Achilles Tendon: Difference between revisions
No edit summary |
Kim Jackson (talk | contribs) No edit summary |
||
| (21 intermediate revisions by 5 users not shown) | |||
| Line 8: | Line 8: | ||
[[Image:Achilles tendon.jpg|right]] | [[Image:Achilles tendon.jpg|right]] | ||
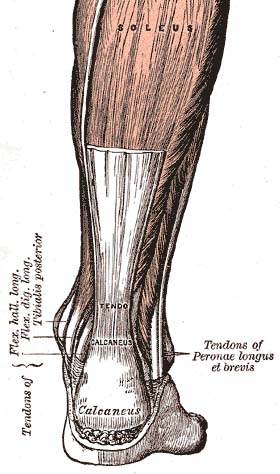
The Achilles ( | The Achilles (calcaneal) [[Tendon Anatomy|tendon]] is a common tendon shared between the [[Gastrocnemius|gastrocnemius]] and [[Soleus|soleus]] muscles of the posterior leg. It connects the two muscle groups (collectively, triceps surae) to the [[calcaneus]]. Generally, the tendon winds 90 degrees on its path towards the heel, such that the gastrocnemius attaches laterally and the soleus attaches medially.<ref name="Moore">Moore KL, Agur AMR, Dalley AF. Essential clinical anatomy. 4th ed. Baltimore: Lippincott Williams & Wilkins, 2011.</ref> It is the thickest tendon in the human body and has the capacity to withstand large tensile forces.<ref name=":0">Wong M, Kiel J. Anatomy, bony pelvis and lower limb, Achilles tendon. StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK499917/ 2018. [Accessed 30th September, 2020].</ref> <br> | ||
A subcutaneous calcaneal bursa permits movement of the skin over the flexed tendon. A deep bursa of the Achilles tendon reduces friction to allow free movement of the tendon over the bone.<ref name="Moore" /> | A subcutaneous calcaneal bursa permits movement of the skin over the flexed tendon. A deep bursa of the Achilles tendon reduces friction to allow free movement of the tendon over the bone.<ref name="Moore" /> | ||
== Attachments == | |||
The tendon provides a distal attachment site for the gastrocnemius (lateral and medial heads) as well as the soleus muscles. It inserts onto the posterior surface of the calcaneus (heel bone). The plantaris tendon also fuses with the medial side of the Achilles tendon proximal to its attachment site.<ref name="Drake">Drake RL, Vogl AW, Mitchell AWM. Gray's anatomy for students. 2nd ed. Philadelphia: Churchill Livingstone Elsevier, 2010.</ref> | The tendon provides a distal attachment site for the gastrocnemius (lateral and medial heads) as well as the soleus muscles. It inserts onto the posterior surface of the calcaneus (heel bone). The [[plantaris]] tendon also fuses with the medial side of the Achilles tendon proximal to its attachment site.<ref name="Drake">Drake RL, Vogl AW, Mitchell AWM. Gray's anatomy for students. 2nd ed. Philadelphia: Churchill Livingstone Elsevier, 2010.</ref> | ||
== Function == | == Function == | ||
Through the action of the triceps surae, which raises the heel and lowers the forefoot, the Achilles tendon is involved in | Through the action of the triceps surae, which raises the heel and lowers the forefoot, the Achilles tendon is involved in plantar flexion of the foot (approximately 93% of the plantar flexion force).<ref name="Moore" /> The contraction of the gastrocnemius and soleus muscles result in a translational force through the Achilles tendon that results in plantar flexion of the foot. This action is very significant in human locomotion and propulsion responsible for actions such as walking, running and even jumping.<ref name=":0" /><ref>Williams SK, Brage M. Heel pain-plantar fasciitis and Achilles enthesopathy. Clinics in sports medicine. 2004 Jan;23(1):123.</ref> Also, these motions exert the greatest load on the Achilles tendon, with tensile loads up to about ten times the body's weight. The anatomy of the tendon provides for both elasticity (recoil) and shock-absorbance in the foot.<ref name="Moore" /> It is the largest and strongest tendon in the human body and is capable of supporting tensional forces produced by movement of the lower limb.<ref name="Järvinen">Järvinen TA, Kannus P, Paavola M, Järvinen TL, Józsa L, Järvinen M. Achilles tendon injuries. Current opinion in rheumatology. 2001 Mar 1;13(2):150-5.</ref><br> | ||
== Blood Supply == | |||
The Achilles tendon has its blood supply from longitudinal arteries which course the length of the tendon from two main blood vessels<ref>Abate M, Salini V. Mid-portion Achilles tendinopathy in runners with metabolic disorders. European Journal of Orthopaedic Surgery & Traumatology. 2019 Apr 9;29(3):697-703.</ref>: | |||
