|
|
| Line 1: |
Line 1: |
| --[[User:Shauni Van Overstraeten|Shauni Van Overstraeten]] 17:17, 26 June 2013 (BST), Anne Ceulemans, Lise Demesmaeker, Ann Verdoodt
| | <div class="editorbox"> |
| | '''Original Editor '''- [[User:Karolyn Conolty|Karolyn Conolty]] |
|
| |
|
| = <br><br>Search Strategy =
| | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} - [[User:Alex Scott|Alex Scott]] |
| | </div> |
| | == Clinically Relevant Anatomy<br> == |
|
| |
|
| Databases Searched: Pubmed, Pedro <br>Keyword Searches: Achilles tendinosis, achilles tendopathy , tendinopathy ankle, tendinopathy lower limb, achilles injury<br>Library: Vrije Universiteit Brussel <br>Search Timeline: October 22, 2012 – November 25,2012
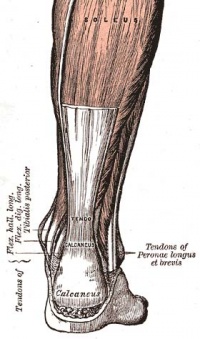
| | [[Image:Achilles tendon.jpg|thumb|right|200px|Achilles Tendon]] |
|
| |
|
| = <br>Definition/ Description = | | The [[Achilles Tendon|Achilles tendon]] is the single tendon of the [[Soleus|soleus]] and [[Gastrocnemius|gastrocnemius]] muscles, inserting into the [[Calcaneus|calcaneus]].<ref name="Cook et al">Cook JL, Khan KM, Purdam C. Achilles tendinopathy. Manual Therapy 2002;7(3):121-130.</ref><br> |
|
| |
|
| <br>Achilles tendinosis, also called as Achillodynia, is a degenerative change of the Achillestendon associated with pain and often with thickening of the tendon. It is common in athletes, but it also occurs in non athletes. Surgical specimens show a range of degenerative changes of the affected tendon, such as changes in tendon fibre structure and arrangement as well as an increase in glycosaminoglycans, which may explain the swelling of the tendon.<ref>T E O Schubert, C. W. (2005). Achilles tendinosis is associated with sprouting of substance P positive nerve fibres. Ann Rheum Dis , 1083-1086.fckLR Level 3B</ref> | | == Mechanism of Injury / Pathological Process<br> == |
|
| |
|
| Tendinosis of the Achilles tendon is therefore a degeneration process in which no temperature rises occur, as apposed to tendonitis.<br>Tendinosis is often confused with tendonitis, but it is important to understand the difference between these two pathologies.<br>Tendonitis is an inflammation of the tendon. This inflammation causes micro-tears in the tendon when the tendon is acutely overloaded. <br>This diagnosis is often mistakenly used when the patiënt actually has tendinosis.<br>It is very important to distinguish between these disorders, to discover which treatment is required, and what the expected duration of the treatment will be.<br>The healing time for tendonitis is generally shorter, and commonly takes several days to 6 weeks. For tendinosis, the expected duration is variable, this can be 6-10 weeks, but it might also take 3-6 months, when the tendinosis has become chronic. <ref>K M Khan, a. p. (2002). Time to abandon the “tendinitis” myth: Painful, overuse tendon conditions have a non-inflammatory pathology . BMJ , 324:626.fckLR Level 2A</ref>, <ref>Evelyn Bass, L. (2012). Tendinopathy: Why the Difference Between Tendinitis and Tendinosis Matters. Int J Ther Massage Bodywork. , 5(1): 14–17.fckLR Level 2C</ref><br> <br>[[Image:Achillestendinosis.png]]
| | '''Achilles tendonitis''' is commonly seen in athletes who sustain an increase in training load, and is most often due to overuse. Tendons respond poorly to overuse, therefore healing is slow. This can leave a tendon pathologically defective, which decreases tendon strength and leaves it less able to tolerate load, thus vulnerable to further injury. <ref name="Cook et al" />Extrinsic factors contributing to this condition include training errors and inappropriate footwear. Intrinsic factors include inflexibility, weakness and malalignment. <ref name="Roos et al">Roos EM, Engstrom M, Lagerquist A, Soderberg B. Clinical improvement after 6 weeks of eccentric exercise in patients with mid-portion Achilles tendinopathy - a randomized trial with 1-year follow-up. Scand J Med Sci Sports. 2004;14:286-295.</ref> |
|
| |
|
| <br>
| | == Clinical Presentation == |
| | |
| <br>
| |
| | |
| <br>Left: The histology of a healthy tendon.<br>Right: The histology of a damaged tendon, in which the disorientation of the collagen fibres and the division of the fibres is clearly visible.<ref>John J. Wilson, T. M. (2005). Common overuse tendon problems: A review and recommendations for treatment. University of Wisconsin Medical School, Madison, Wisconsin , 1-8.fckLR Level 1A</ref>
