ||
<u>Subjective :</u> | <u>Subjective :</u><br><u>Patient History:</u> Pt. is an 18-year old Caucasian female who reports with a recent history of right hip pain of 5/10 during the day and 7/10 at night. She reports limping from a cartwheel at gymnastics 2 months ago. She reports that she has had night sweats with intermittent fever and general fatigue during the day. Pt. reports that she has had a recent physical examination 5 months ago with her GP who found that she was underweight. GP states this could be possibly due to female athlete triad. She notes that she has been more attentive with her diet and exercise since then. Pt. states her goal is to return to gymnastics pain-free and as soon as possible. | ||
<br><u>Patient History:</u> Pt. is an 18-year old Caucasian female who reports with a recent history of right hip pain of 5/10 during the day and 7/10 at night. She reports limping from a cartwheel at gymnastics 2 months ago. She reports that she has had night sweats with intermittent fever and general fatigue during the day. Pt. reports that she has had a recent physical examination 5 months ago with her GP who found that she was underweight. GP states this could be possibly due to female athlete triad. She notes that she has been more attentive with her diet and exercise since then. Pt. states her goal is to return to gymnastics pain-free and as soon as possible. | |||
<br><u>Objective-: </u>Physical Examination Tests and Measures | <u>Medical History:</u> Unremarkable<br><u>Objective-: </u>Physical Examination Tests and Measures | ||
<u>Observation/ Palpation:</u> Pt. has to pinpoint tenderness around R ASIS, and notes pain with R weight shifting<br><u>Lumbar ROM</u><br>Lumbar Flexion 65<br>Lumbar Extension 35<br>Lumbar Side bend 20<br>Lumbar Rotation 30 | |||
<br><u>Lumbar ROM</u><br>Lumbar Flexion 65<br>Lumbar Extension 35<br>Lumbar | |||
<u>Hip ROM Right Left</u><br>Hip Flexion 85 130<br>Hip Extension 15 30<br>Hip IR 20 40<br>Hip ER 25 40<br>Hip ABD 25 45 | <u>Hip ROM Right Left</u><br>Hip Flexion 85 130<br>Hip Extension 15 30<br>Hip IR 20 40<br>Hip ER 25 40<br>Hip ABD 25 45 | ||
| Line 101: | Line 98: | ||
<u>MMT</u><br>L Hip 5/5 in all planes<br>R Hip 4/5 in all planes (pain)<br>UE ROM: WNL<br>UE MMT: WNL | <u>MMT</u><br>L Hip 5/5 in all planes<br>R Hip 4/5 in all planes (pain)<br>UE ROM: WNL<br>UE MMT: WNL | ||
<br><u>Neurovascular:</u> decreased sensation along R lateral thigh | <br><u>Neurovascular:</u> decreased sensation along R lateral thigh<br><u>Special Tests:</u><br>FABER - Negative<br>Scour Test - Positive<br>Anterior Labral Tear - Negative<br>Impingement Test - Positive | ||
<br><u>Special Tests:</u><br>FABER - Negative<br>Scour Test - Positive<br>Anterior Labral Tear - Negative<br>Impingement Test - Positive | |||
'''Clinical Impression''' | '''Clinical Impression''' | ||
| Line 111: | Line 106: | ||
'''Intervention''' | '''Intervention''' | ||
Hip AROM/ PROM exercises<br>Standing hip flexion, extension, abduction, IR and ER resistance exercises<br>Wall slides & standing squats<br>Hip long axis traction | Hip AROM/ PROM exercises<br>Standing hip flexion, extension, abduction, IR and ER resistance exercises<br>Wall slides & standing squats<br>Hip long axis traction<br> | ||
'''Outcomes''' | |||
Over a period of 5 visits, pt’s s/s did not improve. the Pain intensified to a 7/10 during the day and an 8/10 at night. PT then determined that pt needed to be referred out for imaging of the hip. Pt went to MD and received X-Ray which indicated a possible tumour of the pelvis. Blood tests indicated elevated lactate dehydrogenase and red blood cell sedimentation rate. MD referred to Oncologist for a biopsy which confirmed an Ewing’s Sarcoma of the pelvis. Pt received chemotherapy and radiation. | Over a period of 5 visits, pt’s s/s did not improve. the Pain intensified to a 7/10 during the day and an 8/10 at night. PT then determined that pt needed to be referred out for imaging of the hip. Pt went to MD and received X-Ray which indicated a possible tumour of the pelvis. Blood tests indicated elevated lactate dehydrogenase and red blood cell sedimentation rate. MD referred to Oncologist for a biopsy which confirmed an Ewing’s Sarcoma of the pelvis. Pt received chemotherapy and radiation. | ||
Revision as of 01:34, 27 July 2020
Original Editors - from Bellarmine University's Pathophysiology of Complex Patient Problems project.
