Tarsal Tunnel Syndrome
Original Editor - David Cameron
Top Contributors - Admin, Blondeel Jonathan, Dieter Schuddinck, Rani Sileghem, Staci Burns, Kim Jackson, Rachael Lowe, Jesse Lemmens, Vidya Acharya, 127.0.0.1, Tarina van der Stockt, Naomi O'Reilly, Kai A. Sigel, WikiSysop and Jenny Wong
Definition/Description[edit | edit source]
Tarsal tunnel syndrome (TTS) is a compressive neuropathy of the posterior tibial nerve.[1] The tunnel lies posterior to the medial malleolus of the ankle, beneath the flexor retinaculum. Symptoms include pain radiating into the foot, usually, this pain is worsened by walking (or weight-bearing activities). An examination may reveal Tinel’s sign over the tibial nerve at the ankle, weakness, and atrophy of the small foot muscles or loss of sensation in the foot.[2]
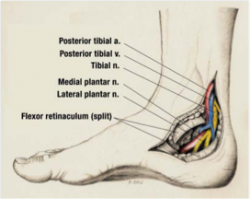
Clinically Relevant Anatomy[edit | edit source]
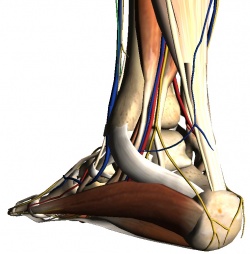
The tarsal tunnel is a channel between the medial malleolus, talus, calcaneus and the flexor retinaculum – a fibrous sheet that runs from the medial malleolus to the calcaneus. The tunnel contains[3][4]:
- Tibialis posterior tendon
- Flexor digitorum longus tendon
- Posterior tibial artery & vein
- Tibial nerve (yellow in the image)
- Flexor hallucis longus tendon
The tibial nerve divides into two terminal branches - the medial and lateral plantar nerves - as it passes through the tarsal tunnel. The medial calcaneal nerve branches from the tibial nerve at or superior to the flexor retinaculum. [5][6][7][8]
Tarsal Tunnel Syndrome (TTS) is a rare compressive neuropathy of the tibial nerve or one of its branches as they pass under the flexor retinaculum.[8][9][4][10][11]
In the TTS literature, the tibial nerve is also referred to as the posterior tibial nerve and TTS is also known as Posterior Tibial Nerve Neuralgia[9]. Some authors [12][6] refer to compression of the deep fibular nerve as “anterior tarsal tunnel syndrome”. This page is limited to the discussion of tarsal tunnel syndrome as the entrapment of the posterior tibial nerve or its branches.
Epidemiology/Etiology[edit | edit source]
Tarsal Tunnel Syndrome is caused by any kind of entrapment or compression of the tibial nerve or its plantar branches. In many cases, the cause is idiopathic or posttraumatic. Lau, M.D. et al. estimated that 20-40% of cases were idiopathic.[1][13] Up to 10% of all cases are the result of the following diseases: arthrosis, tenosynovitis, and Rheumatoid Arthritis. Nearly twice as many cases have convoluted vessels as the origin.[2]
Some other rare causes are Diabetes Mellitus, Hypothyroidism, Gout, mucopolysaccharidoses, and (very rarely) hyperlipidemia.[1]
Some muscles or tendons, medial of the talus bone, can entrap the tibial nerve due to hypertrophy or being accessory. As mentioned in the ‘anatomy’-section the tendon of the flexor hallucis longus muscle passes the tarsal tunnel along with blood vessels, the tibial nerve and other muscles. When enough hypertrophy occurs in one of these muscles the pressure within the tarsal tunnel increases. Sometimes this can even lead up to the muscle belly of the flexor hallucis longus entering the tarsal tunnel. This can cause an overstimulation of the tibial nerve or its branches. Depending on which nerve is being impinged, the patient can get different uncomfortable sensations in its foot.[14]
Some persons are born with accessory muscles. These variations from the norm can cause more harm than good. Those muscles are not necessarily helpful, but it is a given that they do occupy space within the foot. Similar to hypertrophy of the muscles in the medial ankle region, this can compress the tibial nerve possibly resulting in chronic pain.[15]
Surgery or an overload on the ankle region can cause local inflammation and swelling, yet again causing pressure on the tibial nerve. Sports where sprinting and jumping play a significant role have been proven to be provocative for TTS. People with flat feet, talocalcaneal coalition or bony fragments around the tarsal tunnel are more vulnerable to develop the syndrome.[1][13]
It might be important to mention that because tarsal tunnel syndrome is a relatively uncommon clinical entity, it can often be misdiagnosed in both children and adults due to the clinician’s low index of suspicion.[1] McSweeney & Cichero (2015) also state in their review that the incidence of TTS is not known but the prevalence would be greater in females than males, predominately in adults.[1] TTS also tends to be more common in athletes and individuals who are subjected to prolonged weight-bearing periods inclusive of standing, walking or intense physical activity.[1][15][16] Pes planus deformity/hyper pronation may compromise the anatomical structures within the tarsal tunnel and thus lead to a physical decrease of space and an increase in tension of the nerve.[1][16] It would be one of the most common extrinsic factors to cause TTS.[17] Alleviation of pain/complaints could be obtained with rest[16] or neutral immobilization of the foot and ankle, and loose-fitting footwear.[16] External compression resulting from footwear or tight plaster casts is said to be the most common cause.[18]
In summary:
- Incidence is unknown[4][10][19].