# Posterior tibial artery: Which supplies the proximal and distal sections. | |||
# Peroneal artery: Which supply the middle section. | |||
The tendon has a generally poor blood supply throughout its length, as measured by the number of vessels per cross-sectional area.<ref name=":0" /> In addition, a relative region of hypovascularity exists in its midsection which usually happens to be the site around which most injuries occur. This has been attributed as a contributing factor to diminished healing after trauma.<ref name=":0" /> | |||
Overall, the tendon has a relatively poor blood supply throughout its length, as measured by vessels per cross-sectional area. Also, there is a relatively hypovascular area in the midsection, which correlates to the location of many injuries: the area approximately 2 to 6 cm from the tendon's insertion point. Some have also suggested that poor vascularity contributes to diminished healing after trauma. Blood supply to the tendon also diminishes with age. | |||
== Innervation == | |||
The Achilles tendon is innervated by nerves of the muscles from which it is formed and cutaneous nerves. the sural nerve particularly plays a major role in its innervation with a smaller supply from the tibial nerve.<ref name=":1">O'Brien M. The anatomy of the Achilles tendon. Foot and ankle clinics. 2005 Jun 1;10(2):225-38.</ref> The nerve endings form a longitudinal plexus which supplies afferent fibres in the great majority of the tendon. <ref>Doral MN, Alam M, Bozkurt M, Turhan E, Atay OA, Dönmez G, Maffulli N. Functional anatomy of the Achilles tendon. Knee Surgery, Sports Traumatology, Arthroscopy. 2010 May 1;18(5):638-43.</ref> The afferent receptors are largely located close to the osteotendinous junction and have all four types of receptors which are the type I, II, III, IV receptors (Ruffini corpuscle pressure receptors, Vater-Paccinian corpuscle sensitive to movement, Golgi tendons mechanoreceptors and free nerve endings that serve as pain receptors). <ref name=":1" /> | |||
== Pathology/Injury == | == Pathology/Injury == | ||
| Line 30: | Line 41: | ||
== Clinical Examination == | == Clinical Examination == | ||
=== Palpation === | ==== Palpation ==== | ||
The foot is | The foot is plantar flexed against resistance or gravity (body weight) while observing the posterior leg. | ||
=== Examination | ==== Examination ==== | ||
==== Achilles Tendinopathy ==== | |||
*Palpation and physical examination | *Palpation and physical examination | ||
| Line 46: | Line 56: | ||
*The [[VISA-A scale|VISA-A]] is a self-administered questionnaire that evaluates symptoms and their effect on physical activity for patients with chronic Achilles tendinopathy.<br> | *The [[VISA-A scale|VISA-A]] is a self-administered questionnaire that evaluates symptoms and their effect on physical activity for patients with chronic Achilles tendinopathy.<br> | ||
==== Achilles Rupture ==== | |||
*The [[Matles Test|Matles Test]] is a visual diagnostic test for suspected Achilles Tendon Rupture.<br> | *The [[Matles Test|Matles Test]] is a visual diagnostic test for suspected Achilles Tendon Rupture.<br> | ||
| Line 61: | Line 70: | ||
== Physiotherapeutic Techniques == | == Physiotherapeutic Techniques == | ||
{| width="100%" cellspacing="1" cellpadding="1" | |||
|- | |||
| {{#ev:youtube|yiHRNfFXtfs|412}} | |||
| {{#ev:youtube|MsViGvhflVE|412}} | |||
|} | |||
== Achilles Tendinopathy == | |||
A summary of treatment interventions for Achilles Tendinopathy can be found in the [[Achilles Tendinopathy Toolkit: Section C - Summary of Evidence and Recommendations for Interventions|Achilles Tendinopathy Toolkit]].<br> | |||
== Achilles Rupture == | |||
Optimal treatment of acute [[Achilles Rupture]] is a highly contested topic<ref name="Pedowitz">Pedowitz D, Kirwan G. Achilles tendon ruptures. Current reviews in musculoskeletal medicine. 2013 Dec 1;6(4):285-93.</ref>, but can be broken down into: | |||
Optimal treatment of acute Achilles Rupture is a highly contested topic<ref name="Pedowitz">Pedowitz D, Kirwan G. Achilles tendon ruptures. Current | |||
*Open Operative | *Open Operative | ||
| Line 76: | Line 86: | ||
*Nonoperative Types.<ref name="Järvinen" /><br> | *Nonoperative Types.<ref name="Järvinen" /><br> | ||
If a physician advocates for a non-surgical approach, the foot is typically placed in a cast or splint, such that it is held in plantar flexion. This treatment can be combined with early physiotherapy.<ref name="Soroceanu">Soroceanu A, Sidhwa F, Aarabi S, Kaufman A, Glazebrook M. Surgical versus nonsurgical treatment of acute achilles tendon rupture. J Bone Joint Surg Am 2012;94(23):2136-2143 | If a physician advocates for a non-surgical approach, the foot is typically placed in a cast or splint, such that it is held in plantar flexion. This treatment can be combined with early physiotherapy.<ref name="Soroceanu">Soroceanu A, Sidhwa F, Aarabi S, Kaufman A, Glazebrook M. [https://pubmed.ncbi.nlm.nih.gov/23224384/ Surgical versus nonsurgical treatment of acute achilles tendon rupture]. J Bone Joint Surg Am 2012;94(23):2136-2143. </ref> | ||
