Calcaneal Spurs: Difference between revisions
No edit summary |
No edit summary |
||
| Line 126: | Line 126: | ||
== Non Medical Management <br> == | == Non Medical Management <br> == | ||
<u>'''Tier I'''</u><br> ● '''Padding & strapping''' of the foot<ref>Shikoff MD, Figura MA, Postar SE. A retrospective study of 195 patients with heel pain. J Am Podiatr Med Assoc 76:71–75, 1986.
(level of evidence: 2B)</ref><ref>Williams PL. The painful heel. Br J Hosp Med 38:562–563, 1987.
(level of evidence: 4)</ref><br> Video: [https://www.youtube.com/watch?v=jKGDhxcdtzE https://www.youtube.com/watch?v=jKGDhxcdtzE]<br> ● '''Therapeutic orthodic insoles''' for ''short-term painrelieve''<ref>Landorf KB, Keenan AM, Herbert RD. Effectiveness of foot orthoses to treat plantar fasciitis: a randomized trial. Arch Intern Med 166:1305–1310, 2006.(level of evidence: 1B)</ref><ref>Roos E, Engstrom M, Soderberg B. Foot orthoses for the treatment of plantar fasciitis. Foot Ankle Int 27:606–611, 2006.(level of evidence: 1B)</ref><br> ● '''Achilles & plantar fascia stretching'''<ref>DiGiovanni BF, Nawoczenski DA, Lintal ME, Moore EA, Murray JC, Wilding GE, Baumhauer JF. Tissue-specific plantar fascia-stretching exercise enhances outcomes in patients with chronic heel pain. A prospective, randomized study. J Bone Joint Surg Am 85-A:1270–1277, 2003.(level of evidence: 1B)</ref><ref>Digiovanni BF, Nawoczenski DA, Malay DP, Graci PA, Williams TT, Wilding GE, Baumhauer JF. Plantar fascia-specific stretching exercise improves outcomes in patients with chronic plantar fasciitis. A prospective clinical trial with two-year follow-up. J Bone Joint Surg Am 88:1775–1781, 2006.(level of evidence: 2B)</ref><br> Video : [https://www.youtube.com/watch?v=hauyuX-uCq8 https://www.youtube.com/watch?v=hauyuX-uCq8]<br> → ''All grade B recommedation'' | <u>'''Tier I'''</u><br> ● '''Padding & strapping''' of the foot<ref>Shikoff MD, Figura MA, Postar SE. A retrospective study of 195 patients with heel pain. J Am Podiatr Med Assoc 76:71–75, 1986.
(level of evidence: 2B)</ref><ref>Williams PL. The painful heel. Br J Hosp Med 38:562–563, 1987.
(level of evidence: 4)</ref><br> Video: [https://www.youtube.com/watch?v=jKGDhxcdtzE https://www.youtube.com/watch?v=jKGDhxcdtzE]<br> ● '''Therapeutic orthodic insoles''' for ''short-term painrelieve''<ref>Landorf KB, Keenan AM, Herbert RD. Effectiveness of foot orthoses to treat plantar fasciitis: a randomized trial. Arch Intern Med 166:1305–1310, 2006.(level of evidence: 1B)</ref><ref>Roos E, Engstrom M, Soderberg B. Foot orthoses for the treatment of plantar fasciitis. Foot Ankle Int 27:606–611, 2006.(level of evidence: 1B)</ref><br> ● '''Achilles & plantar fascia stretching'''<ref>DiGiovanni BF, Nawoczenski DA, Lintal ME, Moore EA, Murray JC, Wilding GE, Baumhauer JF. Tissue-specific plantar fascia-stretching exercise enhances outcomes in patients with chronic heel pain. A prospective, randomized study. J Bone Joint Surg Am 85-A:1270–1277, 2003.(level of evidence: 1B)</ref><ref>Digiovanni BF, Nawoczenski DA, Malay DP, Graci PA, Williams TT, Wilding GE, Baumhauer JF. Plantar fascia-specific stretching exercise improves outcomes in patients with chronic plantar fasciitis. A prospective clinical trial with two-year follow-up. J Bone Joint Surg Am 88:1775–1781, 2006.