Ankylosing Spondylitis (Axial Spondyloarthritis): Difference between revisions
No edit summary |
(clinical features) |
||
| (39 intermediate revisions by 8 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> | <div class="editorbox"> | ||
'''Original Editor '''- [[User:Thomas Rodeghero|Thomas Rodeghero]] | '''Original Editor '''- [[User:Thomas Rodeghero|Thomas Rodeghero]] | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | |||
</div> | |||
== Definition/Description == | == Definition/Description == | ||
[[File:AnkylosingSpondylitis.png|right|frameless|533x533px]] | [[File:AnkylosingSpondylitis.png|right|frameless|533x533px]] | ||
Axial spondyloarthritis is a seronegative [[spondyloarthritis]] of the spine and pelvis. The term axial spondyloarthritis has only been used since 2009 when the Assessment of Spondyloarthritis International Society Axial Spondyloarthritis (ASAS) classification criteria was developed. The ASAS criteria allowed, for the first time, earlier identification of axial spondyloarthritis through magnetic resonance imaging (MRI).<ref name=":6">Dubreuil M, Deodhar A. [https://www.ncbi.nlm.nih.gov/pmc/articles/pmc5810943/ Axial Spondyloarthritis Classification Criteria–The debate continues]. Current opinion in rheumatology. 2017 Jul;29(4):317.</ref> | |||
Axial spondyloarthritis is used to describe patients who have both non-radiographic and radiographic axial spondyloarthritis. Non-radiographic axial spondyloarthritis does not show on x-ray, but there are changes on MRI.<ref name=":5">Martey C. [https://members.physio-pedia.com/learn/overview-of-spondyloarthropathies/ Overview of Spondyloarthropathies Course]. Plus2020.</ref> Radiographic axial spondyloarthritis is also known as ankylosing spondylitis (AS).<ref name=":7">Sieper J, Poddubnyy D. [https://www.sciencedirect.com/science/article/pii/S0140673616315914 Axial spondyloarthritis]. The Lancet. 2017 Jul 1;390(10089):73-84.</ref> | |||
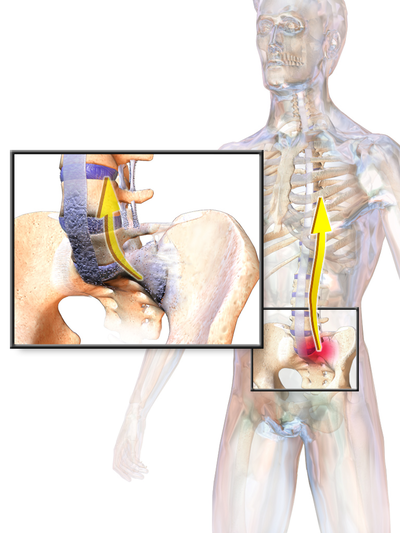
Axial spondyloarthritis predominantly affects the spine, with inflammatory changes causing pain, stiffness and a loss of motion in the back.<ref>Martey C. [https://members.physio-pedia.com/learn/overview-of-spondyloarthropathies/ Overview of Spondyloarthropathies Course]. Plus2020.</ref><ref>Wenker KJ, Quint JM. Ankylosing Spondylitis. [Updated 2020 Jul 13]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470173/</ref> It often causes changes in the [[Sacroiliac Joint|sacroiliac joint]]<nowiki/>s, apophyseal joints, costovertebral joints, and intervertebral disc articulations. It causes characteristic [[Differentiating Inflammatory and Mechanical Back Pain|inflammatory back pain]], resulting in structural and functional impairments and a reduction in quality of life.<ref name="p8">Laura A, Haftel H. Shoulder, Knee, and Hip Pain as Initial Symptoms of Juvenile Ankylosing Spondylitis: A Case Report, Journal of Orthopaedic & Sports Physical Therapy [Internet], 1998Feb [cited 2020 Oct 4];27(2):167–172. Available from https://www.jospt.org/doi/10.2519/jospt.1998.27.2.167</ref><ref name="p0">Giles L, Singer K. The clinical anatomy and management of back pain series, Volume 2 Clincal Anatomy and Management of Thoracic Spine Pain, Butterworth Heinemann, 2000: 61-66.</ref><ref name="p1">Mills K, Page G, Siwek R. A color atlas of low back pain. London:Wolfe Medical Publications,1990. </ref><ref name="p2">Andersson GB, McNeill TW. [https://books.google.com/books?hl=en&lr=&id=U86oBgAAQBAJ&oi=fnd&pg=PT12&dq=Andersson+G,%C2%A0McNeill+T.+Lumbar+spine+syndromes,+evaluation+and+treatment.+New+York:+Springer-Verlag+Wien,1989:180-181.&ots=wp6K8wPp59&sig=WgxWR7WHwu0SQEKAuBG3Zl_GwbU Lumbar spine syndromes: Evaluation and treatment]. Springer Science & Business Media; 2012 Dec 6. </ref> Affected joints progressively become stiff and sensitive due to a bone formation at the level of the joint capsule and cartilage. It causes a decreased range of motion and, in its advanced stages, can give the spine an appearance similar to bamboo, hence the alternative name "bamboo spine". | |||
Although not often recognised, axial spondyloarthritis can also cause peripheral joint pain, particularly in the hips, knees, ankles, and shoulders and neck. It involves synovial and cartilaginous joints, as well as sites of tendon and ligamentous attachment.<ref name="p0" /><ref name="p2" /> Early diagnosis and treatment help to control the pain and stiffness and may reduce or prevent significant deformity.<ref name=":1" /> | |||
== Clinically Relevant Anatomy == | == Clinically Relevant Anatomy == | ||
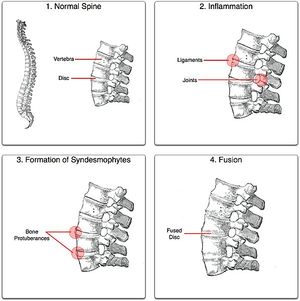
Pain in AS can be caused by [[sacroiliitis]], enthesitis, and spondylitis.<ref name="p8" /> Initially, the sacroiliac joints, situated in the lumbar part of the back, which connect the spine and the pelvis, are damaged. Subsequently, the inflammation moves to entheses, where ligaments and tendons integrate into the bone. | Pain in AS can be caused by [[sacroiliitis]], enthesitis, and spondylitis.<ref name="p8" /> Initially, the sacroiliac joints, situated in the lumbar part of the back, which connect the spine and the pelvis, are damaged. Subsequently, the inflammation moves to entheses, where ligaments and tendons integrate into the bone. Eventually, the spine is affected by this inflammation. The vertebral column normally exists of 24 vertebrae, joined together by ligaments and separated by intervertebral discs. <br>Patients diagnosed with AS form calcium deposits in the ligaments between and around the intervertebral discs. An accumulation of the deposits leads to ossification <ref name="p0" />, starting from the vertebral rim towards the annulus fibrosis and characterised by syndesmophytes.<ref name="p1" /> '''Syndesmophytes''' are one of the main features of spinal structural damage in ankylosing spondylitis.<ref>Tan S, Wang R, Ward MM. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4478446/ Syndesmophyte growth in ankylosing spondylitis.] Current opinion in rheumatology. 2015 Jul;27(4):326.</ref> It is a osseous excrescences or bony outgrowths from the spinal ligaments as they attach to adjacent vertebral bodies.<ref>[https://www.ncbi.nlm.nih.gov/medgen/780898#:~:text=Definition,and%20bridge%20adjacent%20vertebrae%20asymmetrically. Syndesmophytes]. National Library of Medicine</ref> In highly advanced cases, the spine can fuse together as a result of the bone formation.<br> | ||
== Epidemiology /Etiology == | == Epidemiology /Etiology == | ||
[[File:Ankylosing process.jpg|right|frameless]] | [[File:Ankylosing process.jpg|right|frameless]] | ||
AS Affects 0.1 to 1.4% of the population | AS Affects 0.1 to 1.4% of the population.<ref name=":2">Dean L, Jones G, MacDonald A, Downham C, Sturrock R, Macfarlane G. Global prevalence of ankylosing spondylitis. Rheumatology [Internet]. 2014 Apr [cited 2020 Sep 26]; 53(4), 650–657. Available from https://academic.oup.com/rheumatology/doi.org/10.1093/rheumatology/ket387 | ||
</ | </ref> There is a male to female ratio of 2:1 for radiographic axial spondyloarthritis and of 1:1 for non-radiographic axial spondyloarthritis.<ref name=":7" /> The onset of symptoms generally occurs between 20-40 years of age.<ref name=":2" /> Less than 5% of cases have an onset of symptoms over the age of 45.<ref name=":2" /> AS is more prevalent within Europe (mean 23.8 per 10,000) and Asia (mean 16.7 per 10,000) than within Latin America (mean 10.2 per 10,000).<ref name=":2" /> | ||
The etiology of AS is not fully understood. Although a strong link has been established of complex interactions between genetic background and environmental factors.<ref name=":3">Watad A, Bridgewood C, Russell T, Marzo-Ortega H, Cuthbert R, McGonagle D. T[https://www.frontiersin.org/articles/10.3389/fimmu.2018.02668/full he early phases of ankylosing spondylitis: emerging insights from clinical and basic science.] Frontiers in immunology. 2018:2668.</ref> Studies have shown factors such as genetic background gene called ( HLA-B27), microbial infection, endocrinal abnormalities and immune reaction related to the occurrence of AS.<ref name=":3" /> In addition, a direct relationship between AS and the major histocompatibility human leukocyte antigen (HLA)-B27 has also been determined.<ref name=":3" /><ref name="p3">Alvarez I, López de Castro JA. HLA-B27 and immunogenetics of spondyloarthropathies. Curr Opin Rheumatol. 2000;12(4):248-253 | |||