More recently, evidence-based guidelines for managing Achilles Tendon Rupture have been released by the American Academy of Orthopaedic Surgeons (AAOS). None of the recommendations have a grading of "strong", but consensus recommendations based on expert opinion advocate the need for a detailed patient history and physical examination in diagnosis.<ref name="AAOS" /><ref name="Pedowitz" /> The group also recommends a more cautious approach in operative treatment for certain patients, including those with diabetes and/or neuropathy, aged 65 or older, who are obese or who have sedentary lifestyles, who are | More recently, evidence-based guidelines for managing Achilles Tendon Rupture have been released by the American Academy of Orthopaedic Surgeons (AAOS). None of the recommendations have a grading of "strong", but consensus recommendations based on expert opinion advocate the need for a detailed patient history and physical examination in diagnosis.<ref name="AAOS" /><ref name="Pedowitz" /> The group also recommends a more cautious approach in operative treatment for certain patients, including those with diabetes and/or neuropathy, aged 65 or older, who are obese or who have sedentary lifestyles, who are immuno-compromized, and who use tobacco.<ref name="AAOS" /> The only recommendations rated as "moderate" in strength (fair quality evidence) were specifically for '''<u>post-operative interventions</u>'''. These were the suggestions for: | ||
#Protective weight bearing and | #Protective weight bearing and | ||
| Line 89: | Line 99: | ||
A meta-analysis of randomized trials of Achilles tendon rupture repair has suggested that a nonoperative approach, in which plantar flexion is used to produce tendon apposition, can allow adequate healing. Functional bracing and modified postoperative mobilization, including daily active plantar flexion exercises, may stimulate tendon healing and reduce the potential rate of re-rupture.<ref name="Soroceanu" /> | A meta-analysis of randomized trials of Achilles tendon rupture repair has suggested that a nonoperative approach, in which plantar flexion is used to produce tendon apposition, can allow adequate healing. Functional bracing and modified postoperative mobilization, including daily active plantar flexion exercises, may stimulate tendon healing and reduce the potential rate of re-rupture.<ref name="Soroceanu" /> | ||
== Resources == | == Resources == | ||
| Line 101: | Line 109: | ||
<references /><br> | <references /><br> | ||
[[Category:Ankle]] | |||
[[Category:Foot]] | |||
[[Category:Musculoskeletal/Orthopaedics|Orthopaedics]][[Category:Ankle]][[Category:Tendons]][[Category: | [[Category:Musculoskeletal/Orthopaedics|Orthopaedics]] | ||
[[Category:Ankle]] | |||
[[Category:Tendons]] | |||
[[Category:Muscles]] | |||
[[Category:Anatomy]] | |||
[[Category:Ankle - Anatomy]] | |||
[[Category:Foot - Anatomy]] | |||
[[Category:Ankle - Muscles]] | |||
[[Category:Foot - Muscles]] | |||
Latest revision as of 14:43, 19 April 2022
Original Editor - Richard Benes
Top Contributors - Richard Benes, Kim Jackson, Joseph Ayotunde Aderonmu, Naomi O'Reilly, George Prudden, WikiSysop, 127.0.0.1, Admin, Laura Ritchie, Evan Thomas, Uchechukwu Chukwuemeka and Shrutika Das
Anatomy[edit | edit source]
The Achilles (calcaneal) tendon is a common tendon shared between the gastrocnemius and soleus muscles of the posterior leg. It connects the two muscle groups (collectively, triceps surae) to the calcaneus. Generally, the tendon winds 90 degrees on its path towards the heel, such that the gastrocnemius attaches laterally and the soleus attaches medially.[1] It is the thickest tendon in the human body and has the capacity to withstand large tensile forces.[2]
A subcutaneous calcaneal bursa permits movement of the skin over the flexed tendon. A deep bursa of the Achilles tendon reduces friction to allow free movement of the tendon over the bone.[1]
Attachments[edit | edit source]
The tendon provides a distal attachment site for the gastrocnemius (lateral and medial heads) as well as the soleus muscles. It inserts onto the posterior surface of the calcaneus (heel bone). The plantaris tendon also fuses with the medial side of the Achilles tendon proximal to its attachment site.[3]