(level of evidence: 2B)</ref><br> Video : [https://www.youtube.com/watch?v=hauyuX-uCq8 https://www.youtube.com/watch?v=hauyuX-uCq8]<br> → ''All grade B recommedation'' <br><u>'''Tier II'''</u><br> ● '''Prefabricated and custom orthodic device''' <br> prefabricated shows better results compared to the custom device in the improvement of symptoms <ref>Pfeffer, Glenn, et al. "Comparison of custom and prefabricated orthoses in the initial treatment of proximal plantar fasciitis." Foot &amp; Ankle International 20.4 (1999): 214-221.(level of evidence: 1B)</ref><br> → ''Grade B recommedation''<br> ● '''Night splints'''<ref>Lee, Sae Yong, Patrick McKeon, and Jay Hertel. "Does the use of orthoses improve self-reported pain and function measures in patients with plantar fasciitis? A meta-analysis." Physical Therapy in Sport 10.1 (2009): 12-18.(level of evidence: 1A)</ref><br> →''Grade B recommedation''<br> ●'''Physiotherapy'''<ref>Cleland JA, Abbott JH, Kidd MO, Stockwell S, Cheney S, Gerrard DF, Flynn TW. Manual physical therapy and exercise versus electrophysical agents and exercise in the management of plantar heel pain: a multicenter randomized clinical trial.(level of evidence: 1B)</ref><br> → ''Grade I recommedation''<br> ● '''Cast or boot immobilisation'''<ref>Cole C, Seto C, Gazewood J. Plantar fasciitis: evidence-based review of diagnosis and therapy. Am Fam Physician 72:2237–2242, 2005. (level of evidence: 1A)</ref><br> → ''Grade C recommedation'' | ||
<br><u>'''Tier II'''</u><br> ● '''Prefabricated and custom orthodic device''' <br> prefabricated shows better results compared to the custom device in the improvement of symptoms <ref>Pfeffer, Glenn, et al. "Comparison of custom and prefabricated orthoses in the initial treatment of proximal plantar fasciitis." Foot & Ankle International 20.4 (1999): 214-221.(level of evidence: 1B)</ref><br> → ''Grade B recommedation''<br> ● '''Night splints'''<ref>Lee, Sae Yong, Patrick McKeon, and Jay Hertel. "Does the use of orthoses improve self-reported pain and function measures in patients with plantar fasciitis? A meta-analysis." Physical Therapy in Sport 10.1 (2009): 12-18.(level of evidence: 1A)</ref><br> →''Grade B recommedation''<br> ●'''Physiotherapy'''<ref>Cleland JA, Abbott JH, Kidd MO, Stockwell S, Cheney S, Gerrard DF, Flynn TW. Manual physical therapy and exercise versus electrophysical agents and exercise in the management of plantar heel pain: a multicenter randomized clinical trial.(level of evidence: 1B)</ref><br> → ''Grade I recommedation''<br> ● '''Cast or boot immobilisation'''<ref>Cole C, Seto C, Gazewood J. Plantar fasciitis: evidence-based review of diagnosis and therapy. Am Fam Physician 72:2237–2242, 2005. (level of evidence: 1A)</ref><br> → ''Grade C recommedation'' | |||
<br><u>'''Tier III'''</u><br> ● '''ESWT''' (Extracorporal Shock Wave Therapy)<ref>Lee, Gregory P., John A. Ogden, and G. Lee Cross. "Effect of extracorporeal shock waves on calcaneal bone spurs." Foot & ankle international 24.12 (2003): 927-930. (level of evidence: 1A)</ref><ref>Marks W, Jackiewicz A, Witkowski Z, Kot J, Deja W, Lasek J. Extracorporeal shock- wave therapy (ESWT) with a new-generation pneumatic device in the treatment of heel pain. A double blind randomised controlled trial. Acta Orthop Belg 74:98– 101, 2008. (level of evidence: 1B)</ref><ref>Chuckpaiwong B, Berkson EM, Theodore GH. Extracorporeal shock wave for chronic proximal plantar fasciitis: 225 patients with results and outcome
predictors. J Foot Ankle Surg 48:148–155, 2009.