Alvarez I, de Castro JA. [https://journals.lww.com/co-rheumatology/Fulltext/2000/07000/HLA_B27_and_immunogenetics_of.3.aspx HLA-B27 and immunogenetics of spondyloarthropathies]. Current opinion in rheumatology. 2000 Jul 1;12(4):248-53.</ref> The exact role of this antigen is unknown but is believed to act as a receptor for an inciting antigen leading to AS. HLA-B27 occurs in 90-95% of patients with ankylosing spondylitis, compared to a 6 to 9% incidence in the normal population. <ref name="p2" /> Environmental or bacterial factors can also be a trigger. <ref name="p9">Braggins S. Back care: a clinical approach. Churchill Livingstone; 2000. </ref> | |||
Initially, there is an infiltration of the subchondral bone by granulation tissue which causes small lesions, ultimately leading to joint erosion (the adjacent cartilage is distorted which produces a very irregular surface).<ref name="p2" /> These lesions in the annulus eventually undergo ossification, leading to a fusion effect of the spinal segments and the similarity in appearance to bamboo. In the spine, this occurs at the junction of the vertebrae and the annular fibres of the intervertebral disc. | |||
When synovium is the affected tissue, there is an infiltration by macrophages and lymphocytes. This is followed by replacement of the cartilage or fibrous tissue by a scar-like fibroblast invasion which rapidly ossifies. The inflammatory response in the bone adjacent to the involved fibrocartilage, ligament or periosteum is frequently quite severe. The spine can resemble an infectious discitis when the spine is initially involved, which can be an additional source of confusion for the treating therapist. <ref name="p2" /><br> | |||
== Characteristics/Clinical Presentation of Inflammatory back pain == | |||
Inflammatory back pain should be considered if two or more of the following features are present. Additionally, the presence of four or features is considered diagnostic.<ref name=":4">Taurog JD, Chhabra A, Colbert RA. [https://www.nejm.org/doi/full/10.1056/NEJMra1406182 Ankylosing spondylitis and axial spondyloarthritis.] New England Journal of Medicine. 2016 Jun 30;374(26):2563-74.</ref>[[File:Ankylosing spondylitis lumbar spine.jpg|right|frameless]] | |||
*Insidious onset of back pain in the sacroiliac (SI) joints and gluteal regions (presenting as alternating buttock pain), which progress to involve the entire spine<ref name="p42">Baaj A, Praveen V, Mummaneni S, Uribe R, Vaccaro S, Mark S. Handbook of spine surgery. New York:Thieme, 2010:180-182.</ref> | |||
[[File:Ankylosing spondylitis lumbar spine.jpg|right|frameless]] | *Age of onset less than 45 years | ||
* Insidious onset of back pain in the sacroiliac (SI) joints and gluteal regions | *Duration of more than 3 months | ||
* Morning stiffness lasting greater than 30 minutes | *Morning stiffness lasting greater than 30 minutes | ||
* Waking up in the second half of the night | *Waking up in the second half of the night due to pain, but eases with arising | ||
* Pain and stiffness increase with inactivity and improve with exercise | *Pain and stiffness increase with inactivity and improve with exercise<ref name=":4" /><ref name="p23">Andersson GB, McNeill TW. [https://books.google.com/books?hl=en&lr=&id=U86oBgAAQBAJ&oi=fnd&pg=PT12&dq=Andersson+G,%C2%A0McNeill+T.+Lumbar+spine+syndromes,+evaluation+and+treatment.+New+York:+Springer-Verlag+Wien,1989:180-181.&ots=wp6K8wQn8i&sig=fFnTeRW8KU5ePkZzLFdjBVZk9HI Lumbar spine syndromes: Evaluation and treatment]. Springer Science & Business Media; 2012 Dec 6.</ref> | ||
* Involvement of peripheral joints, eyes, skin, and the cardiac and intestinal systems | *The patient is a young adult 15-30 years old male, presenting with a gradual onset of pain and stiffness of the lower back. | ||
* Complaints of intermittent breathing difficulties | *Initially, the stiffness may be noticed only after a period of rest, and improves with movement. | ||
* Intermittent low-grade fever, fatigue, or weight loss can occur | *Pain tends to be worst at night or early morning, awakening the patient from sleep. | ||
More specific to AS the following clinical features may be described: | |||
*Involvement of peripheral joints, eyes, skin, and the cardiac and intestinal systems<ref name="p42" /> | |||
**Eye disease occurs in about 25% of the patients as either iridocyclitis or conjunctivitis<ref name="p23" /> | |||
**Joints other than those of the axial skeleton can be involved with inflammatory arthritis and synovitis. The hips, shoulder and knees are commonly and most severely affected of the extremity joints<ref name="p23" /> | |||
*Complaints of intermittent breathing difficulties due to a reduction in chest expansion. This reduction in chest wall excursion, notably less than 2 cm, can be a characteristic of AS because chest wall excursion is an indicator of decreased axial skeleton mobility<ref name="p222">Kataria RK, Brent LH. [https://www.aafp.org/afp/2004/0615/p2853 Spondyloarthropathies]. American family physician. 2004 Jun 15;69(12):2853-60.</ref> | |||
*Intermittent low-grade fever, fatigue, or weight loss can occur<ref name="p122">Goodman Catherine C, Snyder TE. Differential diagnosis for physical therapists: screening for referral. St. Louis: Saunders Elsevier. 2007.</ref> | |||
== Differential Diagnosis == | == Differential Diagnosis == | ||
| Line 38: | Line 52: | ||
* [[Degenerative Disc Disease]] | * [[Degenerative Disc Disease]] | ||
* Herniated Intervertebral Disc | * Herniated Intervertebral Disc | ||
* Fractures and/or dislocation | * [[Fracture|Fractures]] and/or dislocation | ||
* [[Osteoarthritis]] | * [[Osteoarthritis]] | ||
* [[Lumbar Spinal Stenosis|Spinal Stenosis]] | * [[Lumbar Spinal Stenosis|Spinal Stenosis]] | ||
| Line 44: | Line 58: | ||
* [[Reactive Arthritis|Reactive arthritis]] | * [[Reactive Arthritis|Reactive arthritis]] | ||
* Inflammatory bowel-related arthritis | * Inflammatory bowel-related arthritis | ||
* Diffuse idiopathic skeletal hyperostosis (DISH) | * [[Diffuse Idiopathic Skeletal Hyperostosis|Diffuse idiopathic skeletal hyperostosis (DISH)]] | ||
* [[Rheumatoid Arthritis|Rheumatoid arthritis]] <ref name="p4" /> | * [[Rheumatoid Arthritis|Rheumatoid arthritis]] <ref name="p4">Baaj A, Praveen V, Mummaneni S, Uribe R, Vaccaro S, Mark S. Handbook of spine surgery. New York:Thieme, 2010:180-182. </ref> | ||
* [[Psoriatic Arthritis|Psoriatic arthritis]] <ref name="p4" /> | * [[Psoriatic Arthritis|Psoriatic arthritis]] <ref name="p4" /> | ||
* [[ | * [[Reactive Arthritis|Reiter's syndrome]] (milder with asymmetric sacroiliitis) <ref name="p4" /> | ||
== Diagnostic Procedures == | == Diagnostic Procedures == | ||
The diagnosis of AS is commonly made through a combination of thorough subjective and physical examinations, laboratory data and imaging studies. Common laboratory data include blood tests to determine the presence of the HLA-B2 antigen or substances that indicate an inflammatory process: <ref name="p6">Mandl P. | The diagnosis of AS is commonly made through a combination of thorough subjective and physical examinations, laboratory data and imaging studies. Common laboratory data include blood tests to determine the presence of the HLA-B2 antigen or substances that indicate an inflammatory process: <ref name="p6">Mandl P, Navarro-Compán V, Terslev L, Aegerter P, Van Der Heijde D, D'Agostino MA, Baraliakos X, Pedersen SJ, Jurik AG, Naredo E, Schueller-Weidekamm C. [https://ard.bmj.com/content/74/7/1327.short EULAR recommendations for the use of imaging in the diagnosis and management of spondyloarthritis in clinical practice]. Annals of the rheumatic diseases. 2015 Jul 1;74(7):1327-39. </ref> | ||
=== Criteria to assist diagnosis in Primary care === | === Criteria to assist diagnosis in Primary care === | ||
* Peripheral manifestations, such as dactylitis | * Peripheral manifestations, such as dactylitis, enthesitis or arthritis, especially of the plantar fascia or Achilles tendon | ||
* A family history of AS or related | * A family history of AS or related disorders. A first-degree or second-degree relative with ankylosing spondylitis, psoriasis, uveitis, reactive arthritis or inflammatory bowel disease | ||