| |
| | |
| <br>
| |
|
| |
|
| = Clinically Relevant Anatomy = | | Morning pain is a hallmark symptom because the Achilles tendon must tolerate full range of movement including stretch immediately on rising in the morning. Symptoms are typically localized to the tendon and immediate surrounding area. Swelling and pain at the attachment are less common. The tendon can appear to have subtle changes in outline, becoming thicker in the A-P and M-L planes.<ref name="Cook et al" /><br> |
|
| |
|
| = Epidemiology / Etiology = | | == Diagnostic Procedures == |
|
| |
|
| The precise cause of tendinosis remains unclear. Even though tendinosis of the achilles tendon is often connected to sport activities, the ailment is also often found with people who do not practice sports. The biggest cause is the excessive overburdening of the tendon. A light degeneration of the achilles tendon can be latently present, but pain only comes into being when the tendon is overburdened. It is also noted that the ailment is usually not preceded by a trauma.<ref>John J. Wilson, T. M. (2005). Common overuse tendon problems: A review and recommendations for treatment. University of Wisconsin Medical School, Madison, Wisconsin , 1-8.fckLR Level 1A</ref>, <ref>MIKA PAAVOLA, M. P. (2002). Current Concepts Review Achilles Tendinopathy . THE JOURNAL OF BONE AND JOINT SURGERY, INCORPORATED , 2062-2076.</ref>
| | [[Medical Imaging|Imaging studies]] are not necessary to diagnose Achilles tendonitis, but may be useful with differential diagnosis. US is the imaging modality of first choice as it provides a clear indication of tendon width, changes of water content within the tendon and [[Collagen|collagen]] integrity, as well as bursal swelling. MRI may be indicated if diagnosis is unclear or symptoms are atypical. MRI may show increased signal within the Achilles.<ref name="Cook et al" /><br> |
|
| |
|
| An inflammation is necessary to start a restoration process in the damaged tissue, but the use of certain medication, such as corticosteroids and quinolones counter the inflammation, and as a result also the restoration process. Even when the patient does not take this medication, tendinosis is also a consequence of a disrupted restoration process.<ref>MIKA PAAVOLA, M. P. (2002). Current Concepts Review Achilles Tendinopathy . THE JOURNAL OF BONE AND JOINT SURGERY, INCORPORATED , 2062-2076.</ref>
| | == Outcome Measures == |
|
| |
|
| = Characteristics/Clinical presentation <ref>Dijk, M. N. (2011). Mid-portion Achilles tendinopathy: why painful? An evidence-based philosophy. Knee Surg Sports Traumatol Arthrosc , 19(8): 1367–1375.fckLR Level 5</ref>,<ref>John J. Wilson, T. M. (2005). Common overuse tendon problems: A review and recommendations for treatment. University of Wisconsin Medical School, Madison, Wisconsin , 1-8.fckLR Level 1A</ref>,<ref>KL. Luscombe, P. S. (2003). Achilles tendinopathy. Trauma , 215-225.fckLR Level 2C</ref> =
| | Robinson et al recommend the [[VISA-A scale|VISA-A scale]]. This is a subjective rating scale that quantifies the symptoms and dysfunction in the Achilles tendon. It is very useful to rate Achilles tendons and to assess progress of recovery during rehabilitation. <ref name="Cook et al" /><ref name="Robinson et al">Robinson JM, Cook JL, Purdam C et al. The VISA-A questionnaire: a valid and reliable index of the clinical severity of Achilles tendinopathy. British J of Sports Med. 2001;35:335-341.</ref> |
|
| |
|
| <br>Common symptoms are swelling and pain. This pain usually occurs after exercises.<br>With people who have a tendinopathy of the achilles tendon that has a sensitive zone, combined with intratendinous swelling, that moves along with the tendon and of which sensitivity increases or decreases when the tendon is put under pressure, there will be a high predictive value that in this situation there is a case of tendinosis.<ref>KL. Luscombe, P. S. (2003). Achilles tendinopathy. Trauma , 215-225.fckLR Level 2C</ref><br>Palpation will show oversensitivity, warmth, swelling and crepitations.