(level of evidence: 2B)</ref><ref>Pribut SM. Current approaches to the management of plantar heel pain syndrome, including the role of injectable corticosteroids. J Am Podiatr Med Assoc 97:68–74, 2007. (Level of Evidence: 5)</ref><br> → ''Grade B recommedation''<br> ● '''Bipolar radiofrequency''' ('''microtenotomy''')<ref>Weil L Jr, Glover JP, Sr Weil LS. A new minimally invasive technique for treating plantar fasciosis using bipolar radiofrequency: a prospective analysis. Foot Ankle Spec 1:13–18, 2008. (Level of Evidence: 4)</ref><br> → ''Grade C recommedation (2010)''<br> | <br><u>'''Tier III'''</u><br> ● '''ESWT''' (Extracorporal Shock Wave Therapy)<ref>Lee, Gregory P., John A. Ogden, and G. Lee Cross. "Effect of extracorporeal shock waves on calcaneal bone spurs." Foot &amp; ankle international 24.12 (2003): 927-930. (level of evidence: 1A)</ref><ref>Marks W, Jackiewicz A, Witkowski Z, Kot J, Deja W, Lasek J. Extracorporeal shock- wave therapy (ESWT) with a new-generation pneumatic device in the treatment of heel pain. A double blind randomised controlled trial. Acta Orthop Belg 74:98– 101, 2008. (level of evidence: 1B)</ref><ref>Chuckpaiwong B, Berkson EM, Theodore GH. Extracorporeal shock wave for chronic proximal plantar fasciitis: 225 patients with results and outcome
predictors. J Foot Ankle Surg 48:148–155, 2009.
(level of evidence: 2B)</ref><ref>Pribut SM. Current approaches to the management of plantar heel pain syndrome, including the role of injectable corticosteroids. J Am Podiatr Med Assoc 97:68–74, 2007. (Level of Evidence: 5)</ref><br> → ''Grade B recommedation''<br> ● '''Bipolar radiofrequency''' ('''microtenotomy''')<ref>Weil L Jr, Glover JP, Sr Weil LS. A new minimally invasive technique for treating plantar fasciosis using bipolar radiofrequency: a prospective analysis. Foot Ankle Spec 1:13–18, 2008. (Level of Evidence: 4)</ref><br> → ''Grade C recommedation (2010)''<br> | ||
== Missing evidence in the guidlines <br> == | |||
== Physical Therapy Management <br> == | == Physical Therapy Management <br> == | ||
Revision as of 12:15, 19 May 2016
Original Editors
Top Contributors - Ivakhnov Sergei, Caro De Koninck, Sheik Abdul Khadir, Scott Cornish, Admin, Simisola Ajeyalemi, Kim Jackson, Rachael Lowe, Joao Costa, Wanda van Niekerk, 127.0.0.1, Evan Thomas, Naomi O'Reilly and Priyanka Chugh
Search Strategy[edit | edit source]
add text here related to databases searched, keywords, and search timeline
Definition/Description[edit | edit source]
A calcaneal spur, or commonly known as a heel spur, occurs when there is a bone spur (a bony outgrowth) formed on the heel bone. Calcaneal spurs can be located at the back of the heel (dorsal heel spur) or under the sole (plantar heel spur). The dorsal spurs are often associated with achilles Tendinopathy, while spurs under the sole are associated with Plantar fasciitis.