Top Contributors - Joseph Dorrell, Lisa Miville, Elaine Lonnemann, Nikhil Benhur Abburi, Lucinda hampton, Jack Tencza, Tessa Larimer, Admin, Vidya Acharya, Khloud Shreif, Kim Jackson, WikiSysop, Claire Knott, 127.0.0.1 and Wendy Walker
Definition/Description[edit | edit source]
Ewing’s Sarcoma is the second most high grade malignant primary tumour that can arise in soft tissue or bone. The tumour is named after James Ewing who first discovered the small, blue round cell that was distinctly different from osteogenic sarcoma[1]. It is often referred to as a family of tumours known as Ewing family of tumours (EFT)[1][2][3] [4]The Ewing family of tumours include Ewing’s Sarcoma, Extraosseous Ewing Sarcoma, Askin's Tumor, and Primitive Neuroectodermal Tumor. Although any bone can be involved, the most common are the pelvis, hip, femur, tibia and fibula [5]. Less common sites include the ribs and vertebral column[4]. The most common sites for secondary tumours include the lungs, bone marrow and other bones; rarely does Ewing’s Sarcoma metastasize to the lymphatic system, brain or liver[6]. It represents 10-15% of malignant bone tumour, and up to 45% for pediatric bone tumours[7].
Locations:[edit | edit source]
Lower limbs: 45%(femur most common)
Pelvis: 20%
Upper limbs: 13%
Spine and ribs: 13%(sacrococcygeal)
Skull/face: 2%[6].
Prevalence[edit | edit source]
Ewing’s Sarcoma primarily affects Caucasians, whereas Asian and African populations are considerably less affected.[8] Rates of Ewing’s Sarcoma are found to be higher in North America as compared to Europe or Asia. The rate of prevalence between males and females is not significantly different. Ewing’s Sarcoma is not currently related to any gene mutations or hereditary cancer syndromes. However, relationships between race and inherited familial risk suggest a possible association[8]. Ewing's Sarcoma is the second most common primary malignant bone tumour of children and the fourth most common overall. 80% of these tumours occur in people under the age of 20. EFT is most common in children between the ages of 10 and 20. Factors include a tall stature or experiencing a premature growth spurt from puberty. In adults risk factors such as infection, radiation, and occupation increase the risk of development of Ewing’s Sarcoma.[8]
- Youngest reported case of EFT - 5 months old
- Oldest reported case 77-year-old female
- More common in males than females 1.5:1[1] [2][3][4][9][10]
Incidence[edit | edit source]
The incidence of Ewing’s Sarcoma has relatively been unchanged for the past 30 years and occurs 2.93 children per 1 million in the United States. Currently, in the United States, the incidence rate is currently nine-fold greater in Caucasian males and females than in African Americans, and intermediate recurrence in Asian Americans[11]. In the United States, about 200-250 from children and adolescent diagnosed with EFT each year.
Prognosis[edit | edit source]
Ewing’s sarcoma is typically cured 70% of the time in the early stages of metastasis. Teenagers in the range of 15-19 have a lower survival rate of 56%.[1] After the disease has spread, children have a survival rate of less than 30%.[1]
Etiology/Causes[edit | edit source]
It has been found that 95% of Ewing's tumours are derived from a specific reciprocal translocation between chromosomes 11 and 22. The molecular oncogenesis remains unknown[2][1]. In rare cases, it may develop as a secondary malignancy, that meanes a complication of a treatment of another type of cancer.
Characteristics/Clinical Presentation[edit | edit source]
Local pain at the affected site is usually the initial symptom[1]. The pain may be worse during exercise or at night and can be accompanied by swelling or a lump, redness, and warmth (see in this picture swelling of the left side)[3]. The pain is typically intermittent and ma progress to be more consistent.[5] Tumours that are deep inside the body such as the pelvis can be hidden from observation and inspection.
It is common to see fatigue, weight loss, decreased appetite, weakness and numbness, and/or paralysis or incontinence (if the tumour is of spinal origin)[4]. Fever, anaemia, and leukocytosis may occur with this tumour and a palpable mass may present. The tumour may be present for months before there are any signs or symptoms. Symptoms can vary from patient to patient in terms of severity and can disappear from weeks to months at a time[6]. An injury is often what brings attention to the tumour, this is due to progressive structural bone-weakening by the disease, which can result in a fracture with minimal force. Children and adolescents with EFT can go undiagnosed until an injury from a sport or rough play requires diagnostic imaging[2].