* Inflammatory back pain | * Inflammatory back pain symptoms | ||
* Psoriasis, inflammatory bowel disease or a history of uveitis | * Psoriasis, inflammatory bowel disease or a history of uveitis | ||
* Elevated C-reactive protein (CRP), where causes such as spinal infection or cancer have been excluded. This is also a marker of inflammation and is found in 50-70% of people with AS.<ref name="p6" /> Patients with AS may have CRP levels ranging from > 6 mg/L (slightly elevated) to 20 – 30 mg/L | * Elevated C-reactive protein (CRP), where causes such as spinal infection or cancer have been excluded. This is also a marker of inflammation and is found in 50-70% of people with AS.<ref name="p6" /> Patients with AS may have CRP levels ranging from > 6 mg/L (slightly elevated) to 20 – 30 mg/L | ||
* Back pain which improves after 24 – 48 hours of treatment with non-steroidal anti-inflammatory | * Back pain which improves after 24 – 48 hours of treatment with non-steroidal anti-inflammatory | ||
* Positive HLA-B27 test: HLA B27 is positive in 80-90% of AS patients, more so in the Caucasian population and African Americans. <ref name="p8" /> The HLA-B27 antigen is also present in other inflammatory conditions of intestines or joints | * Positive HLA-B27 test: HLA B27 is positive in 80-90% of AS patients, more so in the Caucasian population and African Americans. <ref name="p8" /> The HLA-B27 antigen is also present in other inflammatory conditions of intestines or joints | ||
* Sacroiliitis on X-ray or MRI | * Sacroiliitis on X-ray or MRI | ||
* Erythrocyte sedimentation rate (ESR): This is a blood test for inflammation, in approximately one-third of the | * Erythrocyte sedimentation rate (ESR): This is a blood test for inflammation, in approximately one-third of the AS patients there is a raised ESR observable in exacerbations of the disease, but other conditions can also cause a high ESR<ref name="p1" /><ref name="p6" /> | ||
< | Laboratory tests are specific and often more helpful to exclude other diagnoses rather than confirming AS. In combination with other clinical symptoms, the diagnosis can often be made more accurate. <ref name="p8" /><ref name="p1" /> | ||
=== Detection of AS by Medical Imaging === | |||
*X-rays have traditionally been considered the most useful imaging modality in established disease, although they may be normal in the early phases<ref name="p6" />[[File:Spondy 1.png|right|frameless]]X-ray shows up areas where the bone has been worn away by the condition. The vertebrae of the spine may start to fuse together because the ligaments between them become calcified.<ref name="p6" />Early X-ray changes are vertebral body squaring following erosion of anterior column of spine. The '''shiny corner sign''' is a spinal finding in ankylosing spondylitis, representing reactive sclerosis secondary to inflammatory erosions at the superior and inferior endplates (corners on lateral radiograph) of the vertebral bodies which are known as '''Romanus lesions.'''<ref>Shiny corner sign (ankylosing spondylitis).Available from: https://radiopaedia.org/articles/shiny-corner-sign-ankylosing-spondylitis#:~:text=The%20shiny%20corner%20sign%20is,are%20known%20as%20Romanus%20lesions.</ref> | |||
*MRI scanning is also used to detect inflammation on MRI that is suggestive of sacroiliitis.<ref>Slobodin G, Eshed I. [https://www.ima.org.il/imaj/ViewArticle.aspx?aId=3798 Non-radiographic axial spondyloarthritis]. Isr Med Assoc J. 2015 Dec 1;17(12):770-6.</ref> MRI of the sacroiliac joints is more sensitive than either plain X-ray or CT scan in demonstrating [[sacroiliitis]]. Sacroiliitis initially shows as blurring in the lower part of the joint, then bony erosions or sclerosis occur and widening or eventual fusion of the joint<ref name="p6" /> | |||
*Vertebral body squaring<ref name="p6" /> | |||
*Bamboo spine appearance<ref name="p6" /> | |||
*Dagger sign: central dense line seen on AP radiography of spine and pelvis following ossification of supraspinous and interspinous ligaments<ref name="p6" /> | |||
*Tram- track sign: Ossification of the apophyseal joint capsules forming two vertical radiodense lines lateral to this central line on frontal view | |||
*Trolley-track sign: combining a central “dagger” sign and a peripheral tram-like track<ref>Lambrecht V, Vanhoenacker FM, Van Dyck P, Gielen J, Parizel PM. [https://www.researchgate.net/publication/7944099_Ankylosing_spondylitis_what_remains_of_the_standard_radiography_anno_2004 Ankylosing spondylitis: what remains of the standard radiography anno 2004.] JBR-BTR. 2005;88(1):25-30.</ref> | |||
*Hatchet deformity<ref name="p6" /> | |||
*Subchondral erosions, sclerosis and proliferation on iliac side of SI joints<ref name="p6" /> | |||
*Bridging or fusion of the pubic symphysis<ref name="p6" /> | |||
= | <br>The modified New York Classification Criteria (mNYCC) was previously used to diagnose axial spondyloarthritis.<ref name=":6" /> The mNYCC combines clinical findings with radiograph studies. Radiographic findings are graded on a scale of 0 to 4 where 0 represents normal findings and 4 represents complete ankylosis.<ref name="p8" /> A definitive diagnosis is considered with the following radiographic combinations:<ref name=":8">Linden SV, Valkenburg HA, Cats A. [https://onlinelibrary.wiley.com/doi/abs/10.1002/art.1780270401 Evaluation of diagnostic criteria for ankylosing spondylitis]. Arthritis & Rheumatism. 1984 Apr;27(4):361-8.</ref> | ||
*Grade 3 or 4 at bilateral SI joints on radiograph with at least one clinical finding | |||
*Grade 3 or 4 unilaterally (or Grade 2 bilaterally) with two clinical findings | |||
The patient must also fulfil at least one of the following clinical criteria:<ref name=":8" /> | |||
* Low back pain and stiffness for at least 3 months, which improves with exercise, but is not relieved by rest | |||
* Limited lumbar spinal motion in sagittal (sideways) and frontal (forward and backward) plane | |||
* Chest expansion decreased relative to normal values corrected for age and sex | |||
Grading | |||
* A patient can be classified as having definite AS if at least 1 clinical criterion plus the radiologic criterion are fulfilled | |||
* A probable diagnosis of AS is made if three clinical criteria are present or the radiologic criterion is present without any signs or symptoms satisfying the clinical criteria | |||
==== Ankylosing Spondylitis and Axial Spondyloarthritis ==== | |||
The modified New York criteria (1984) are somewhat specific, they were found to be insensitive for the determination of early disease. Furthermore, large intraobserver and interobserver disparity in diagnosis further drives the dependency on plain radiographs of the sacroiliac joints. Inflammation of the sacroiliac joints can be identified on MRI in patients with symptoms of AS, even when these joints do not seem to be abnormal on traditional radiography. The same MRI techniques also show spinal inflammation in many patients. The detection of these conditions on MRI resulted in the creation of "axial spondyloarthritis" (see definition / description section above). This diagnosis encompassed patients with definite AS and patients with symptoms alike to those of AS and findings of sacroiliitis on MRI, but without advanced sacroiliitis on traditional radiography.<ref name=":4" /> | |||
In 2009, the Assessment of SpondyloArthritis International Society (ASAS) developed classification criteria for axial spondyloarthritis that are supported on these imaging, clinical, and laboratory criteria. Implementing these criteria, the diagnosis is established in persons who have had back pain for 3 or more sequential months prior reaching 45 years of age, with the presence of sacroiliitis confirmed on MRI or plain radiography, and have a minimum of one clinical or laboratory finding that is characteristic of spondyloarthritis. Alternatively, individuals with this history who have a positive test result for HLA-B27 and two symptoms of spondyloarthritis, as identified on clinical examination or laboratory analysis will also meet the criteria for a diagnosis of axial spondyloarthritis.<ref name=":4" /> | |||
In summary, as stated by the ASAS criteria, the diagnosis of axial spondyloarthritis comprise two subsets — nonradiographic axial spondyloarthritis and classic ankylosing spondylitis (that is radiographic axial spondyloarthritis).<ref name=":4" /> | |||