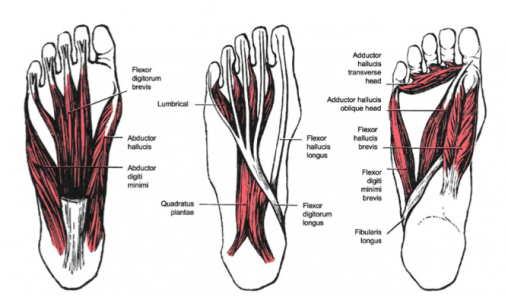
The apex of the spur lies either within the origin of the planter fascia (on the medial tubercle of the calcaneus) or superior to it (in the origin of the flexor digitorum brevis muscle). The relationship between spur formation, the medial tubercle of the calcaneus and intrinsic heel musculature results in a constant pulling effect on the plantar fascia consequent a inflammatory process.[1]
Clinically Relevant Anatomy[edit | edit source]
M. Soleus
M. Gastrocnemius
M. Plantaris
M. Abductor Digiti minimi
M. Flexor digitorum brevis
M. Extensor digitorum brevis
M. Abductor hallucis
M. Extensor hallucis brevis
M. Quadratus plantae
Plantar fascia
All of these structures are in a position to exert a traction force on the tuberosity and adjacent regions of the calcaneus, especially when excessive or abnormal pronation occurs. The origin of the spurs appears to be repetitive trauma that produced microtears in the plantar fascia near its attachment and the attempted repair led to inflammation which is responsible for the release and the maintenance of the symptoms.[2][3][4][5]
Epidemiology /Etiology[edit | edit source]
The etiology of the spur has been debated. At the beginning of the twentieth century, gonorrhea was considered a prime ethiological factor. Heredity, metabolic disorders, tuberculosis, systemic inflammatory diseases and many other disorders have also been implicated. Now abnormal biomechanics (excessive or abnormal pronation) enjoys wide support as the prime etiological factor for the painful plantar heel and the inferior calcaneal spur. The spur is thought to be a result of the biomechanical fault and an incidental finding when associated with the painful plantar heel.
The most common etiology involves abnormal pronation with resultant increased tension forces developed in the structures attaching in the region of the calcaneal tuberosity.
Asymptomatic heel spurs are relatively common in the normal, adult population. One epidemiologic study found that 11% of the adult U.S. population demonstrated a calcaneal spur as an incidental radiographic finding.[6]
Characteristics/Clinical Presentation[edit | edit source]
The painful heel is a relatively common foot problem but calcaneal spurs are not considered a primary cause of heel pain. A calcaneal spur is caused by long-term stress on the plantar fascia and muscles on the foot and may develop as a reaction to plantar fasciitis.[7]
The pain, mostly localised in the area of the medial process of the calcaneal tuber, is caused by pressure in the region of the plantar aponeurosis attachment to the calcaneal bone. The condition may exist without producing symptoms, or it may become very painful, even disabling.[8]
Most heel pain patients are middle-aged adults. Some of them are obese, so obesity can be considered a risk factor. Not all heel spurs cause symptoms and are often painless, but when they do cause symptoms people often experience more pain during weight-bearing activities, in the morning or after a period of rest. The experienced pain, however, is not the result of pressure of weight on the top of the spur but comes from an inflammation around tendons where they attach to the bone.
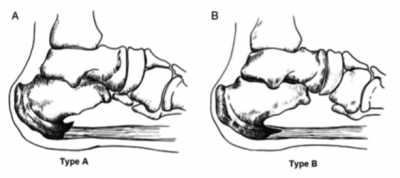
Two types of calcaneal spurs may be distinguished. Type A spurs are superior to the plantar fascia insertion, and type B spurs stretch forward from the plantar fascia insertion to extend distally within the plantar fascia.