As a physical therapist, one should be cautious when the symptoms of "growing pains" or a proposed sports injury are out of proportion or abnormal.
Radiographic features[edit | edit source]
Poorly marginated large tumours extending into adjacent soft tissues, appearance on plain radiographs is very variable, but have clearly aggressive appearance. they are permeative, have an onionskin appearance. so tissue calcification is uncommon, seen in less than 10% of cases
Differential Diagnosis[edit | edit source]
Osteomyelitis and Ewing's Sarcoma may both present with swelling, redness, low-grade fever, and flu-like symptoms. The patient will typically experience intermittent pain with Ewing's Sarcoma versus the constant pain seen with osteomyelitis[5]. The patient may also experience extreme fatigue, weight loss, and loss of appetite with a tumour. Antibiotics will not affect Ewing's Sarcoma but should help with osteomyelitis. X-rays and Lab values are utilized to distinguish Ewing’s Sarcoma and Osteomyelitis.
Osteosarcoma, most common bone cancer about 60% of cases presented in children and adolescent, long bones of arm and leg are most affected. Its symptoms according to the location of the lesion.
Eosinophilic granuloma, it is one of the rare disorders known as Langerhans cell histiocytosis (LCH). There is overproduction and accumulation of histiocytes in different organs, associated with bone pain, swelling of adjacent tissue, and/or osteolysis, in some cases, it may be asymptomatic[12].
Ewing’s Sarcoma’s symptoms are very general and differential diagnosis of this condition include tendinopathy, Osgood Schlatter's disease, trauma, and slipped epiphysis of a long bone[6].
Review an excellent Presentation on Ewings Sarcoma by Jen Son and Gillian Lieberman MD
Systemic Involvement[edit | edit source]
Ewing's Family of Tumors are highly malignant. It most commonly spreads to the lungs, but it can also metastasize to the kidney, bone marrow, heart, adrenal gland, and other soft tissues[4]. Chemotherapy and radiation, which are most commonly used to treat EFT, have many systemic side effects including hair loss, nausea, vomiting, ulcers, and low blood cell count.[4]
Diagnostic Tests/Lab Tests/Lab Values[edit | edit source]
The diagnosing Ewing’s Sarcoma depends on full patient history, symptoms, clinical presentation and diagnostic methods as following, the first test most commonly used is X-Ray over the painful area if there is a palpable mass. Other tests that may be performed to rule in Ewing’s Sarcoma and determine staging are bone scans, CT scans, MRI, blood tests (elevated lactate dehydrogenase and red blood cell sedimentation rate) and biopsy for bone marrow, for example, to know whether it spreads to bone marrow or not. These tests in combination are important to find the location of the tumour and to determine if the tumour is localized or has diffused to other areas of the body to help guide treatment. the Biopsy is considered the gold standard test for diagnosis of Ewing’s Sarcoma.[1][5][4]
Medical Management (current best evidence)[edit | edit source]
Depending upon the location of the tumour and metastases, doctors in many specialities help treat EFT. Medical management is considered a multidisciplinary effort which includes orthopaedic surgical oncologists, pediatric or adult medical oncologists, radiation oncologists, pathologists, and radiologists. Most patients are treated at major hospital institutions or cancer centres.[13][4][1][2]
The first line of recommended treatment is chemotherapy, also referred to as cytostatic drug therapy, which is given through an indwelling intravenous catheter. Chemotherapy medications most commonly used are vincristine (Oncovin), dactinomycin (Actinomycin D), cyclophosphamide (Cytoxan), ifosfamide (Ifex), etoposide (VePeside, VP-16), and doxorubicin (Adriamycin)[1][10][2]Chemotherapy treatment is typically performed in cycles to let the blood cell count recover. The second line of treatment, which can be done before or during chemotherapy, is a local treatment. Local treatment includes radiation and/or surgery. Surgery is used to treat localized tumour when the tumour is easily assessable. When the localized tumour is not assessable as in the pelvis or spine, surgery is not an option and radiation is used to treat the localized tumour. A detrimental side effect that can result from radiation is structural deformities in children. Surgery can also be performed to rebuild a body part or limb. As the child grows, reconstruction therapy will be necessary to lengthen the bone.[4][1][2]
Follow up intervals of 2-4 months for the first 3 years after completion of therapy is recommended for high-grade tumours such as EFT. Follow up every 6 months for year 4 and 5 and annually after that[4]. Due to the recent availability of multi-agent cytostatic approaches and local therapy, the 5-year survival rate has increased from 10% to 70%[1][9].