- A higher prevalence is reported for women than men[4][10][11].
- It can be seen at any age.[10]
- Causes of TTS include[9][4][10][20][6][11][21]:
- Repetitive stress activities such as running, excessive walking or standing
- Traumas such as fracture, dislocation or stretch injuries
- Heel varus or valgus
- Fibrosis
- Excessive Weight
- Space occupying lesions in tarsal tunnel region such as a ganglion, tumors, edema, osteophytes or varicosities
- Tendonitis
- Systemic diseases that cause ankle inflammation or nerve compromise (ex: diabetes mellitus, arthritis)
- Many cases (20%-40%) are idiopathic.[4][6]
Characteristics/Clinical Presentation[edit | edit source]
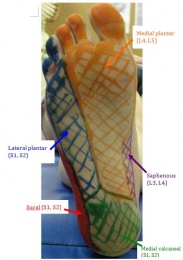
Common symptoms of TTS include paraesthesia (burning, numbness or tingling) in the posterior tibial, lateral plantar and/or medial plantar nerve distributions - see picture. Burning, tingling, or pain in the medial portion of the ankle and or plantar aspect of the foot, as well as local tenderness behind the medial malleolus, may be seen[22][8][23]. Symptoms usually worsen with forced eversion and dorsiflexion of foot. When the medial plantar nerve is affected in isolation, patients can present with a stabbing pain in the medial sole of the foot upon walking, which is usually seen in middle-aged runners. In a progressed or chronic case muscle weakness of the toe abductors and flexors can be demonstrated. In more serious cases, muscle atrophy can be seen[6]. Patients can also present with night pain that awakens them from sleep as well as aggravation with prolonged walking[19].
Differential Diagnosis[edit | edit source]
TTS can present similarly to other lower extremity conditions with the most common differential diagnosis being plantar fasciitis as these patients also present with plantar heel pain[7]. In addition to Plantar fasciitis (in which TTS is thought to be commonly misdiagnosed), polyneuropathy, L5 and S1 nerve root syndromes, Morton metatarsalgia, compartment syndrome of the deep flexor compartment will have to be distinguished from tarsal tunnel syndrome as well[6]. The most common causes are Posterior Tibialis Tendon Dysfunction.