The mean spur length for type A calcaneal spurs is significantly longer statistically than the mean spur length for type B spurs, while patients with type B spurs reported more severe clinical pain.[9]
Differently, spurs can be classified into three types:
- There are those which are large in size but are asymptomatic, because the angle of growth is such that the spur does not become a weight-bearing point and/or the inflammatory changes have been arrested.[10]
- Secondly, there are those which are large as well as painful upon weight-bearing, because the pitch of the calcaneus has been changed by a depression of the longitudinal arch and, as a result, the spur may become a weight-bearing point, sometimes causing intractable refractory pain.[10]
- Lastly, there are those which have only a rudiment of proliferation and whose outline is irregular and jagged, usually accompanied by an area of decreased density around the origin of the plantar fascia, indicating a subacute inflammatory process. All calcaneal spurs undoubtedly begin in this manner, but only a few become symptomatic at this stage, because the etiologic factors are acute.[10]
Differential Diagnosis[edit | edit source]
Because chronic heel pain is a common manifestation of many conditions, these must be excluded before planning treatment. Medical (diagnostic) imaging as well as medical signs are often used to differentiate some of the conditions that are mentioned below from calcaneal spurs.
1. Musculoskeletal causes:
- Peroneal tendonitis: (inflammation of one or both peroneal tendons)
MRI scan (level 3B) or ultrasound investigation (level 4).
- Haglund's deformity(with or without bursitis): (symptomatic osseous posterior-superior prominence of the calcaneus)
Radiographs or Sonography of foot in maximal dorsiflexion (level I).[11]
- Sever's disease(calcaneal apophysitis): (inflammation of the calcaneal apophysis due to overloading)
Clinical[12] (level 3B), ultrasonography[13] (level 4).
2. Traumatic influences:
- Calcaneal fractures (and stress fractures): (fractures as a consequence of repetitive load to the heel)
Ottawa Ankle Rules, Radiography, MRI (isotopic bone scan) and ultrasound.[14]
3. Neurological causes:
- Baxter nerve entrapment: (chronic compression of the first branch of the lateral plantar nerve)
Clinical (Tinel’s sign) (level 2A).
- Tarsal tunnel syndrome (sinus tarsi): (Impingement of the posterior tibial nerve)
Clinical (Tinel’s sign, dorsiflexion-eversion test) (level 1B).
4. Other:
- Heel fat pad syndrome: (Atrophy or inflammation of the shock-absorbing fatty pad or corpus adiposum)
Clinical, ultrasound scan (level 1B).
- Chronic lateral ankle pain with other cause:
MRI (level 4).
Diagnostic Procedures[edit | edit source]
The diagnosis is based on the patient's history and on results of the physical examination. The suspicion diagnose is confirmed mostly in the X-ray on the calcaneus, but diagnostic adjuncts are available to assist the clinician.[15] Radiology may demonstrate calcaneal spur formation or calcification at either the insertion of the Achilles tendon or the origin of the plantar fascia.[16]
Rarely MRI may be required.
Outcome Measures[edit | edit source]
Lower Extremity Functional Scale (LEFS)
Examination[edit | edit source]
There are different aspects that need to be taken in consideration when performing the clinical examination.
- Is there a limitation in range of motion in the ankle and foot?
Spend more attention to passive dorsiflexion in the toes.
Video : https://www.youtube.com/watch?v=QsCmuO37-aA
- Palpation of the plantar fascia end heel. The presence of the calcaneal spur, any tenderness (site/severity) or deformities can be felt (in combination with the dorsiflexion in the ankle)
- Is there any atrophy of the heel pad in compare with the other foot in combination with reduced muscle strength?
- Is there any swelling?
- Sensation
→ Hypesthesias/dysthesias? (tibial nerve) → Tinel’s sign
- Are there any skin tears on the foot?
- Any difference in foot-alignement in compare with the other foot?