Immunological approaches, such as the use of cytokines (interleukins, and interferon), are still being researched.[8][14]
Physical Therapy Management (current best evidence)[edit | edit source]
Physical therapy (PT) can be beneficial for those diagnosed with EFT for many reasons and at different stages during the management process. The most common limitations for patients undergoing chemotherapy include fatigue, paralysis, or weakness, cognition, and weight loss/ gain [5]
Pre-operative PT is beneficial when feasible. Plan of care should include strengthening of the affected limb and aerobic conditioning (precaution: avoid weight bearing on an extremity or placing weight distal to the extremity in which tumour is located).[6]
Post-operative PT is essential but caution must be taken because of the impaired healing process due to chemotherapy. Precautions include: stretching the skin in the area of the incision, weight-bearing status and lab values (especially platelet count). Some general guidelines include aerobic conditioning, strengthening, continuous passive range of motion, and aquatic therapy[6].
If amputation is done, it may take the child several months to learn to use a prosthetic leg or arm. A physical therapist will be able to assist in fitting and donning the prosthesis, teaching the child how to use it, and how to use necessary assistive devices. Children may also have a tissue graft, which the child needs to start moving almost immediately. Physical therapy and rehabilitation is typically recommended for six to twelve weeks post operation[2].
Ewing’s Sarcoma Case Study[edit | edit source]
Keywords
Fatigue, treatment, fever, bone pain, cancer, therapy, symptoms
Authors
Jack Tencza and Joseph Dorrell
Abstract
Ewing’s Sarcoma is the 2nd most commonly diagnosed form of primary bone cancer in children and young adults. In this example, a case study of an 18 year old Caucasian female gymnast is examined to help health care professionals identify a possible clinical case of Ewing’s Sarcoma.
Introduction
Ewing’s Sarcoma family of tumours are a group of small round cell tumours that include Ewing’s Sarcoma, Extraosseous Ewing Sarcoma, Askin Tumor, and Primitive Neuroectodermal Tumor. This cancer primarily affects children and adolescents, and most often affects soft tissue and bone. The most common sites for Ewing’s Sarcoma is the pelvis, hip, femur, tibia and fibula.
Case Presentation[edit | edit source]
Subjective :
Patient History: Pt. is an 18-year old Caucasian female who reports with a recent history of right hip pain of 5/10 during the day and 7/10 at night. She reports limping from a cartwheel at gymnastics 2 months ago. She reports that she has had night sweats with intermittent fever and general fatigue during the day. Pt. reports that she has had a recent physical examination 5 months ago with her GP who found that she was underweight. GP states this could be possibly due to female athlete triad. She notes that she has been more attentive with her diet and exercise since then. Pt. states her goal is to return to gymnastics pain-free and as soon as possible.
Medical History: Unremarkable
Objective-: Physical Examination Tests and Measures
Observation/ Palpation: Pt. has to pinpoint tenderness around R ASIS, and notes pain with R weight shifting
Lumbar ROM
Lumbar Flexion 65
Lumbar Extension 35
Lumbar Side bend 20
Lumbar Rotation 30
Hip ROM Right Left
Hip Flexion 85 130
Hip Extension 15 30
Hip IR 20 40
Hip ER 25 40
Hip ABD 25 45
MMT
L Hip 5/5 in all planes
R Hip 4/5 in all planes (pain)
UE ROM: WNL
UE MMT: WNL
Neurovascular: decreased sensation along R lateral thigh
Special Tests:
FABER - Negative
Scour Test - Positive
Anterior Labral Tear - Negative
Impingement Test - Positive
Clinical Impression
Examination findings show decreased ROM and weakness of the R hip with palpable pinpoint pain, tenderness, and warmth. No other musculoskeletal abnormalities found to be present. Working diagnosis of female athlete triad and hip impingement. Targeted interventions include strengthening the R hip musculature, improving R hip ROM in all planes, manual therapy to decrease pain and improve function, and modalities for pain relief.