Neuropathy - Most persons have once had the sensation of so-called sleeping limbs, usually referred to as paraesthesia. This feeling can also rise due to a pathogenic condition such as polyneuropathy. That’s when this numb, tingling feeling can no longer be put under control by the patient. It’s a condition that often arises at the hands or feet. Considering one has paraesthesia at the foot, the symptoms are very similar to those of the TTS.[1]
Ischemia - A shortage of oxygen supply to tissue is called ischemia. Permanent damage can occur when this supply is put on hold for an extensive time. As nerves start to lack oxygen, their functionality slowly decreases. The result of extended ischemia can be devastating. However, if a lack of blood flow is the cause, and it is normalized in time, damage can be near to none. Concerning nerves, in some cases, permanent ischemic paraesthesia can arise. This makes the neurons fire at random, which gives the same sensation as the symptoms of TTS.[1]
Compartment Syndrome - A compartment syndrome can mostly be found in the upper arm and lower leg. It can show up after a pressure build-up on or within a muscle compartment with an overload of certain muscle groups or fluid build-up being possible origins of this syndrome. The tibial nerve runs along the deep calf muscles with a compartment. Excessive pressure may trigger this nerve to fire uncontrollably. The TTS can be misdiagnosed for this compartment syndrome if the compression of the nerve mostly takes place near the medial malleolus.[1] The former has also proven to be able to produce a distal tibial nerve lesion. A lesion is any damage or abnormal change in tissue. A lesion in or near a nerve can compromise its function. Therefore, it can simulate the same symptoms as the TTS when a nerve near the medial malleolus is involved.[1]
Tumor - As a tumor is a group of cells that grow uncontrollably and can be benign, precancerous, or malignant. Despite these three distinctions, they do have in common that they take up space unnecessarily. Pressure caused by tumors rarely induces trouble to its surrounding tissues. It can however be a differential diagnosis for TTS if it overexcites a nerve at the medial malleolus.[1]
| A sum-up of possible differential diagnoses[1] |
|
Diagnostic Procedures[edit | edit source]
The diagnosis of TTS is mainly a clinical diagnosis based on detailed medical history and clinical examination. The clinical tests performed by physiotherapists are mostly provocative tests.[2] These will be further described in the topic “Examination” (underneath). Adjunctive medical imaging and electrophysiological studies may assist in diagnosing/>[25] and could provide additional information useful to plan management.[15]This can include electrodiagnostic studies, radiographs, ultrasound, MRI and computed tomography.[1][15][25][1][25][16][18] It is, for example, also possible for the digital abductor and flexor muscles of the symptomatic foot to weaken, atrophy, or even paralyze in some chronic circumstances.[1] This is often difficult to detect clinically and may therefore require subsequent referral for medical imaging or nerve conduction studies.[1] We should keep in mind though that these kinds of examinations are not substitutes for the clinical examination but they can play a key role in confirming or excluding the physician’s suspicion.[25]
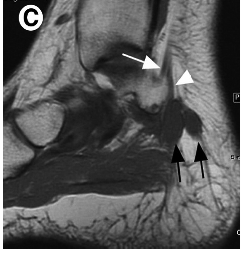
As already mentioned, diagnosing the cause of TTS, and actually a lot of other medial ankle and heel pain, by physical examination alone can be challenging for the clinician.[18] This is due to the complex anatomy of the medial aspect of the ankle and hindfoot, which makes localizing symptoms to a specific structure difficult.[18] For example, plain X-rays of the ankle are useful in demonstrating structural abnormalities such as hindfoot varus/valgus. Magnetic resonance imaging (MRI) adds further detail and is highly accurate (83%) when investigating space-occupying lesions.[15]
MRI is considered the gold standard in identifying suspected compression of the tarsal tunnel caused by the presence of obstructive foreign masses, lesions or tumors.[1][18] This type of imaging not only confirms the presence of a suspected lesion but also defines the depth, extent and margins of the lesion for accurate characterization.[1] In a study undertaken by Frey (reviewed by McSweeney & Cichero, 2015), MRI was deemed to have shown significant findings in 88% of symptomatic tarsal tunnel candidates, thus assisting with aetiological reasoning and surgical planning if required.[1] MRI and high-resolution ultrasound have the diagnostic capability to detect and demonstrate the thickness of the flexor retinaculum, overall depth and contents within the tarsal tunnel, including the posterior tibial nerve cross-sectional area and its terminal branch derivatives.[1]
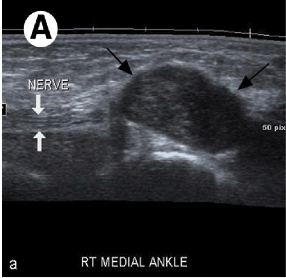
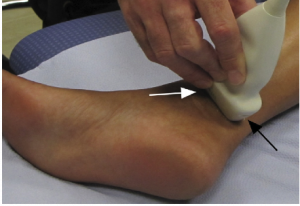