== Outcome Measures == | == Outcome Measures == | ||
* [[Schober Test|Schober Test]] | * [[Schober Test|Schober Test]] | ||
* [[Occiput to Wall Distance OWD|Occiput to Wall Distance]] (Flesche test) | |||
* [[Oswestry Disability Index|Oswestry Disability Index]] (ODI) | * [[Oswestry Disability Index|Oswestry Disability Index]] (ODI) | ||
* [[Neck Disability Index]] (NDI) | * [[Neck Disability Index]] (NDI) | ||
* [[Visual Analogue Scale]] | * [[Visual Analogue Scale]] | ||
* [[Patient Specific Functional Scale]] | * [[Patient Specific Functional Scale]] | ||
Evaluation Scales | |||
* Bath Ankylosing Spondylitis Metrology Index (BASMI) | ===== Evaluation Scales ===== | ||
* Revised Leeds Disability Questionnaire (RLDQ) | * Bath Ankylosing Spondylitis Metrology Index (BASMI)<ref name="p7">Jordan CL, Rhon DI. [https://www.jospt.org/doi/abs/10.2519/jospt.2012.4050 Differential diagnosis and management of ankylosing spondylitis masked as adhesive capsulitis: a resident's case problem]. journal of orthopaedic & sports physical therapy. 2012 Oct;42(10):842-52. </ref><ref name=":1" /> | ||
* European Quality of Life (EuroQoL) | * Revised Leeds Disability Questionnaire (RLDQ)<ref name=":1" /> | ||
* Bath AS Disease Activity Index (BASDAI; 0-100) | * European Quality of Life (EuroQoL)<ref name=":1" /> | ||
Laboratory values, such as the CRP, are used to monitor the effectiveness of medication treatments. | * Bath AS Disease Activity Index (BASDAI; 0-100)<ref name="p7" /><ref name=":1" /> | ||
* AMOR criteria for Spondyloarthritis<ref name="p7" /> | |||
*BASFI index ( Bath Ankylosing Spondylitis Functional Index)<ref name="p7" /> | |||
*BAS-G index ( Bath Ankylosing Spondylitis Global Index)<ref name="p7" /> | |||
Laboratory values, such as the C-Reactive Protein(CRP), are used to monitor the effectiveness of medication treatments. | |||
== Examination == | == Examination == | ||
A thorough physical examination, particularly of the musculoskeletal system, is needed. Clinical signs are sometimes minimal in the early stages of the disease. Examination of the sacroiliac joints and the spine (including the neck), measurement of chest expansion and range of motion of the hip and shoulder joints, and a search for signs of enthesitis are critical in making an early diagnosis of AS. <ref name="p2" /><ref name="p5">Bullough | A thorough physical examination, particularly of the musculoskeletal system, is needed. Clinical signs are sometimes minimal in the early stages of the disease. Examination of the sacroiliac joints and the spine (including the neck), measurement of chest expansion and range of motion of the hip and shoulder joints, and a search for signs of enthesitis are critical in making an early diagnosis of AS. <ref name="p2" /><ref name="p5">Bullough G, Boachie-Adjei O. Atlas of spinal diseases. Hampshire:Gower Medical Publishing, 1987. </ref><ref name="p8" /> | ||
Video 1: The aim of the [[Schober Test]] is to assess the mobility of the lumbar spine, which can be abnormal even when it is not obvious to the individual. | Video 1: The aim of the [[Schober Test]] is to assess the mobility of the lumbar spine, which can be abnormal even when it is not obvious to the individual. | ||
| Line 137: | Line 148: | ||
Video 4: The tragus to wall test is a test to measure the cervical mobility. | Video 4: The tragus to wall test is a test to measure the cervical mobility. | ||
{{#ev:youtube|9-SvI4disNE|350}} | {{#ev:youtube|9-SvI4disNE|350}} | ||
There are certain special tests for detecting the involvement of sacro-iliac joint includes- | |||
-Sacro-iliac compression: Direct side to side compression of the pelvis in supine lying may cause pain at the sacro-iliac joints or promoting compression of the symptomatic pelvis in side lying may cause pain. {{#ev:youtube|pWjvrhWMR4w}}<ref>Physiotutors. Compression Test / Side-lying Compression | Sacroiliac Joint Provocation. Available from youtube.com/watch?v=pWjvrhWMR4w (last accessed on 20/7/2023</ref> | |||
-Gaenslen's test: The hip and the knee joints of the opposite side are flexed to fix the pelvis, and the hip joint of the side under test is hyperextended over the edge of the table. This will exert a rotational strain over the sacro-iliac joint and give rise to pain.{{#ev:youtube|ED_bYoQk9d4}}<ref>Physiotutors. Gaenslen's Test | Sacroiliac Joint Provocation. Available from https://www.youtube.com/watch?v=ED_bYoQk9d4 (last accessed on 20/7/2023</ref> | |||
--Straight leg raising test: The patient is asked to lift the leg up with the knee extended. This will cause pain at the affected sacro- iliac joint.{{#ev:youtube|LdAD9GNv8FI}}<ref>Physiotutors. Straight Leg Raise or Lasègue's Test for Lumbar Radiculopathy. Available from https://www.youtube.com/watch?v=LdAD9GNv8FI (last accessed on 20/7/2023)</ref> | |||
== Complications == | |||
* Fractures following minor trauma due to osteoporosis, usually compression fractures | |||
* Uveitis | |||
* Reduced flexibility | |||
* Pulmonary function restrictions | |||
* Increased risk of heart diseases (aortic insufficiency, aortitis, angina, pericarditis, and cardiac conduction abnormalities) | |||
* Fatigue | |||
* Gastrointestinal disorders | |||
== Medical Management == | == Medical Management == | ||
| Line 153: | Line 183: | ||
==== Biphosphonates ==== | ==== Biphosphonates ==== | ||
Biphosphonates have good outcomes on bone turnover, which is positive as ankylosing spondylitis is characterised by bone resorption and formation. Neridronate and pamidronate are amino-biphosphonates with similar effects as the TNF inhibitor Infliximab. <ref name="p6" / | Biphosphonates have good outcomes on bone turnover, which is positive as ankylosing spondylitis is characterised by bone resorption and formation. Neridronate and pamidronate are amino-biphosphonates with similar effects as the TNF inhibitor Infliximab. <ref name="p6" /> All drugs have side effects, so patients with other health issues need to verify if they are able to take the recommended medicines. | ||
== | == Physiotherapy Management == | ||
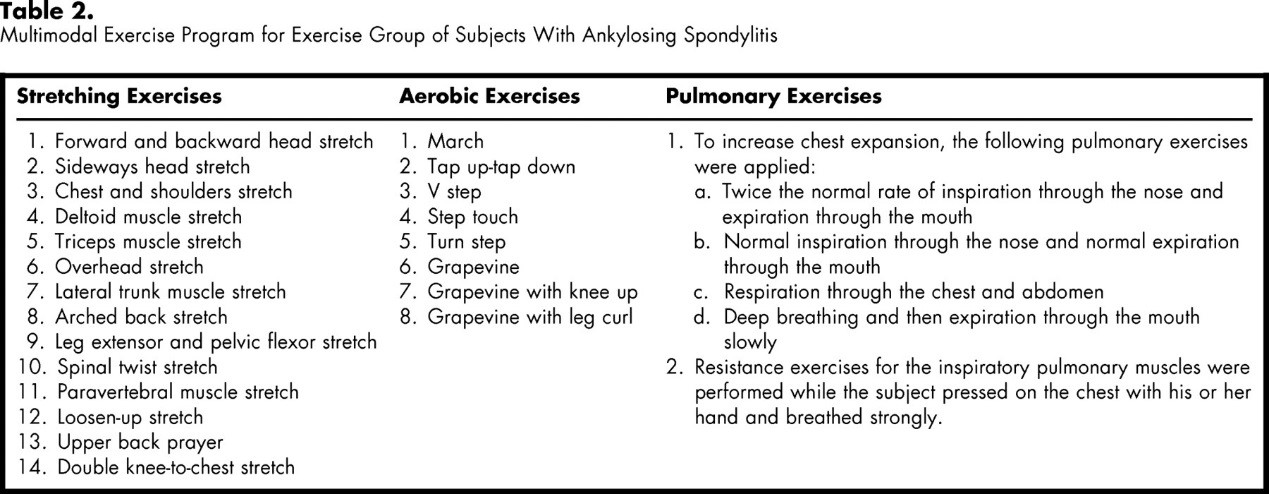
Physiotherapy is an essential part of the treatment of AS.<ref name="p0" /> It aims to alleviate pain, increase spinal mobility and functional capacity, reduce morning stiffness, correct postural deformities, increase mobility and improve the psychosocial status of the patients. According to a Cochrane review completed by Dagfinrud and colleagues, a supervised or individual home-based exercise program is better than no intervention,<ref name=":1">Nava T. Physiotherapy rehabilitation in patients with ankylosing spondylitis. Beyond Rheumatol [Internet]. 2019 Dec 20 [cited 2020 Sep 26];1(2):37-6. Available from: http://beyond-rheumatology.org/index.php/br/article/view/6</ref> The main aspects of rehabilitation include education, a program of personalised exercises and outline of physical activities to be completed at home or in a group based environment.<ref name=":1" /> | |||
=== Education === | === Education === | ||
According to a study | According to a study conducted by Sweeney and colleagues, education into long term home self-care has proven to be effective.<ref name=":1" /> Studies have highlighted how limited education and information can result in poor adherence to rehabilitation.<ref name=":1" /> Self care and educational packages including education booklets and videos, reminder stickers and progression charts.<ref name=":1" /> The failure or success of exercise programs is determined by compliance with the prescribed program, which requires motivation, participation and time. This can be monitored using patient diaries or physiotherapist records.<ref name=":1" /> | ||
<br> | |||
[[Image:Table of AS Exs.jpg]]<br> | [[Image:Table of AS Exs.jpg]]<br> | ||
== Treatment Phase == | == Treatment Phase == | ||
=== Initial/Acute Phase === | === Initial/Acute Phase === | ||
The initial phase of AS is | The initial phase of AS is characterised by morning stiffness and pain in the spine.<ref name=":1" /> | ||
==== Primary Objective ==== | ==== Primary Objective ==== | ||
* | * Control of the diffuse and intense pain secondary to joint stiffness,<ref name=":1" /> | ||