Function[edit | edit source]
Through the action of the triceps surae, which raises the heel and lowers the forefoot, the Achilles tendon is involved in plantar flexion of the foot (approximately 93% of the plantar flexion force).[1] The contraction of the gastrocnemius and soleus muscles result in a translational force through the Achilles tendon that results in plantar flexion of the foot. This action is very significant in human locomotion and propulsion responsible for actions such as walking, running and even jumping.[2][4] Also, these motions exert the greatest load on the Achilles tendon, with tensile loads up to about ten times the body's weight. The anatomy of the tendon provides for both elasticity (recoil) and shock-absorbance in the foot.[1] It is the largest and strongest tendon in the human body and is capable of supporting tensional forces produced by movement of the lower limb.[5]
Blood Supply[edit | edit source]
The Achilles tendon has its blood supply from longitudinal arteries which course the length of the tendon from two main blood vessels[6]:
- Posterior tibial artery: Which supplies the proximal and distal sections.
- Peroneal artery: Which supply the middle section.
The tendon has a generally poor blood supply throughout its length, as measured by the number of vessels per cross-sectional area.[2] In addition, a relative region of hypovascularity exists in its midsection which usually happens to be the site around which most injuries occur. This has been attributed as a contributing factor to diminished healing after trauma.[2]
Overall, the tendon has a relatively poor blood supply throughout its length, as measured by vessels per cross-sectional area. Also, there is a relatively hypovascular area in the midsection, which correlates to the location of many injuries: the area approximately 2 to 6 cm from the tendon's insertion point. Some have also suggested that poor vascularity contributes to diminished healing after trauma. Blood supply to the tendon also diminishes with age.
Innervation[edit | edit source]
The Achilles tendon is innervated by nerves of the muscles from which it is formed and cutaneous nerves. the sural nerve particularly plays a major role in its innervation with a smaller supply from the tibial nerve.[7] The nerve endings form a longitudinal plexus which supplies afferent fibres in the great majority of the tendon. [8] The afferent receptors are largely located close to the osteotendinous junction and have all four types of receptors which are the type I, II, III, IV receptors (Ruffini corpuscle pressure receptors, Vater-Paccinian corpuscle sensitive to movement, Golgi tendons mechanoreceptors and free nerve endings that serve as pain receptors). [7]
Pathology/Injury[edit | edit source]
The Achilles tendon is susceptible to damage with repetitive use or overload. These types of injuries typically occur in athletes and are usually sports or exercise-related.[5]
The most common types of injuries are due to overuse and Achilles Tendon disorders, of which 55%-65% are diagnosed as Achilles Tendinopathy. Insertional issues (Retrocalcaneal Bursitis and Insertional Tendinopathy) account for 25%-35% of cases, with the remaining diagnosed as partial tears or undiagnosed complete ruptures.[5]
Complete Rupture of the Achilles Tendon has been estimated to occur at a rate of 5.5 to 9.9 per 100,000 in North America and between 6 to 18 per 100,000 in Europe.[9] Roughly 60-75% of ruptures take place in sporting activities, including basketball and soccer.[5]
Clinical Examination[edit | edit source]
Palpation[edit | edit source]
The foot is plantar flexed against resistance or gravity (body weight) while observing the posterior leg.
Examination[edit | edit source]
Achilles Tendinopathy[edit | edit source]
- Palpation and physical examination
- The VISA-A is a self-administered questionnaire that evaluates symptoms and their effect on physical activity for patients with chronic Achilles tendinopathy.
Achilles Rupture[edit | edit source]
- The Matles Test is a visual diagnostic test for suspected Achilles Tendon Rupture.
- The Thompson Test is used to identify the presence of a complete Achilles Tendon Rupture and is performed by squeezing the calf.
Physiotherapeutic Techniques[edit | edit source]
Achilles Tendinopathy[edit | edit source]
A summary of treatment interventions for Achilles Tendinopathy can be found in the Achilles Tendinopathy Toolkit.