Ultrasound represents an accessible, portable and relatively inexpensive (less expensive than MRI) imaging tool for the assessment of medial ankle and heel pain.[18][17] In addition, it offers the advantage of comparison with the contralateral side.[18] Although MRI (above) is considered the gold standard, ultrasound is effective in the diagnosis of pathologic conditions affecting the medial ankle and heel and correlates well with MRI.[18] Ultrasound is able to demonstrate the complex anatomy of the tarsal tunnel and show the entire course of the tibial nerve and its branches at the medial ankle. It is also effective in the identification of space-occupying lesions. Even small changes in the cross-sectional area of the nerve can be detected on ultrasound in symptomatic patients.[18]
Electrodiagnostic testing can also assist in the diagnosis of tarsal tunnel syndrome.[1] These tests include nerve conduction studies that assess sensory conduction velocities of the tibial nerve or one of its branches, as well as the amplitude and duration of motor-evoked potentials.[1] There is limited quality evidence-based research that demonstrates high sensitivity and specificity of the electrophysiological techniques in TTS. Reduced amplitude and increased duration of the motor response are the more sensitive indicators of the presence of pathology.[1] Unfortunately, these investigations often yield an unacceptable level of false-negative results, and should be utilized as an adjunctive assessment to confirm physical examination findings.[1][2]
Saeed (reviewed by McSweeney & Cichero, 2015) discusses evidence of false-positive readings in his study of 70 asymptomatic subjects[1] and Ahmad et al (2012) report that false negative tests are not uncommon and therefore do not rule out the diagnosis.[15] Thus, Abouelela & Zohiery (2012) state that provocative tests remain important in the diagnosis of TTS due to the unaccepted range of false-negative results in electrodiagnostic testing.[2]
Last, plain weight-bearing radiographs and/or computed tomography of the foot and ankle should be acquired if suspecting morphological influences or structural anomalies from bony abnormalities, according to McSweeney & Cichero (2012).[1] Omoumi et al. (2010) state that in practice, the visualization of articular communication with MRI or ultrasonography can be challenging.[1] Computed tomography (arthrography) with delayed acquisitions has been shown to be a valuable technique for the detection of articular communication between structures and a joint.[1] In closing, it is recommended that all tests should ideally be performed bilaterally for adequate observation and comparative study of the contralateral joint.[1]
There exist a wide variety of clinical outcomes that can be used to evaluate foot conditions. In 2013 Kenneth J. et al. concluded in their 10-year research that most of them were inconsistently used. Out of 139 clinical outcomes the American Orthopaedic Foot & Ankle Society (AOFAS), the visual analog scale (VAS) for pain, the Short Form-36 (SF-36) Health Survey, the Foot Function Index (FFI) and the American Academy of Orthopaedic Surgeons (AAOS) outcomes instruments were the most popular. The study underlined the need for consistent use of a responsive, valid, reliable and clinically meaningful outcome measurement tool.[2]
One measurement tool that meets the requirements is the Foot and Ankle Ability Measure. It was made in 2005 by RobRoy et al. It covers a wide variety of disorders in the lower extremity, namely the lower leg, foot and ankle. Examples are plantar fasciitis[18], ankle instability[1], etc. Its clinical relevance was researched by Martin et al. and in the table underneath the validity, reliability and responsiveness of the tool is summarised.[17]
| Instrument | Content validity | Construct validity | Reliability | Responsiveness |
| FAAM | 1-factor structure and high interal consistency (alpha .96 and .98 respectively) |
- No correlation to SF-36 physical function subscale and physical component summary score (r, 0.78 and 0.84, respectively)* - Low correlation to SF-36 mental health subscale and mental component summary score* |
- ADL subscale - Sport subscale ICC, 0.89 (SEM 4,5) - MDC95 of 6 points on the ADL subscale and 12 points on the sport subscale during 9 wk |
- Minimum clinically important differences of 8 and 9 points for the ADL and sports subscales, respectively, distinguishing between those improved versus not improved after 4 wk of physical therapy* - Significantly different change in scores during 4 wk in the group expected to change (P<.001)* |
Examination[edit | edit source]
It is important to take a thorough history. The physical therapist should inquire about the following:[26]
- Mechanism of injury (MOI) – was there any trauma, strain, or overuse?
- Duration and location of pain and paraesthesia?
- Weakness or difficulty walking?
- Back or buttock pain associated with more distal symptoms?
- Pain getting worse, staying the same, or getting better?