** | ** Recovery of proprioception, joint stability, restoring normal postural patterns and reduction of pain<ref name=":1" /> | ||
* | * Interventions for pain management along with pharmacological treatment prevents compensatory postures<ref name=":1" /> | ||
==== Secondary Objective ==== | ==== Secondary Objective ==== | ||
* | * Maintain the elasticity of the pelvis and spine to enable good respiratory function<ref name=":1" /> | ||
=== Remission Phase === | === Remission Phase === | ||
The remission phase of AS is | The remission phase of AS is characterised by pain, restricted mobility of the spine +/- peripheral joints<ref name=":1" /> | ||
==== Primary Objective ==== | ==== Primary Objective ==== | ||
| Line 277: | Line 223: | ||
* To enable the patient to maintain their residual function to guarantee the most autonomy possible. | * To enable the patient to maintain their residual function to guarantee the most autonomy possible. | ||
** Education on the importance of physiotherapy and body awareness is key in this phase of AS. | ** Education on the importance of physiotherapy and body awareness is key in this phase of AS. | ||
** In-clinic sessions with manual therapy | ** In-clinic sessions with manual therapy are essential to enable the patient to continue their home exercise program.<ref name=":1" /> | ||
== Considerations for | == Considerations for Physiotherapy Management == | ||
Fatigue is a common complain in rheumatological conditions. It can be managed by taking regular microbreaks, avoiding sitting in the same position for long | * Fatigue is a common complain in rheumatological conditions. It can be managed by taking regular microbreaks, avoiding sitting in the same position for long periods, maintaining physical activity and having good sleep hygiene. | ||
* AS patients can suffer from flare-ups of increased disease activity, which can last from days to weeks. During the flare-up the patient may benefit from gentle stretching exercise, taking breaks and medications. | |||
AS patients can suffer from flare-ups of increased disease activity, which can last from days to weeks. During the flare-up the patient may benefit from gentle stretching exercise, taking breaks and medications. | * [[Joint Protection Principles|Joint protection management]] applies the ergonomic principles to ADL activities to preserve the functional ability. | ||
* Patient compliance can be achieved by determining the barriers facing the individual, including the patient’s exercise preference in the program, using different exercise varieties to avoid boredom and group therapy. | |||
[[Joint Protection Principles|Joint protection management]] applies the | * Educating the patient about his condition and how to manage it, besides having a patient-provider relationship are important for patients’ self managing. | ||
* ADL activities can be made easier using assistive devices and alternative techniques. For example, managing shoes; slip-on shoes can be used or the patient can raise their leg on a stool or place it on the opposite knee. Driving can be difficult due to neck pain and stiffness, advice for driving can include taking breaks on long journeys and using a small pillow behind their back or under their buttock to promote better [[posture]].<ref name=":0">[https://www.physio-pedia.com/images/a/a4/Ankylosing_Spondylitis.pdf Living with a Chronic Disease – The Story of Ankylosing Spondylitis] </ref> | |||
Patient compliance can be achieved by determining the barriers facing the individual, including the patient’s exercise preference in the program, using different exercise varieties to avoid boredom and group therapy. | |||
Educating the patient about his condition and how to manage it, besides having a patient-provider relationship are important for patients’ self managing. | |||
ADL activities can be made easier using assistive devices and alternative techniques. For example, | |||
Driving can be difficult | |||
== Clinical Bottom Line == | == Clinical Bottom Line == | ||
Axial spondyloarthritis is a chronic inflammatory rheumatic disease with unknown etiology. Affected joints progressively become stiff and sensitive due to a bone formation at the level of the joint capsule and cartilage. This can lead to structural and functional impairments and a decrease in quality of life. Regions most affected by the disease are the axial skeleton and sacroiliac joints. A combination of medicines (such as non-steroidal anti-inflammatory drugs and biological medications) and physical therapy is recommended. Physiotherapy primarily consists of range of motion and respiratory exercises as well as working on postural corrections. | |||
== Resources == | == Resources == | ||
| Line 317: | Line 256: | ||
== References == | == References == | ||
<references /> | <references /> | ||
[[Category:Nottingham University Spinal Rehabilitation Project]] | [[Category:Nottingham University Spinal Rehabilitation Project]] | ||
[[Category:Rheumatology]] | [[Category:Rheumatology]] | ||
| Line 325: | Line 265: | ||
[[Category:Pelvis - Conditions]] | [[Category:Pelvis - Conditions]] | ||
[[Category:Autoimmune Disorders]] | [[Category:Autoimmune Disorders]] | ||
[[Category:Genetic Disorders]] | |||
Latest revision as of 11:38, 14 October 2023
Original Editor - Thomas Rodeghero Top Contributors - Laura Ritchie, Kalyani Yajnanarayan, Admin, Mathieu Henrotte, Vanwymeersch Celine, Jack Rubotham, Nikhil Benhur Abburi, Jacintha McGahan, Kim Jackson, Ajay Upadhyay, Rich Lee, Thomas Rodeghero, Rachael Lowe, Lucinda hampton, Anthony Willey, Scott Cornish, Lilian Ashraf, Jarapla Srinivas Nayak, Scott Buxton, Candace Goh, 127.0.0.1, Anouk Van den Bossche, Jess Bell, Niels Cloet, WikiSysop, Evan Thomas, Shaimaa Eldib, Sai Kripa, Sanne Peeten, Evelien De Wolf, Aminat Abolade, Els Bernaers, Neil Arun, Joshua Samuel, Vidya Acharya, Michelle Lee, Manisha Shrestha, Eva Devliegher, Tony Lowe and Venugopal Pawar
Definition/Description[edit | edit source]
Axial spondyloarthritis is a seronegative spondyloarthritis of the spine and pelvis. The term axial spondyloarthritis has only been used since 2009 when the Assessment of Spondyloarthritis International Society Axial Spondyloarthritis (ASAS) classification criteria was developed. The ASAS criteria allowed, for the first time, earlier identification of axial spondyloarthritis through magnetic resonance imaging (MRI).[1]
Axial spondyloarthritis is used to describe patients who have both non-radiographic and radiographic axial spondyloarthritis. Non-radiographic axial spondyloarthritis does not show on x-ray, but there are changes on MRI.[2] Radiographic axial spondyloarthritis is also known as ankylosing spondylitis (AS).[3]
Axial spondyloarthritis predominantly affects the spine, with inflammatory changes causing pain, stiffness and a loss of motion in the back.[4][5] It often causes changes in the sacroiliac joints, apophyseal joints, costovertebral joints, and intervertebral disc articulations. It causes characteristic inflammatory back pain, resulting in structural and functional impairments and a reduction in quality of life.[6][7][8][9] Affected joints progressively become stiff and sensitive due to a bone formation at the level of the joint capsule and cartilage. It causes a decreased range of motion and, in its advanced stages, can give the spine an appearance similar to bamboo, hence the alternative name "bamboo spine".
Although not often recognised, axial spondyloarthritis can also cause peripheral joint pain, particularly in the hips, knees, ankles, and shoulders and neck. It involves synovial and cartilaginous joints, as well as sites of tendon and ligamentous attachment.[7][9] Early diagnosis and treatment help to control the pain and stiffness and may reduce or prevent significant deformity.[10]
Clinically Relevant Anatomy[edit | edit source]
Pain in AS can be caused by sacroiliitis, enthesitis, and spondylitis.[6] Initially, the sacroiliac joints, situated in the lumbar part of the back, which connect the spine and the pelvis, are damaged. Subsequently, the inflammation moves to entheses, where ligaments and tendons integrate into the bone. Eventually, the spine is affected by this inflammation. The vertebral column normally exists of 24 vertebrae, joined together by ligaments and separated by intervertebral discs.