→ Weight-bearing
- Evaluation of the gait
Medical Management
[edit | edit source]
Tier I
● Non steroidal anti inflammatory drugs (NSAID)[17]
→ Grade I recommendation
● Cortisone injections[18]
→ Grade B recommedation
Tier II
● Repeat cortisone injections[19][20][21]
→ Grade B recommedation
● Botulinum toxin[22][23][24]
→ Grade I recommendation
Tier III
● Endoscopic plantar fasciotomy[25]
● In-step fasciotomy[26][27]
● Minimal invasive surgical technique
→ All grade B recommendation
Non Medical Management
[edit | edit source]
Tier I
● Padding & strapping of the foot[28][29]
Video: https://www.youtube.com/watch?v=jKGDhxcdtzE
● Therapeutic orthodic insoles for short-term painrelieve[30][31]
● Achilles & plantar fascia stretching[32][33]
Video : https://www.youtube.com/watch?v=hauyuX-uCq8
→ All grade B recommedation
Tier II
● Prefabricated and custom orthodic device
prefabricated shows better results compared to the custom device in the improvement of symptoms [34]
→ Grade B recommedation
● Night splints[35]
→Grade B recommedation
●Physiotherapy[36]
→ Grade I recommedation
● Cast or boot immobilisation[37]
→ Grade C recommedation
Tier III
● ESWT (Extracorporal Shock Wave Therapy)[38][39][40][41]
→ Grade B recommedation
● Bipolar radiofrequency (microtenotomy)[42]
→ Grade C recommedation (2010)
Missing evidence in the guidlines
[edit | edit source]
Physical Therapy Management
[edit | edit source]
add text here
Key Research[edit | edit source]
add links and reviews of high quality evidence here (case studies should be added on new pages using the case study template)
Resources
[edit | edit source]
add appropriate resources here
Clinical Bottom Line[edit | edit source]
add text here
Recent Related Research (from Pubmed)[edit | edit source]
see tutorial on Adding PubMed Feed
Extension:RSS -- Error: Not a valid URL: Feed goes here!!|charset=UTF-8|short|max=10
References[edit | edit source]
see adding references tutorial.
- ↑ Johal KS .,‘Plantar fasciitis and the calcaneal spur: Fact or fiction?’., Foot Ankle Surg.,18 March 2012 (level of evidence 3B)
- ↑ Gill LH. Plantar fasciitis: diagnosis and conservative management. J Am Acad Orthop Surg, 1997
- ↑ McCarthy DJ, Gorecki GE: The anatomical basis of inferior calcaneal lesions. J Am Podiatry Assoc 69527-536,1979 (level of evidence: 2C)
- ↑ Young CC, Rutherford DS, Niedfeldt MW. Treatment of plantar fasciitis. AmfckLRFam Physician 2001 (level of evidence: 5)
- ↑ Heyd, Reinhard, et al. "Radiation therapy for painful heel spurs." Strahlentherapie und Onkologie 183.1 (2007): 3-9. (level of evidence: 1B)
- ↑ McCarthy DJ, Gorecki GE: The anatomical basis of inferior calcaneal lesions. J Am Podiatry Assoc 69527-536,1979 (level of evidence: 2C)
- ↑ E.K. Agyekum., “Heel pain: A systematic review”., Chinese Journal of Traumatology., 2015 (level of evidence 1A)
- ↑ B. Jasiak-Tyrkalska., ‘Efficacy of two different physiotherapeutic preocedures in comprehensive therapy of plantar calcaneal spur’., Fizjoterapia Polska., January 2007 (level of evidence: 1B)
- ↑ Zhou, Binghua, et al. "Classification of Calcaneal Spurs and Their Relationship With Plantar Fasciitis." The Journal of Foot and Ankle Surgery 54.4 (2015): 594-600. (level of evidence: 3A)
- ↑ 10.0 10.1 10.2 Henri L. Duvries., “Heel Spur (Calcaneal Spur)”., AMA Arch Surg., (level of evidence: 3A)