| | == Management / Interventions<br> == |
|
| |
|
| <br> | | {| width="40%" cellspacing="1" cellpadding="1" border="0" align="right" class="FCK__ShowTableBorders" |
| | |- |
| | | align="right" | |
| | | {{#ev:youtube|bZccYojlDvQ|250}} <ref>BJSM Videos. Patellar pubic percussion test, with Mike Reiman. Available from: http://www.youtube.com/watch?v=bZccYojlDvQ [last accessed 25/01/14]</ref> |
| | |} |
|
| |
|
| = Mechanism of Injury / Pathological Process =
| | Treatment of Achilles tendinopathy is initially non-operative, including rest, equipment changes, strength and flexibility exercises, [[Anti-Inflammatory Agents|anti-inflammatory agents]] and corticosteroids. The effects of physical therapy on Achilles tendonitis is poorly understood, although musculotendinous strengthening appears essential. [[Eccentric Exercises|Eccentric exercises]] have been shown to have positive effects of Achilles tendonitis, and remains the gold standard for rehabiliation of this condition.<ref name="Cook et al" /><ref name="Roos et al" /> A study by Roos et al concluded that eccentric exercises improve function and reduce pain and effects were apparent after 6 weeks of treatment, lasting for 1 year.<ref name="Robinson et al" /><br> |
| | |
| = <br>Clinical Presentation <br> =
| |
| | |
| = Diagnostic Procedures =
| |
| | |
| Examination of the Achilles tendon is inspection for muscle atrophy, swelling, asymmetry, joint effusions and erythema. Atrophy is an important clue to the duration of the tendinopathy and it is often present with chronic conditions. Swelling, asymmetry and erythema in pathologic tendons are often observed in the examination. Joint effusions are uncommon with tendinopathy and suggest the possibility of intra-articular pathology. Range of motion testing is often limited on the side of the tendinopathy.<ref>. Hammer, W. I. (1999). Functional Soft Tissue Examination and Treatment by Manual Methods. Aspen: Jones &amp;amp;amp;amp;amp;amp;amp; Bartlett Learning.</ref>, <ref>KL. Luscombe, P. S. (2003). Achilles tendinopathy. Trauma , 215-225.fckLR Level 2C</ref><br>Palpation tends to elicit well-localized tenderness that is similar in quality and location to the pain experienced during activity.<ref>John J. Wilson, T. M. (2005). Common overuse tendon problems: A review and recommendations for treatment. University of Wisconsin Medical School, Madison, Wisconsin , 1-8.fckLR Level 1A</ref><br>Physical examinations of the Achilles tendon often reveals palpable nodules and thickening. Anatomic deformities, such as forefoot and heel varus and excessive pes planus or foot pronation, should receive special attention. These anatomic deformities are often associated with this problem.<ref>John J. Wilson, T. M. (2005). Common overuse tendon problems: A review and recommendations for treatment. University of Wisconsin Medical School, Madison, Wisconsin , 1-8.fckLR Level 1A</ref>, <ref>Shibuya N, T. J. (2012). Is calcaneal inclination higher in patiënts with insertional achilles tendinosis? A case- controlled, cross-sectional study. The journal of foot and ankle surgery , 757-761.fckLR Level 3B</ref><br>In case extra research is wanted, an echography is the first choice of examination when there is a suspicion of tendinosis.<ref>Healy, N. T. (2010). Ultrasound-guided treatments for chronic Achilles tendinopathy: an update and current status . Skeletal Radiol , 39:425–434.fckLR Level 5</ref>
| |
|
| |
|
| <br> | | <br> |
|
| |
|
| = Outcome Measures =
| | Supportive taping can also help manage symptoms: |
|
| |
|
| = <br>Management / Interventions = | | {| width="100%" cellspacing="1" cellpadding="1" class="FCK__ShowTableBorders" |