Patients diagnosed with AS form calcium deposits in the ligaments between and around the intervertebral discs. An accumulation of the deposits leads to ossification [7], starting from the vertebral rim towards the annulus fibrosis and characterised by syndesmophytes.[8] Syndesmophytes are one of the main features of spinal structural damage in ankylosing spondylitis.[11] It is a osseous excrescences or bony outgrowths from the spinal ligaments as they attach to adjacent vertebral bodies.[12] In highly advanced cases, the spine can fuse together as a result of the bone formation.
Epidemiology /Etiology[edit | edit source]
AS Affects 0.1 to 1.4% of the population.[13] There is a male to female ratio of 2:1 for radiographic axial spondyloarthritis and of 1:1 for non-radiographic axial spondyloarthritis.[3] The onset of symptoms generally occurs between 20-40 years of age.[13] Less than 5% of cases have an onset of symptoms over the age of 45.[13] AS is more prevalent within Europe (mean 23.8 per 10,000) and Asia (mean 16.7 per 10,000) than within Latin America (mean 10.2 per 10,000).[13]
The etiology of AS is not fully understood. Although a strong link has been established of complex interactions between genetic background and environmental factors.[14] Studies have shown factors such as genetic background gene called ( HLA-B27), microbial infection, endocrinal abnormalities and immune reaction related to the occurrence of AS.[14] In addition, a direct relationship between AS and the major histocompatibility human leukocyte antigen (HLA)-B27 has also been determined.[14][15] The exact role of this antigen is unknown but is believed to act as a receptor for an inciting antigen leading to AS. HLA-B27 occurs in 90-95% of patients with ankylosing spondylitis, compared to a 6 to 9% incidence in the normal population. [9] Environmental or bacterial factors can also be a trigger. [16]
Initially, there is an infiltration of the subchondral bone by granulation tissue which causes small lesions, ultimately leading to joint erosion (the adjacent cartilage is distorted which produces a very irregular surface).[9] These lesions in the annulus eventually undergo ossification, leading to a fusion effect of the spinal segments and the similarity in appearance to bamboo. In the spine, this occurs at the junction of the vertebrae and the annular fibres of the intervertebral disc.
When synovium is the affected tissue, there is an infiltration by macrophages and lymphocytes. This is followed by replacement of the cartilage or fibrous tissue by a scar-like fibroblast invasion which rapidly ossifies. The inflammatory response in the bone adjacent to the involved fibrocartilage, ligament or periosteum is frequently quite severe. The spine can resemble an infectious discitis when the spine is initially involved, which can be an additional source of confusion for the treating therapist. [9]
Characteristics/Clinical Presentation of Inflammatory back pain[edit | edit source]
Inflammatory back pain should be considered if two or more of the following features are present. Additionally, the presence of four or features is considered diagnostic.[17]
- Insidious onset of back pain in the sacroiliac (SI) joints and gluteal regions (presenting as alternating buttock pain), which progress to involve the entire spine[18]
- Age of onset less than 45 years
- Duration of more than 3 months
- Morning stiffness lasting greater than 30 minutes
- Waking up in the second half of the night due to pain, but eases with arising
- Pain and stiffness increase with inactivity and improve with exercise[17][19]
- The patient is a young adult 15-30 years old male, presenting with a gradual onset of pain and stiffness of the lower back.
- Initially, the stiffness may be noticed only after a period of rest, and improves with movement.
- Pain tends to be worst at night or early morning, awakening the patient from sleep.
More specific to AS the following clinical features may be described:
- Involvement of peripheral joints, eyes, skin, and the cardiac and intestinal systems[18]
- Complaints of intermittent breathing difficulties due to a reduction in chest expansion. This reduction in chest wall excursion, notably less than 2 cm, can be a characteristic of AS because chest wall excursion is an indicator of decreased axial skeleton mobility[20]
- Intermittent low-grade fever, fatigue, or weight loss can occur[21]
Differential Diagnosis[edit | edit source]
Common disorders to consider as differential diagnoses with AS are:
- Degenerative Disc Disease
- Herniated Intervertebral Disc
- Fractures and/or dislocation
- Osteoarthritis
- Spinal Stenosis
- Spondylolisthesis, Spondylolysis, and Spondylosis
- Reactive arthritis
- Inflammatory bowel-related arthritis
- Diffuse idiopathic skeletal hyperostosis (DISH)
- Rheumatoid arthritis [22]
- Psoriatic arthritis [22]
- Reiter's syndrome (milder with asymmetric sacroiliitis) [22]
Diagnostic Procedures[edit | edit source]
The diagnosis of AS is commonly made through a combination of thorough subjective and physical examinations, laboratory data and imaging studies. Common laboratory data include blood tests to determine the presence of the HLA-B2 antigen or substances that indicate an inflammatory process: [23]
Criteria to assist diagnosis in Primary care[edit | edit source]
- Peripheral manifestations, such as dactylitis, enthesitis or arthritis, especially of the plantar fascia or Achilles tendon
- A family history of AS or related disorders. A first-degree or second-degree relative with ankylosing spondylitis, psoriasis, uveitis, reactive arthritis or inflammatory bowel disease
- Inflammatory back pain symptoms
- Psoriasis, inflammatory bowel disease or a history of uveitis
- Elevated C-reactive protein (CRP), where causes such as spinal infection or cancer have been excluded. This is also a marker of inflammation and is found in 50-70% of people with AS.[23] Patients with AS may have CRP levels ranging from > 6 mg/L (slightly elevated) to 20 – 30 mg/L
- Back pain which improves after 24 – 48 hours of treatment with non-steroidal anti-inflammatory
- Positive HLA-B27 test: HLA B27 is positive in 80-90% of AS patients, more so in the Caucasian population and African Americans. [6] The HLA-B27 antigen is also present in other inflammatory conditions of intestines or joints
- Sacroiliitis on X-ray or MRI
- Erythrocyte sedimentation rate (ESR): This is a blood test for inflammation, in approximately one-third of the AS patients there is a raised ESR observable in exacerbations of the disease, but other conditions can also cause a high ESR[8][23]
Laboratory tests are specific and often more helpful to exclude other diagnoses rather than confirming AS. In combination with other clinical symptoms, the diagnosis can often be made more accurate. [6][8]
Detection of AS by Medical Imaging [edit | edit source]
- X-rays have traditionally been considered the most useful imaging modality in established disease, although they may be normal in the early phases[23]X-ray shows up areas where the bone has been worn away by the condition. The vertebrae of the spine may start to fuse together because the ligaments between them become calcified.[23]Early X-ray changes are vertebral body squaring following erosion of anterior column of spine. The shiny corner sign is a spinal finding in ankylosing spondylitis, representing reactive sclerosis secondary to inflammatory erosions at the superior and inferior endplates (corners on lateral radiograph) of the vertebral bodies which are known as Romanus lesions.[24]
- MRI scanning is also used to detect inflammation on MRI that is suggestive of sacroiliitis.[25] MRI of the sacroiliac joints is more sensitive than either plain X-ray or CT scan in demonstrating sacroiliitis. Sacroiliitis initially shows as blurring in the lower part of the joint, then bony erosions or sclerosis occur and widening or eventual fusion of the joint[23]
- Vertebral body squaring[23]
- Bamboo spine appearance[23]
- Dagger sign: central dense line seen on AP radiography of spine and pelvis following ossification of supraspinous and interspinous ligaments[23]
- Tram- track sign: Ossification of the apophyseal joint capsules forming two vertical radiodense lines lateral to this central line on frontal view
- Trolley-track sign: combining a central “dagger” sign and a peripheral tram-like track[26]
- Hatchet deformity[23]
- Subchondral erosions, sclerosis and proliferation on iliac side of SI joints[23]
- Bridging or fusion of the pubic symphysis[23]
The modified New York Classification Criteria (mNYCC) was previously used to diagnose axial spondyloarthritis.[1] The mNYCC combines clinical findings with radiograph studies. Radiographic findings are graded on a scale of 0 to 4 where 0 represents normal findings and 4 represents complete ankylosis.[6] A definitive diagnosis is considered with the following radiographic combinations:[27]
- Grade 3 or 4 at bilateral SI joints on radiograph with at least one clinical finding
- Grade 3 or 4 unilaterally (or Grade 2 bilaterally) with two clinical findings
The patient must also fulfil at least one of the following clinical criteria:[27]
- Low back pain and stiffness for at least 3 months, which improves with exercise, but is not relieved by rest
- Limited lumbar spinal motion in sagittal (sideways) and frontal (forward and backward) plane
- Chest expansion decreased relative to normal values corrected for age and sex
Grading
- A patient can be classified as having definite AS if at least 1 clinical criterion plus the radiologic criterion are fulfilled
- A probable diagnosis of AS is made if three clinical criteria are present or the radiologic criterion is present without any signs or symptoms satisfying the clinical criteria
Ankylosing Spondylitis and Axial Spondyloarthritis[edit | edit source]
The modified New York criteria (1984) are somewhat specific, they were found to be insensitive for the determination of early disease. Furthermore, large intraobserver and interobserver disparity in diagnosis further drives the dependency on plain radiographs of the sacroiliac joints. Inflammation of the sacroiliac joints can be identified on MRI in patients with symptoms of AS, even when these joints do not seem to be abnormal on traditional radiography. The same MRI techniques also show spinal inflammation in many patients. The detection of these conditions on MRI resulted in the creation of "axial spondyloarthritis" (see definition / description section above). This diagnosis encompassed patients with definite AS and patients with symptoms alike to those of AS and findings of sacroiliitis on MRI, but without advanced sacroiliitis on traditional radiography.[17]
In 2009, the Assessment of SpondyloArthritis International Society (ASAS) developed classification criteria for axial spondyloarthritis that are supported on these imaging, clinical, and laboratory criteria. Implementing these criteria, the diagnosis is established in persons who have had back pain for 3 or more sequential months prior reaching 45 years of age, with the presence of sacroiliitis confirmed on MRI or plain radiography, and have a minimum of one clinical or laboratory finding that is characteristic of spondyloarthritis. Alternatively, individuals with this history who have a positive test result for HLA-B27 and two symptoms of spondyloarthritis, as identified on clinical examination or laboratory analysis will also meet the criteria for a diagnosis of axial spondyloarthritis.[17]
In summary, as stated by the ASAS criteria, the diagnosis of axial spondyloarthritis comprise two subsets — nonradiographic axial spondyloarthritis and classic ankylosing spondylitis (that is radiographic axial spondyloarthritis).[17]
Outcome Measures[edit | edit source]
- Schober Test
- Occiput to Wall Distance (Flesche test)
- Oswestry Disability Index (ODI)
- Neck Disability Index (NDI)
- Visual Analogue Scale
- Patient Specific Functional Scale
Evaluation Scales[edit | edit source]
- Bath Ankylosing Spondylitis Metrology Index (BASMI)[28][10]
- Revised Leeds Disability Questionnaire (RLDQ)[10]
- European Quality of Life (EuroQoL)[10]
- Bath AS Disease Activity Index (BASDAI; 0-100)[28][10]
- AMOR criteria for Spondyloarthritis[28]
- BASFI index ( Bath Ankylosing Spondylitis Functional Index)[28]
- BAS-G index ( Bath Ankylosing Spondylitis Global Index)[28]
Laboratory values, such as the C-Reactive Protein(CRP), are used to monitor the effectiveness of medication treatments.