- ↑ Chauveaux, D., et al. "A new radiologic measurement for the diagnosis of Haglund's deformity." Surgical and Radiologic Anatomy 13.1 (1991): 39-44. (level of evidence: I)
- ↑ Perhamre, Stefan, et al. "Sever’s injury: a clinical diagnosis." Journal of the American Podiatric Medical Association 103.5 (2013): 361-368. (level of evidence: 3A)
- ↑ Hosgoren, B., A. Koktener, and Gülçin Dilmen. "Ultrasonography of the calcaneus in Sever's disease." Indian pediatrics 42.8 (2005): 801. (level of evidence: 4)
- ↑ Yu, Sarah M., and Joseph S. Yu. "Calcaneal avulsion fractures: an often forgotten diagnosis." American Journal of Roentgenology 205.5 (2015): 1061-1067. (level of evidence: 2A)
- ↑ Rosenbaum, Andrew J., John A. DiPreta, and David Misener. "Plantar heel pain." Medical Clinics of North America 98.2 (2014): 339-352. (level of evidence: 2A)
- ↑ Aldridge, Tracy. "Diagnosing heel pain in adults." American family physician 70 (2004): 332-342. (Level of evidence: 2A)
- ↑ Donley BG, Moore T, Sferra J, Gozdanovic J, Smith R. The efficacy of oral nonsteroidal anti-inflammatory medication (NSAID) in the treatment of plantar fasciitis: a randomized, prospective, placebo-controlled study. Foot Ankle Int 28:20–23, 2007.(level of evidence: 1B)
- ↑ Kalaci A, Cakici H, Hapa O, Yanat AN, Dogramaci Y, Sevinç TT. Treatment of plantar fasciitis using four different local injection modalities: a randomized prospective clinical trial. J Am Podiatr Med Assoc 99:108–113, 2009.(level of evidence: 1B)
- ↑ Kiter E, Celikbas E, Akkaya S, Demirkan F, Kilic BA. Comparison of injection modalities in the treatment of plantar heel pain: a randomized controlled trial. J Am Podiatr Med Assoc 96:293–296, 2006. (level of evidence: 1B)
- ↑ Buccilli TA Jr, Hall HR, Solmen JD. Sterile abscess formation following a cortico- steroid injection for the treatment of plantar fasciitis. J Foot Ankle Surg 44:466– 468, 2005. (level of evidence: 3A)
- ↑ Porter MD, Shadbolt B. Intralesional corticosteroid injection versus extracorporeal shock wave therapy for plantar fasciopathy. Clin J Sport Med 15:119–124, 2005. (level of evidence: 1B)
- ↑ Placzek R, Holscher A, Deuretzbacher G, Meiss L, Perka C. [Treatment of chronic plantar fasciitis with botulinum toxin Adan open pilot study on 25 patients with a 14-week-follow-up.]. Z Orthop Ihre Grenzgeb 144:405–409, 2006. German. (level of evidence: 1B)
- ↑ Placzek R, Deuretzbacher G, Meiss AL. Treatment of chronic plantar fasciitis with Botulinum toxin A: preliminary clinical results. Clin J Pain 22:190–192, 2006. (level of evidence: 1B)
- ↑ Babcock MS, Foster L, Pasquina P, Jabbari B. Treatment of pain attributed to plantar fasciitis with botulinum toxin a: a short-term, randomized, placebo- controlled, double-blind study. Am J Phys Med Rehabil 84:649–654, 2005. (level of evidence: 1B)
- ↑ Urovitz EP, Birk-Urovitz A, Birk-Urovitz E. Endoscopic plantar fasciotomy in the treatment of chronic heel pain. Can J Surg 51:281–283, 2008. (level of evidence: 2A)
- ↑ Fishco WD, Goecker RM, Schwartz RI. The instep plantar fasciotomy for chronic plantar fasciitis. A retrospective review. J Am Podiatr Med Assoc 90:66–69, 2000.(level of evidence: 2B)