| | |- |
| | | {{#ev:youtube|xzRhIyw85Xk|300}} <ref>Jenna Beaudry. Achilles Tendonitis Tape Job. Available from: http://www.youtube.com/watch?v=xzRhIyw85Xk [last accessed 01/12/12]</ref> |
| | | {{#ev:youtube|fQAwpCToR48|300}}<ref>Aaron Tomlinson. Achilles Tape Application. Available from: http://www.youtube.com/watch?v=fQAwpCToR48 [last accessed 01/12/12]</ref> |
| | |} |
|
| |
|
| <br>The treatment should be conservative. A popular and effective option is the eccentric strength training. Deep friction massage and stretching of the gastrocnemius and soleus are considered helpful for Achilles tedinopathy.<ref>John J. Wilson, T. M. (2005). Common overuse tendon problems: A review and recommendations for treatment. University of Wisconsin Medical School, Madison, Wisconsin , 1-8.fckLR Level 1A</ref><br>Anatomic deformities can be treated with shoe orthotics. These shoe orthotics correct overpronation or pes planus problems.<ref>John J. Wilson, T. M. (2005). Common overuse tendon problems: A review and recommendations for treatment. University of Wisconsin Medical School, Madison, Wisconsin , 1-8.fckLR Level 1A</ref> | | <br> |
|
| |
|
| <u>Conservative treatment:</u> <ref>Alex Scott, R. P. (2011). Conservative treatment of chronic Achilles tendinopathy. CMAJ , 183(10): 1159–1165.fckLR Level 1A</ref>,<ref>John J. Wilson, T. M. (2005). Common overuse tendon problems: A review and recommendations for treatment. University of Wisconsin Medical School, Madison, Wisconsin , 1-8.fckLR Level 1A</ref><br>In order to treat the symptoms, antiflogistics or other anti-inflammatory therapy are often used. However these forms of therapy usually cannot prevent the injury to live on.<br>Nevertheless patients will always have to be encouraged to execute less burdening activities, so that the burden on the tendon decreases as well. Complete immobilisation should however be avoided, since it can cause atrophy.<br>Passive revalidation:<br>Mobilisations can be used for dorsiflexion limitation of the talocrural joint and varus- or valgus limitation of the subtalar joint.<br>Deep cross frictions (15 min). It’s effectiveness is not scientifically proven and gives limited results. <ref>. Hammer, W. I. (1999). Functional Soft Tissue Examination and Treatment by Manual Methods. Aspen: Jones &amp;amp;amp;amp;amp;amp;amp; Bartlett Learning.</ref>, <ref>Stasinopoulos D, S. I. (2004). Comparison of effects of exercise programme, pulsed ultrasound and transverse friction in the treatment of chronic patellar tendinopathy. Clin Rehabil , 18(4):347-52.fckLR Level 1B</ref>, <ref>James Henry Cyriax, P. J. (1993). Illustrated manual of orthopaedic medicine. Oxford: Elsevier Health Sciences.</ref>, <ref>Joseph MF, T. K. (2012). Deep friction massage to treat tendinopathy: a systematic review of a classic treatment in the face of a new paradigm of understanding. J Sport Rehabil. , 21(4):343-53.fckLR Level 3A</ref>
| | == Differential Diagnosis<br> == |
|
| |
|
| <br>Recently, the use of Extracorporal Shock Wave Therapy was proven.<ref>John J. Wilson, T. M. (2005). Common overuse tendon problems: A review and recommendations for treatment. University of Wisconsin Medical School, Madison, Wisconsin , 1-8.fckLR Level 1A</ref>, <ref>Rompe JD, F. J. (2008). Eccentric loading compared with shock wave treatment for chronic insertional achilles tendinopathy. A randomized, controlled trial. J Bone Joint Surg Am. , (1):52-61.fckLR Level 1B</ref>, <ref>Sten Rasmussen, M. C. (2008). Shockwave therapy for achilles tendinopathy. A double-blind, randomized clinical trail of efficacy. Acta Orthopaedica , 249-256.fckLR Level 1B</ref>