Key history Findings:
- Paraesthesia or burning sensation in the territory of the distal branches of the tibial nerve
- Prolonged walking or standing often exacerbates patient’s pain
- Dysesthesia (an abnormal and unpleasant sensation) arises during the night and can disturb sleep
- Weakness of muscles
Observation (observe in weight-bearing and non-weight-bearing):
- Muscle atrophy of the abductor hallucis muscle may be seen
- Check for arch stability
- Position of the talus and calcaneus
Gait Analysis:
- Assess for abnormalities (excessive pronation/supination, out-toeing, excessive inversion/eversion, antalgic gait, etc.)
Sensory Testing
- Test light touch, 2-point discrimination, and pinprick in the lower extremity
- Deficits will be in the distribution of the posterior tibial nerve
Palpation:
- Tender to palpation in between the medial malleolus and Achilles tendon
- Painful in 60-100% of those affected[6]
Range of Motion (ROM):
- Focus on ankle and toe ROM
Manual Muscle Testing (MMT):
- Decreased strength generally occurs late in the progression of TTS
- The phalangeal abductors are impacted first, followed by the short-phalangeal flexors
Special Tests:
Tinel’s Sign:
- Percussion of the tarsal tunnel results in distal radiation of paraesthesias
- Elicited in over 50% of those affected [6]
Dorsiflexion – Eversion Test: [22]
- Place the patient’s foot into full dorsiflexion and eversion and hold for 5-10 seconds[26]
- The results are that it elicits the patient’s symptoms
EMG studies: [19]
- The presence of an isolated tibial nerve lesion in the tarsal tunnel is confirmed by measurement of the sensory and motor nerve conduction velocity (NCV).
- Sensory conduction velocity of the medial and lateral plantar nerves. This is best done by recording from the tibial nerve just above the flexor retinaculum and stimulating the nerves at the vault of the foot. When surface electrodes are used, the responses to stimulation are of low amplitude.
- Measurement of the motor NCV through recording of the distal motor latency at the abductor hallucis brevis muscle is a much easier, but less sensitive method. The important finding on electromyography (EMG) is the demonstration of axonal injury when the EMG is recorded from the distal muscles supplied by the tibial nerve.
Medical Management[edit | edit source]
PHARMACOLOGICAL MANAGEMENT
Pharmacological treatments are often used in combination with physical therapy management to optimize recovery and decrease functional disability.[4][6][26]
- NSAIDs
- Corticosteroid Injections
- Pain Medications
SURGICAL MANAGEMENT
Surgery is indicated for patients who have not benefited from conservative treatments such as physical therapy and have symptoms that significantly impact their daily life. Individuals with a space-occupying lesion tend to not to respond to conservative management and often require surgery. Godges and Klingman have identified several characteristics that have been associated with a successful response to surgery. The characteristics include; younger age, a short history of symptoms, no previous history of ankle pathology, early diagnosis, and a determined etiology.
- Posterior Tibial Nerve Decompression[27]
- If there is a space-occupying lesion, the lesion will be removed
and decompression will not be done. - Cryosurgery[28]
ALTERNATIVE MANAGEMENT
- Acupuncture[29]
Physical Therapy Management[edit | edit source]
There is a lack of evidence in the literature on treatment approaches.[13] Small RCTs would help to find successful rehabilitation exercises or other treatments for patients with tarsal tunnel syndrome.[1] Published papers have reported case studies, but empirical evidence of their efficacy is lacking.[1]
At the time patients who do not respond to physical therapy or other conservative treatment are referred to a clinician for a surgical approach (e.g. decompression of the tarsal tunnel).
Conservative treatment
There are three stages[14][13] (Levels of evidence: 5, 5) in the development of TTS, in every stage, there are different aspects that may be addressed in the management of the symptoms.
| Physical agents | Orthotics and taping | Therapeutic exercises | Manual therapy | |
|
Acute stage: reduce inflammation, tissue stress and pain |
- Ice - Contrast baths - Ultrasound - Lidocaine ointment - Iontophoresis - Interferential current therapy |
- UCBL orthosis - CAM walker - Plantar arch taping - Medial heel wedge - Patient education on footwear |
- Calf stretching - Nerve mobility |
- Soft tissue massage - Neural mobilization |
| Subacute stage: improve strength and flexibility | See above | See above |
- Tibialis posterior strengthening - Impairment based interventions |
See above |
| Settled stage: improve functional mobility, strength and flexibility bilaterally | See above | See above |
- Tibialis posterior strengthening in weight-bearing - Impairment based interventions |
See above |
Orthotics and taping[1][13][24] (Levels of evidence: 5, 5, 1B)
- UCBL orthosis: A University of California Berkeley Laboratory orthosis can be used to improve hindfoot alignment
- CAM walker: Controlled Ankle Motion walker, with this boot the ROM of the patients' ankle can be altered.