Examination[edit | edit source]
A thorough physical examination, particularly of the musculoskeletal system, is needed. Clinical signs are sometimes minimal in the early stages of the disease. Examination of the sacroiliac joints and the spine (including the neck), measurement of chest expansion and range of motion of the hip and shoulder joints, and a search for signs of enthesitis are critical in making an early diagnosis of AS. [9][29][6]
Video 1: The aim of the Schober Test is to assess the mobility of the lumbar spine, which can be abnormal even when it is not obvious to the individual.
Video 2: The lumbar spine side flexion test is another test to measure the lumbar spine mobility.
Video 3: When ankylosing spondylitis affects the mid-back region, normal chest expansion may be compromised. The aim of the chest expansion test is to assess the thoracic mobility.
Video 4: The tragus to wall test is a test to measure the cervical mobility.
There are certain special tests for detecting the involvement of sacro-iliac joint includes-
-Sacro-iliac compression: Direct side to side compression of the pelvis in supine lying may cause pain at the sacro-iliac joints or promoting compression of the symptomatic pelvis in side lying may cause pain.
[33] -Gaenslen's test: The hip and the knee joints of the opposite side are flexed to fix the pelvis, and the hip joint of the side under test is hyperextended over the edge of the table. This will exert a rotational strain over the sacro-iliac joint and give rise to pain.
[34] --Straight leg raising test: The patient is asked to lift the leg up with the knee extended. This will cause pain at the affected sacro- iliac joint.
Complications[edit | edit source]
- Fractures following minor trauma due to osteoporosis, usually compression fractures
- Uveitis
- Reduced flexibility
- Pulmonary function restrictions
- Increased risk of heart diseases (aortic insufficiency, aortitis, angina, pericarditis, and cardiac conduction abnormalities)
- Fatigue
- Gastrointestinal disorders
Medical Management[edit | edit source]
First-Line Drug Treatment : NSAIDs[edit | edit source]
Non-steroidal anti-inflammatory drugs are primarily used for ankylosing spondylitis (AS) patients to reduce the inflammatory symptoms such as pain and stiffness of the spine and other joints. It is important to remember that NSAIDs do not alter the disease's cause and only affect the symptoms.[7] Commonly used NSAIDs for AS are tolmetin, sulindac, naproxen, diclofenac and indomethacin, [8] which is the most effective.[9]
Second-Line Treatments: Corticosteroids and DMARDs[edit | edit source]
When patients are refractory to NSAIDs, corticosteroid injections may be prescribed or disease modifying anti-rheumatic drugs (DMARDs)[7], including methotrexate and sulfasalazine. However, corticosteroids do not have evidence-based outcomes and DMARDs are only proven to be effective for the treatment of peripheral joint diseases.[9]
Biological Medications[edit | edit source]
Tumor Necrosis Factor Inhibitors(anti-TNF- alpha therapy)[edit | edit source]
Research has shown that patients with ankylosing spondylitis have an abundance of pro-inflammatory cytokine tumor necrosis factor (TNF) messenger RNA and proteins in the sacroiliac joints. The use of anti-tumor necrosis factor therapies has therefore proven to be positive.[15] [22] Etanercept [29]and Infliximab[22] have both been used to treat AS patients with successful results.
Biphosphonates[edit | edit source]
Biphosphonates have good outcomes on bone turnover, which is positive as ankylosing spondylitis is characterised by bone resorption and formation. Neridronate and pamidronate are amino-biphosphonates with similar effects as the TNF inhibitor Infliximab. [23] All drugs have side effects, so patients with other health issues need to verify if they are able to take the recommended medicines.
Physiotherapy Management[edit | edit source]
Physiotherapy is an essential part of the treatment of AS.[7] It aims to alleviate pain, increase spinal mobility and functional capacity, reduce morning stiffness, correct postural deformities, increase mobility and improve the psychosocial status of the patients. According to a Cochrane review completed by Dagfinrud and colleagues, a supervised or individual home-based exercise program is better than no intervention,[10] The main aspects of rehabilitation include education, a program of personalised exercises and outline of physical activities to be completed at home or in a group based environment.[10]
Education[edit | edit source]
According to a study conducted by Sweeney and colleagues, education into long term home self-care has proven to be effective.[10] Studies have highlighted how limited education and information can result in poor adherence to rehabilitation.[10] Self care and educational packages including education booklets and videos, reminder stickers and progression charts.[10] The failure or success of exercise programs is determined by compliance with the prescribed program, which requires motivation, participation and time. This can be monitored using patient diaries or physiotherapist records.[10]
Treatment Phase[edit | edit source]
Initial/Acute Phase[edit | edit source]
The initial phase of AS is characterised by morning stiffness and pain in the spine.[10]
Primary Objective[edit | edit source]
- Control of the diffuse and intense pain secondary to joint stiffness,[10]
- Recovery of proprioception, joint stability, restoring normal postural patterns and reduction of pain[10]
- Interventions for pain management along with pharmacological treatment prevents compensatory postures[10]
Secondary Objective[edit | edit source]
- Maintain the elasticity of the pelvis and spine to enable good respiratory function[10]
Remission Phase[edit | edit source]
The remission phase of AS is characterised by pain, restricted mobility of the spine +/- peripheral joints[10]
Primary Objective[edit | edit source]
- Divided into short and long term goals.[10]
Chronic Phase[edit | edit source]
The Chronic phase of AS is characterised by formation of diffused ankyloses, resulting in total rigidity of the spine, and assuming a curved orthostatic posture.[10]
Primary Objective[edit | edit source]
- To enable the patient to maintain their residual function to guarantee the most autonomy possible.
- Education on the importance of physiotherapy and body awareness is key in this phase of AS.
- In-clinic sessions with manual therapy are essential to enable the patient to continue their home exercise program.[10]
Considerations for Physiotherapy Management [edit | edit source]
- Fatigue is a common complain in rheumatological conditions. It can be managed by taking regular microbreaks, avoiding sitting in the same position for long periods, maintaining physical activity and having good sleep hygiene.
- AS patients can suffer from flare-ups of increased disease activity, which can last from days to weeks. During the flare-up the patient may benefit from gentle stretching exercise, taking breaks and medications.
- Joint protection management applies the ergonomic principles to ADL activities to preserve the functional ability.
- Patient compliance can be achieved by determining the barriers facing the individual, including the patient’s exercise preference in the program, using different exercise varieties to avoid boredom and group therapy.
- Educating the patient about his condition and how to manage it, besides having a patient-provider relationship are important for patients’ self managing.