- ↑ Woelffer KE, Figura MA, Sandberg NS, Snyder NS. Five-year follow-up results of instep plantar fasciotomy for chronic heel pain. J Foot Ankle Surg 39:218–223, 2000. (level of evidence: 2B)
- ↑ Shikoff MD, Figura MA, Postar SE. A retrospective study of 195 patients with heel pain. J Am Podiatr Med Assoc 76:71–75, 1986. (level of evidence: 2B)
- ↑ Williams PL. The painful heel. Br J Hosp Med 38:562–563, 1987. (level of evidence: 4)
- ↑ Landorf KB, Keenan AM, Herbert RD. Effectiveness of foot orthoses to treat plantar fasciitis: a randomized trial. Arch Intern Med 166:1305–1310, 2006.(level of evidence: 1B)
- ↑ Roos E, Engstrom M, Soderberg B. Foot orthoses for the treatment of plantar fasciitis. Foot Ankle Int 27:606–611, 2006.(level of evidence: 1B)
- ↑ DiGiovanni BF, Nawoczenski DA, Lintal ME, Moore EA, Murray JC, Wilding GE, Baumhauer JF. Tissue-specific plantar fascia-stretching exercise enhances outcomes in patients with chronic heel pain. A prospective, randomized study. J Bone Joint Surg Am 85-A:1270–1277, 2003.(level of evidence: 1B)
- ↑ Digiovanni BF, Nawoczenski DA, Malay DP, Graci PA, Williams TT, Wilding GE, Baumhauer JF. Plantar fascia-specific stretching exercise improves outcomes in patients with chronic plantar fasciitis. A prospective clinical trial with two-year follow-up. J Bone Joint Surg Am 88:1775–1781, 2006.(level of evidence: 2B)
- ↑ Pfeffer, Glenn, et al. "Comparison of custom and prefabricated orthoses in the initial treatment of proximal plantar fasciitis." Foot & Ankle International 20.4 (1999): 214-221.(level of evidence: 1B)
- ↑ Lee, Sae Yong, Patrick McKeon, and Jay Hertel. "Does the use of orthoses improve self-reported pain and function measures in patients with plantar fasciitis? A meta-analysis." Physical Therapy in Sport 10.1 (2009): 12-18.(level of evidence: 1A)
- ↑ Cleland JA, Abbott JH, Kidd MO, Stockwell S, Cheney S, Gerrard DF, Flynn TW. Manual physical therapy and exercise versus electrophysical agents and exercise in the management of plantar heel pain: a multicenter randomized clinical trial.(level of evidence: 1B)
- ↑ Cole C, Seto C, Gazewood J. Plantar fasciitis: evidence-based review of diagnosis and therapy. Am Fam Physician 72:2237–2242, 2005. (level of evidence: 1A)
- ↑ Lee, Gregory P., John A. Ogden, and G. Lee Cross. "Effect of extracorporeal shock waves on calcaneal bone spurs." Foot & ankle international 24.12 (2003): 927-930. (level of evidence: 1A)
- ↑ Marks W, Jackiewicz A, Witkowski Z, Kot J, Deja W, Lasek J. Extracorporeal shock- wave therapy (ESWT) with a new-generation pneumatic device in the treatment of heel pain. A double blind randomised controlled trial. Acta Orthop Belg 74:98– 101, 2008. (level of evidence: 1B)
- ↑ Chuckpaiwong B, Berkson EM, Theodore GH. Extracorporeal shock wave for chronic proximal plantar fasciitis: 225 patients with results and outcome predictors. J Foot Ankle Surg 48:148–155, 2009. (level of evidence: 2B)
- ↑ Pribut SM. Current approaches to the management of plantar heel pain syndrome, including the role of injectable corticosteroids. J Am Podiatr Med Assoc 97:68–74, 2007. (Level of Evidence: 5)
- ↑ Weil L Jr, Glover JP, Sr Weil LS. A new minimally invasive technique for treating plantar fasciosis using bipolar radiofrequency: a prospective analysis. Foot Ankle Spec 1:13–18, 2008. (Level of Evidence: 4)