- Plantar arch taping[15]:
[30] - Patient education on footwear: the therapist should educate the patient on wearing appropriate footwear. Tight-fitting shoes should be avoided. When dealing with athletes one must pay attention to their running mechanics and/or motions in their technique (sport specific) that may cause the symptoms.[25]
Therapeutic exercises
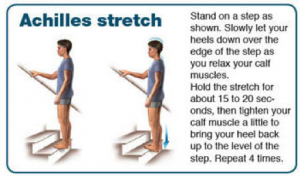
1) Stretching[1][13]
- Calf muscle: there are many ways to stretch the calf muscle, one of the most frequently used is the calf stretch using a wall. The first picture focuses on stretching the gastrocnemius muscle, the second picture focuses on stretching the soleus muscle.
- Achilles tendon:
- Plantar fascia:
1) Cross your affected leg over your other leg.
2) Using the hand on your affected side, take hold of your affected foot and pull your toes back towards the shin. This creates tension/stretch in the arch of the foot/plantar fascia.
3) Check for the appropriate stretch position by gently rubbing the thumb of your unaffected side left to right over the arch of the affected foot. The plantar fascia should feel firm, like a guitar string.
4) Hold the stretch for a count of 10. A set is 10 repetitions.
2) Nerve mobility[24]
Nerve mobilization exercises have been used to treat carpal tunnel syndrome (nerve entrapment in the wrist) with contradicting results. In the present literature, only a limited number of case studies where nerve mobilization exercises have been used to treat plantar heel pain of neural origin.
Kavlak Y. and Uygur F. conducted RCT where they used nerve mobilization techniques as an adjunct to conservative treatment. The study reported a positive outcome for ROM, muscle strength, and pain in both groups. The study group showed a significant improvement for 2-point discrimination, light touch, and Tinel’s sign.
Nerve mobilization as described by Meyer et al.[15]
The patient is seated at the edge of the table with the hand behind and is asked to slump forward into a comfortable position with the hands behind the back (see image). The ankle is taken into end-range dorsiflexion and eversion to bring tension on the tibial nerve. The knee is extended to R1 (= the angle where the PT feels the first resistance) with the ankle in end-range dorsiflexion and eversion and back to the relaxed flexed state. Each extension-flexion takes about 4 seconds and is repeated 10 times.
3) Tibialis posterior strengthening[1][15]
The function of the tibialis posterior muscle is to stabilize the ankle, it is also used for inversion of the ankle. Exercises can be classified into two categories: weight-bearing and non-weight bearing.
- Example of a non-weight bearing exercise:
[31]
- Example of a weight bearing exercise:
[32]
Other types of conservative treatment may include[13]:
• Rest
• NSAID’s
• Corticosteroid injections
• Extracorporeal shockwave therapy
• Laser
• Local anesthetic injections
• Heel pads and heel cups
• Night splints
• Medial longitudinal arch supports
• Strapping
• Soft-soled shoes
• Casting
It is recommended that patients are treated conservatively prior to the surgical treatment. When patients do not respond to the conservative treatment or if there are signs of atrophy or motor involvement, they should be referred to a clinician.
Postoperative rehabilitation[25]
| Timeline | Goals | Intervention | |
| Phase I | Week 1 - 3 |
- Protect joint/nerve integrity - Control inflammation - Control pain/edema |
- Immobilization - Passive mobilization - Surgical site protection - Elevation and ice - Educate and monitor non-weight bearing crutch ambulation |
| Phase II | Week 3 - 6 |
- Prevent contraction, scar tissue - Soft tissue and joint mobility |
- Weight-bearing as tolerated - Gentle passive, active-assist, active ankle stretches - Gentle passive dorsiflexion - Tibial nerve gliding with anti-tension - Pain-free, weight-bearing dorsiflexion - Gait training wearing protective splint - Aqua therapy |
| Phase III | Week 6 - 12 |
- Normal gait mechanics - Symmetric ankle mobility - Single leg proprioception - Repeated single leg heel raises (pain free) - Sport/job - specific exercises
|
- Gait training - Resistive ankle ex. (pain free) - Progress stretching ex. - Progress resistive ex. (to body weight) - Progress proprioceptive and balance ex. - Cardiovascular ex. (pain free) - Low level plyometric ex. |
Clinical Bottom Line[edit | edit source]
Tarsal tunnel syndrome is a rare condition and often underdiagnosed.[1] A variety of symptoms are possible, such as: tingling or burning pain (paraesthesia), hyperaesthesia and sensory impairment (dysesthesia). These are felt on the plantar face of the ankle and foot.