- ADL activities can be made easier using assistive devices and alternative techniques. For example, managing shoes; slip-on shoes can be used or the patient can raise their leg on a stool or place it on the opposite knee. Driving can be difficult due to neck pain and stiffness, advice for driving can include taking breaks on long journeys and using a small pillow behind their back or under their buttock to promote better posture.[36]
Clinical Bottom Line[edit | edit source]
Axial spondyloarthritis is a chronic inflammatory rheumatic disease with unknown etiology. Affected joints progressively become stiff and sensitive due to a bone formation at the level of the joint capsule and cartilage. This can lead to structural and functional impairments and a decrease in quality of life. Regions most affected by the disease are the axial skeleton and sacroiliac joints. A combination of medicines (such as non-steroidal anti-inflammatory drugs and biological medications) and physical therapy is recommended. Physiotherapy primarily consists of range of motion and respiratory exercises as well as working on postural corrections.
Resources[edit | edit source]
To download the PDF click here Living with a Chronic Disease – The Story of Ankylosing Spondylitis
 |
Ankylosing Spondylitis
This presentation, created by Kyle Martin, Robby Martin, Haley Metzner, and Stacey Potter; Texas State DPT Class. |
References[edit | edit source]
- ↑ 1.0 1.1 Dubreuil M, Deodhar A. Axial Spondyloarthritis Classification Criteria–The debate continues. Current opinion in rheumatology. 2017 Jul;29(4):317.
- ↑ Martey C. Overview of Spondyloarthropathies Course. Plus2020.
- ↑ 3.0 3.1 Sieper J, Poddubnyy D. Axial spondyloarthritis. The Lancet. 2017 Jul 1;390(10089):73-84.
- ↑ Martey C. Overview of Spondyloarthropathies Course. Plus2020.
- ↑ Wenker KJ, Quint JM. Ankylosing Spondylitis. [Updated 2020 Jul 13]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470173/
- ↑ 6.0 6.1 6.2 6.3 6.4 6.5 Laura A, Haftel H. Shoulder, Knee, and Hip Pain as Initial Symptoms of Juvenile Ankylosing Spondylitis: A Case Report, Journal of Orthopaedic & Sports Physical Therapy [Internet], 1998Feb [cited 2020 Oct 4];27(2):167–172. Available from https://www.jospt.org/doi/10.2519/jospt.1998.27.2.167
- ↑ 7.0 7.1 7.2 7.3 7.4 7.5 Giles L, Singer K. The clinical anatomy and management of back pain series, Volume 2 Clincal Anatomy and Management of Thoracic Spine Pain, Butterworth Heinemann, 2000: 61-66.
- ↑ 8.0 8.1 8.2 8.3 8.4 Mills K, Page G, Siwek R. A color atlas of low back pain. London:Wolfe Medical Publications,1990.
- ↑ 9.0 9.1 9.2 9.3 9.4 9.5 9.6 9.7 Andersson GB, McNeill TW. Lumbar spine syndromes: Evaluation and treatment. Springer Science & Business Media; 2012 Dec 6.
- ↑ 10.00 10.01 10.02 10.03 10.04 10.05 10.06 10.07 10.08 10.09 10.10 10.11 10.12 10.13 10.14 10.15 10.16 10.17 10.18 10.19 10.20 10.21 Nava T. Physiotherapy rehabilitation in patients with ankylosing spondylitis. Beyond Rheumatol [Internet]. 2019 Dec 20 [cited 2020 Sep 26];1(2):37-6. Available from: http://beyond-rheumatology.org/index.php/br/article/view/6
- ↑ Tan S, Wang R, Ward MM. Syndesmophyte growth in ankylosing spondylitis. Current opinion in rheumatology. 2015 Jul;27(4):326.
- ↑ Syndesmophytes. National Library of Medicine
- ↑ 13.0 13.1 13.2 13.3 Dean L, Jones G, MacDonald A, Downham C, Sturrock R, Macfarlane G. Global prevalence of ankylosing spondylitis. Rheumatology [Internet]. 2014 Apr [cited 2020 Sep 26]; 53(4), 650–657. Available from https://academic.oup.com/rheumatology/doi.org/10.1093/rheumatology/ket387
- ↑ 14.0 14.1 14.2 Watad A, Bridgewood C, Russell T, Marzo-Ortega H, Cuthbert R, McGonagle D. The early phases of ankylosing spondylitis: emerging insights from clinical and basic science. Frontiers in immunology. 2018:2668.
- ↑ 15.0 15.1 Alvarez I, López de Castro JA. HLA-B27 and immunogenetics of spondyloarthropathies. Curr Opin Rheumatol. 2000;12(4):248-253 Alvarez I, de Castro JA. HLA-B27 and immunogenetics of spondyloarthropathies. Current opinion in rheumatology. 2000 Jul 1;12(4):248-53.
- ↑ Braggins S. Back care: a clinical approach. Churchill Livingstone; 2000.
- ↑ 17.0 17.1 17.2 17.3 17.4 Taurog JD, Chhabra A, Colbert RA. Ankylosing spondylitis and axial spondyloarthritis. New England Journal of Medicine. 2016 Jun 30;374(26):2563-74.
- ↑ 18.0 18.1 Baaj A, Praveen V, Mummaneni S, Uribe R, Vaccaro S, Mark S. Handbook of spine surgery. New York:Thieme, 2010:180-182.
- ↑ 19.0 19.1 19.2 Andersson GB, McNeill TW. Lumbar spine syndromes: Evaluation and treatment. Springer Science & Business Media; 2012 Dec 6.
- ↑ Kataria RK, Brent LH. Spondyloarthropathies. American family physician. 2004 Jun 15;69(12):2853-60.
- ↑ Goodman Catherine C, Snyder TE. Differential diagnosis for physical therapists: screening for referral. St. Louis: Saunders Elsevier. 2007.
- ↑ 22.0 22.1 22.2 22.3 22.4 Baaj A, Praveen V, Mummaneni S, Uribe R, Vaccaro S, Mark S. Handbook of spine surgery. New York:Thieme, 2010:180-182.
- ↑ 23.00 23.01 23.02 23.03 23.04 23.05 23.06 23.07 23.08 23.09 23.10 23.11 23.12 Mandl P, Navarro-Compán V, Terslev L, Aegerter P, Van Der Heijde D, D'Agostino MA, Baraliakos X, Pedersen SJ, Jurik AG, Naredo E, Schueller-Weidekamm C. EULAR recommendations for the use of imaging in the diagnosis and management of spondyloarthritis in clinical practice. Annals of the rheumatic diseases. 2015 Jul 1;74(7):1327-39.
- ↑ Shiny corner sign (ankylosing spondylitis).Available from: https://radiopaedia.org/articles/shiny-corner-sign-ankylosing-spondylitis#:~:text=The%20shiny%20corner%20sign%20is,are%20known%20as%20Romanus%20lesions.
- ↑ Slobodin G, Eshed I. Non-radiographic axial spondyloarthritis. Isr Med Assoc J. 2015 Dec 1;17(12):770-6.
- ↑ Lambrecht V, Vanhoenacker FM, Van Dyck P, Gielen J, Parizel PM. Ankylosing spondylitis: what remains of the standard radiography anno 2004. JBR-BTR. 2005;88(1):25-30.
- ↑ 27.0 27.1 Linden SV, Valkenburg HA, Cats A. Evaluation of diagnostic criteria for ankylosing spondylitis. Arthritis & Rheumatism. 1984 Apr;27(4):361-8.
- ↑ 28.0 28.1 28.2 28.3 28.4 Jordan CL, Rhon DI. Differential diagnosis and management of ankylosing spondylitis masked as adhesive capsulitis: a resident's case problem. journal of orthopaedic & sports physical therapy. 2012 Oct;42(10):842-52.
- ↑ 29.0 29.1 Bullough G, Boachie-Adjei O. Atlas of spinal diseases. Hampshire:Gower Medical Publishing, 1987.
- ↑ bjchealthAU. Modified Schober's Test. Available from: http://www.youtube.com/watch?v=B9RaFB5BwrQ [last accessed 01/12/12]
- ↑ bjchealthAU. Lumbar Side Flexion Test. Available from: http://www.youtube.com/watch?v=c-IeFZkPEoE [last accessed 01/12/12]
- ↑ bjchealthAU. Chest Expansion Test. Available from: http://www.youtube.com/watch?v=SumtVr5c1Qg [last accessed 01/12/12]
- ↑ Physiotutors. Compression Test / Side-lying Compression | Sacroiliac Joint Provocation. Available from youtube.com/watch?v=pWjvrhWMR4w (last accessed on 20/7/2023
- ↑ Physiotutors. Gaenslen's Test | Sacroiliac Joint Provocation. Available from https://www.youtube.com/watch?v=ED_bYoQk9d4 (last accessed on 20/7/2023
- ↑ Physiotutors. Straight Leg Raise or Lasègue's Test for Lumbar Radiculopathy. Available from https://www.youtube.com/watch?v=LdAD9GNv8FI (last accessed on 20/7/2023)
- ↑ Living with a Chronic Disease – The Story of Ankylosing Spondylitis