Intervention
Hip AROM/ PROM exercises
Standing hip flexion, extension, abduction, IR and ER resistance exercises
Wall slides & standing squats
Hip long axis traction
Outcomes
Over a period of 5 visits, pt’s s/s did not improve. the Pain intensified to a 7/10 during the day and an 8/10 at night. PT then determined that pt needed to be referred out for imaging of the hip. Pt went to MD and received X-Ray which indicated a possible tumour of the pelvis. Blood tests indicated elevated lactate dehydrogenase and red blood cell sedimentation rate. MD referred to Oncologist for a biopsy which confirmed an Ewing’s Sarcoma of the pelvis. Pt received chemotherapy and radiation.
Discussion
Ewing’s Sarcoma is a malignant bone tumour which in this case affects a female, which is not as common as a male. In this case, the pt. demonstrated constitutional signs and symptoms including night sweats, weakness, fatigue, intermittent fever and increased pain at night which could indicate a systemic problem. Physical therapists should be aware that Ewing’s Sarcoma can mimic musculoskeletal signs and symptoms which can make it difficult to diagnosis. It is imperative to monitor the patient and refer out to patient’s MD when appropriate to prevent further metastasis of the tumour. The pelvic and hip region is the most common area affected by Ewing’s Sarcoma and can be difficult to observe and palpate due to its location. In this case the pt did not improve upon multiple visits which would indicate it is not a musculoskeletal pathology and the pt. was referred to her primary care provider for further testing.
Related Pages[edit | edit source]
A case report, Ewing's sarcoma of the ilium mimicking inflammatory arthritis of the hip.
National Organization for Rare Disorders.
References[edit | edit source]
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 Paulussen, Michael. Frohlich, Brigit, Jurgens, Herbert. Ewing Tumour: Incidence, Prognosis, and Treatment Options. Pediatric Drugs 2001; 3(12); 899-913.(accessed 28 Feb 2011).
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 2.7 Goodman, Boissonnault, Fuller. Pathology: Implications for the Physical Therapist. Pennsylvania: Saunders, 2003.
- ↑ 3.0 3.1 3.2 Medline Plus. Ewing’s Sarcoma. http://www.nlm.nih.gov/medlineplus/ency/article/001302.htm (accessed Feb 2011).
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 4.6 4.7 4.8 4.9 Gerrand C, Athanasou N, Brennan B, Grimer R, Judson I, Morland B, Peake D, Seddon B, Whelan J. UK guidelines for the management of bone sarcomas. Clinical Sarcoma Research. 2016 Dec 1;6(1):7.
- ↑ 5.0 5.1 5.2 5.3 5.4 Elaine Lonnemann’s Powerpoint, Oncology. Pathophysiology of Complex Patient Problems. Bellarmine University 2011.
- ↑ 6.0 6.1 6.2 6.3 6.4 6.5 Ewing sarcoma. Bone Cancer Research Trust. Accessed April 5, 2017.
- ↑ Ben Kridis W, Toumi N, Chaari H, Khanfir A, Ayadi K, Keskes H, Boudawara T, Daoud J, Frikha M. A review of Ewing sarcoma treatment: is it still a subject of debate?. Reviews on recent clinical trials. 2017 Mar 1;12(1):19-23.
- ↑ 8.0 8.1 8.2 8.3 Burningham Z, Hashibe M, Spector L, Schiffman JD. The epidemiology of sarcoma. Clinical sarcoma research. 2012 Dec 1;2(1):14.
- ↑ 9.0 9.1 Goodman C, Snyder T. Differential Diagnosis for Physical Therapists: Screening for Referral. St. Louis, MO: Saunders Elsevier: 2007
- ↑ 10.0 10.1 Karosas AO. Ewing’s sarcoma. American Journal of Health-System Pharmacy. 2010 Oct 1;67(19):1599-605.
- ↑ Ewing’s SarcomaTreatment. National Cancer Institute. https://www.cancer.gov/types/bone/hp/ewing-treatment-pdq#link/_153_toc.
- ↑ https://rarediseases.org/rare-diseases/langerhans-cell-histiocytosis/
- ↑ Bouaoud J, Temam S, Cozic N, Galmiche‐Rolland L, Belhous K, Kolb F, Bidault F, Bolle S, Dumont S, Laurence V, Plantaz D. Ewing’s Sarcoma of the Head and Neck: Margins are not just for surgeons. Cancer medicine. 2018 Dec;7(12):5879-88.
- ↑ Yu H, Ge Y, Guo L, Huang L. Potential approaches to the treatment of Ewing's sarcoma. Oncotarget. 2017 Jan 17;8(3):5523.
- ↑ Joseph Dorrell. Physiopedia Ewing's Sarcoma PT Management. Available from: http://www.youtube.com/watch?v=FRcrAieE_TA[last accessed 25/7/2020]