There are a few tests to identify tarsal tunnel syndrome or rule out other possibilities, the tests include: MRI, Ultrasound, Hoffman-Tinels test, dorsiflexion-eversion test, Trepman test, and the Triple compression stress test.[13]
Treatment of tarsal tunnel syndrome should be attempted conservatively at first (see “Physical therapy management”). If conservative treatment fails, a surgical approach can be taken.
There is a lack of high-quality research on the effective management of tarsal tunnel syndrome. The physical therapist should stage the patient based on swelling, pain, duration of symptoms and/or time since surgery. Management should be impairment-based to address specific strength, flexibility, gait and functional limitations of a given patient.
References[edit | edit source]
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 1.13 1.14 1.15 1.16 1.17 1.18 1.19 1.20 1.21 1.22 1.23 1.24 1.25 1.26 1.27 1.28 1.29 1.30 1.31 1.32 1.33 1.34 1.35 1.36 1.37 McSweeney SC, Cichero M. Tarsal tunnel syndrome-A narrative literature review. The Foot 2015;25:244-50)
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 https://www.ncbi.nlm.nih.gov/mesh/?term=tarsal+tunnel+syndrome
- ↑ Louisiana State University Health Sciences Center. Posterior Thigh Dissection Guide: Posterior leg - Tarsal tunnel. Available at: http://virtualhumanembryo.lsuhsc.edu/hs2412/laboratory/New_Lab_Guide/LowerLimb/TarsalTunnel.html. Accessed July 5, 2011.
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 4.6 Hudes, K. Conservative management of a case of tarsal tunnel syndrome. J can Chiropr Assoc. 2010; 54(2): 100-106.
- ↑ University Foot and Ankle Institute. Tarsal Tunnel Syndrome. Available at: http://www.footankleinstitute.com/tarsal-tunnel-syndrome. Accessed July 5, 2011.
- ↑ 6.0 6.1 6.2 6.3 6.4 6.5 6.6 6.7 6.8 Antoniadis G, Scheglmann K. Posterior tarsal tunnel syndrome: Diagnosis and treatment. Dtsch Arztebl Int. 2008; 1-5(45): 776-781.
- ↑ 7.0 7.1 Alshami AM, Babri AS, Souvlis T, Coppieters MW. Strain in the tibial and plantar nerves with foot and ankle movements and the influence of adjacent joint positions. J Applied Biomechanics. 2008; 24: 368-376.
- ↑ 8.0 8.1 8.2 Moore KL, Dalley AF, Agur AMR. Clinically Oriented Anatomy. 6th ed. Philadelphia, Pa: Lippincott Williams and Wilkins; 2010: 617-618, 666-667.
- ↑ 9.0 9.1 9.2 National Institute of Health – Office of Rare Disease Research. Tarsal tunnel syndrome. Available at: http://rarediseases.info.nih.gov/GARD/Condition/7733/QnA/21157/Tarsal_tunnel_syndrome.aspx. Accessed on July 5, 2011.
- ↑ 10.0 10.1 10.2 10.3 10.4 Llanos LF, Vila J, Nunez-Samper M. Clinical symptoms and treatment of the foot and ankle nerve entrapment syndromes. Foot and Ankle Surg. 1999; 5: 211-218.
- ↑ 11.0 11.1 11.2 Mondelli M, Morana P, Padua L. An electrophysiological severity scale in tarsal tunnel syndrome. Acta Neurol Scand. 2004; 109: 284-289.
- ↑ Zongzhoa L, Jiansheng Z, Li Z. Anterior tarsal tunnel syndrome. J Bone & Joint Surg. 1991; 73: 470-473.
- ↑ 13.0 13.1 13.2 13.3 13.4 13.5 13.6 13.7 Alshami AM, Souvlis T, Coppieters MW. A review of plantar heel pain of neural origin: Differntial diagnosis and management. Manual Therapy 2008;13:103-11.