Achilles Rupture[edit | edit source]
Optimal treatment of acute Achilles Rupture is a highly contested topic[13], but can be broken down into:
- Open Operative
- Percutaneous Operative
- Nonoperative Types.[5]
If a physician advocates for a non-surgical approach, the foot is typically placed in a cast or splint, such that it is held in plantar flexion. This treatment can be combined with early physiotherapy.[14]
More recently, evidence-based guidelines for managing Achilles Tendon Rupture have been released by the American Academy of Orthopaedic Surgeons (AAOS). None of the recommendations have a grading of "strong", but consensus recommendations based on expert opinion advocate the need for a detailed patient history and physical examination in diagnosis.[9][13] The group also recommends a more cautious approach in operative treatment for certain patients, including those with diabetes and/or neuropathy, aged 65 or older, who are obese or who have sedentary lifestyles, who are immuno-compromized, and who use tobacco.[9] The only recommendations rated as "moderate" in strength (fair quality evidence) were specifically for post-operative interventions. These were the suggestions for:
- Protective weight bearing and
- Use of a protective device that allows mobilization 2-4 weeks post-operatively.[13][9]
A review on the topic advocates for educating patients on the potential risks and benefits of each type of treatment, including operative and nonoperative types.[13]
Healing[edit | edit source]
A meta-analysis of randomized trials of Achilles tendon rupture repair has suggested that a nonoperative approach, in which plantar flexion is used to produce tendon apposition, can allow adequate healing. Functional bracing and modified postoperative mobilization, including daily active plantar flexion exercises, may stimulate tendon healing and reduce the potential rate of re-rupture.[14]
Resources[edit | edit source]
AAOS Guideline and Evidence Report: The Diagnosis and Treatment of Acute Achilles Tendon Rupture (2009)
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 Moore KL, Agur AMR, Dalley AF. Essential clinical anatomy. 4th ed. Baltimore: Lippincott Williams & Wilkins, 2011.
- ↑ 2.0 2.1 2.2 2.3 Wong M, Kiel J. Anatomy, bony pelvis and lower limb, Achilles tendon. StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK499917/+2018. [Accessed 30th September, 2020].
- ↑ Drake RL, Vogl AW, Mitchell AWM. Gray's anatomy for students. 2nd ed. Philadelphia: Churchill Livingstone Elsevier, 2010.
- ↑ Williams SK, Brage M. Heel pain-plantar fasciitis and Achilles enthesopathy. Clinics in sports medicine. 2004 Jan;23(1):123.
- ↑ 5.0 5.1 5.2 5.3 5.4 Järvinen TA, Kannus P, Paavola M, Järvinen TL, Józsa L, Järvinen M. Achilles tendon injuries. Current opinion in rheumatology. 2001 Mar 1;13(2):150-5.
- ↑ Abate M, Salini V. Mid-portion Achilles tendinopathy in runners with metabolic disorders. European Journal of Orthopaedic Surgery & Traumatology. 2019 Apr 9;29(3):697-703.
- ↑ 7.0 7.1 O'Brien M. The anatomy of the Achilles tendon. Foot and ankle clinics. 2005 Jun 1;10(2):225-38.
- ↑ Doral MN, Alam M, Bozkurt M, Turhan E, Atay OA, Dönmez G, Maffulli N. Functional anatomy of the Achilles tendon. Knee Surgery, Sports Traumatology, Arthroscopy. 2010 May 1;18(5):638-43.
- ↑ 9.0 9.1 9.2 9.3 American Academy of Orthopaedic Surgeons. The Diagnosis and Treatment of Acute Achilles Tendon Rupture. Rosemont: American Academy of Orthopaedic Surgeons, 2009. Available at: http://www.aaos.org/Research/guidelines/atrguideline.asp
- ↑ Clinically Relevant Technologi. Achilles Tendon Palpation Test (CR). Available from: https://www.youtube.com/watch?v=a9FI_0HpQ5Y [Accessed 18 Mar 2015]
- ↑ MSK Medicine. Matles Test. Available from: https://www.youtube.com/watch?v=7Vw9g-aI5pQ [Accessed 18 Mar 2015]
- ↑ Clinically Relevant Technologi. Thompson's Test (CR). Available from: https://www.youtube.com/watch?v=GtJF5cUmslI [Accessed 18 Mar 2015]
- ↑ 13.0 13.1 13.2 13.3 Pedowitz D, Kirwan G. Achilles tendon ruptures. Current reviews in musculoskeletal medicine. 2013 Dec 1;6(4):285-93.
- ↑ 14.0 14.1 Soroceanu A, Sidhwa F, Aarabi S, Kaufman A, Glazebrook M. Surgical versus nonsurgical treatment of acute achilles tendon rupture. J Bone Joint Surg Am 2012;94(23):2136-2143.