- ↑ 14.0 14.1 Fantino O. Role of ultrasound in posteromedial tarsal tunnel syndrome: 81 cases. J Ultrasound 2014;17(2):99–112.
- ↑ 15.0 15.1 15.2 15.3 15.4 15.5 15.6 15.7 15.8 Cheung Y. Normal Variants: Accessory Muscles About the Ankle. Magn Reson Imaging Clin N Am. 2017;25(1):11-26.
- ↑ 16.0 16.1 16.2 16.3 16.4 Tu P, Bytomski JR. Diagnosis of Heel Pain. American Family Physician 2011;84(8):909-16.
- ↑ 17.0 17.1 17.2 Lin D, Williams C, Zaw H. A rare case of an accessory flexor hallucis longus causing tarsal tunnel syndrome. Foot Ankle Surg. 2014;20:e37-39.
- ↑ 18.0 18.1 18.2 18.3 18.4 18.5 18.6 18.7 18.8 18.9 Kotnis N, Harish S, Popowich T. Medial Ankle and Heel: Ultrasound Evaluation and Sonographic Appearances of Conditions Causing Symptoms. Seminars in Ultrasound, CT and MRI 2011;32:125-41.
- ↑ 19.0 19.1 19.2 Patel AT, Gaines K, Malamut R, Park A, Del Toro DR, Holland N. Usefulness of electrodiagnostic techniques in the evaluation of suspected tarsal tunnel syndrome: An evidence-based review. Muscle and Nerve. 2005; 236-240.
- ↑ American College of Foot and Ankle Surgeons. Tarsal tunnel syndrome. Available at: http://www.foothealthfacts.org/footankleinfo/tarsal-tunnel-syndrome.htm. Accessed on July 5, 2011.
- ↑ Toth C, McNeil S, Feasby T. Peripheral nervous system injuries in sport and recreation: A systematic review. Sports Med. 2006; 35(8): 717-738.
- ↑ 22.0 22.1 Kinoshita M, Okuda R, Morikawa J, Jotoku T, Abe M. The dorsiflexion-eversion test for diagnosis of tarsal tunnel syndrome. Journal of Bone and Joint Surgery, American Volume. December 2001; 83A (12): 1835-1839.
- ↑ Netter, FH. Atas of Human Anatomy. 5th ed. Philadelphia, Pa: Saunders Elsevier; 2011: 529.
- ↑ 24.0 24.1 24.2 Kavlak Y, Uygur F. Effects of nerve mobilization exercise as an adjunct to the conservative treatment for patients with tarsal tunnel syndrome. Journal of manipulative and physiological therapeutics 2011;34(7):441-48.
- ↑ 25.0 25.1 25.2 25.3 25.4 25.5 Moore KL, Dalley AF, Agur AMR. Clinically Oriented Anatomy. 6th ed. Philadelphia, Pa: Lippincott Williams and Wilkins;2010:617-18, 666-67.
- ↑ 26.0 26.1 26.2 Huber L, Lombara A. Clinical Review: Tarsal Tunnel Syndrome. Rehabilitation Operations Council: Glendale Adventist Medical Center. October 8, 2010.
- ↑ Ward P Porter M. Tarsal tunnel syndrome: a study of the clinical and neurophysiological results of decompression. Royal College of Surgeons of Edinburgh. 1998;43:35-36
- ↑ Goldstein S. New technologies. Cryosurgery for the treatment of tarsal tunnel syndrom. Podiatry Management. October 2006;25(8):163-170.
- ↑ Smith S. Acupuncture in the treatment of tarsal tunnel syndrome. Journal of Chinese Medicine. February 2009;(89):19-25.
- ↑ www.sportsinjuryclinic.netTaping technique for Plantar Fasciitis. Available fromhttps://www.youtube.com/watch?v=5Z2XlqsuQSY&feature=emb_logo
- ↑ MrHealthystep Tibialis Posterior Dysfunction - rehab exercises with latex band. Available from https://www.youtube.com/watch?v=zJ56EjnQ3Ok&feature=emb_logo
- ↑ ShaychiITATibialis posterior full weight - bearing heel raise strengthening Available fromhttps://www.youtube.com/watch?v=aDyr2wAOIhM&feature=emb_logo