| | [[Ankle Impingement|Posterior ankle impingement]], medial tendinopathy, [[Retrocalcaneal Bursitis|retrocalcaneal bursitis]], [[Sural Nerve|sural nerve]], [[Lumbar Radiculopathy|lumbar radiculopathy]], [[Ankle Osteoarthritis|ankle OA]], [[Deep Vein Thrombosis|DVT]], [[Haglund Deformity|Haglund deformity]], partial [[Achilles Rupture|Achilles tendon rupture]].<ref name="Cook et al" /><br> |
|
| |
|
| Besides that, the application of ice can cause a short decrease in pain and in swelling. Even though cryotherapy 2, 5 was not studied very thoroughly, recent research has shown that for injuries of soft tissue, applications of ice through a wet towel for ten minutes are the most effective measures. <ref>Bleakley C, M. S. (2004). The use of ice in the treatment of acute soft-tissue injury: a systematic review of randomized controlled trials. Am J Sports Med , (1):251-61.fckLR Level 1A</ref>, <ref>Dykstra JH, H. H. (2009). Comparisons of cubed ice, crushed ice, and wetted ice on intramuscular and surface temperature changes. J Athl Train. , (2):136-41.fckLR Level 2A</ref>, <ref>John J. Wilson, T. M. (2005). Common overuse tendon problems: A review and recommendations for treatment. University of Wisconsin Medical School, Madison, Wisconsin , 1-8.fckLR Level 1A</ref>
| | == Resources == |
| | <div class="coursebox"> |
| | {| width="100%" cellspacing="4" cellpadding="4" border="0" class="FCK__ShowTableBorders" |
| | |- |
| | | align="center" | <imagemap> |
| | Image:AchTendToolkit Algorithm.png|140px|border|left| |
| | rect 0 0 220 126 [[Achilles_Tendinopathy_Toolkit]] |
| | desc none |
| | </imagemap> |
| | | [[Achilles Tendinopathy Toolkit]] |
| | The Achilles Tendinopathy Toolkit is a comprehensive evidence based resource to assist practitioners in clinical decision making for Achilles Tendinopathy. |
|
| |
|
| <u>Active revalidation:</u><br>An active exercise program mostly includes eccentric exercises. This can be explained by the fact that eccentric muscle training will lengthen the muscle fibres, which stimulates the collagen production. This form of therapy appears successful for mid-portion tendinosis, but has less effect with insertion tendinopathy. The sensation of pain sets the beginning burdening of the patient and the progression of the exercises.<ref>Bleakley C, M. S. (2004). The use of ice in the treatment of acute soft-tissue injury: a systematic review of randomized controlled trials. Am J Sports Med , (1):251-61.fckLR Level 1A</ref>, <ref>Brett L Woodley, R. J.‐W. (2007). Chronic tendinopathy: effectiveness of eccentric exercise. Br J Sports Med , 41(4): 188–198.fckLR Level 1A</ref>, <ref>John J. Wilson, T. M. (2005). Common overuse tendon problems: A review and recommendations for treatment. University of Wisconsin Medical School, Madison, Wisconsin , 1-8.fckLR Level 1A</ref>
| | [[Achilles Tendinopathy Toolkit|View the Toolkit]] |
|
| |
|
| <u>Hypotheses: </u><br>Stronger/thicker tendon + strengthen pulling power<br>Stretching component influence on elastic tendon characteristics<br>↑ Collagen synthesis <br>↑ tendon perfusion<br>Sclerosing effect on neovascularisation<br>Normalise tendon structures <ref>Brett L Woodley, R. J.‐W. (2007). Chronic tendinopathy: effectiveness of eccentric exercise. Br J Sports Med , 41(4): 188–198.</ref> | | |} |
| | </div> |
| | == Recent Related Research (from [http://www.ncbi.nlm.nih.gov/pubmed/ Pubmed]) == |
| | <div class="researchbox"> |
| | <rss>http://eutils.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=1DeUIcPgNLDEQT17PEJLA26uuKLv4fz4eTsAi9nkGXzfWOXsZF|charset=UTF-8|short|max=10</rss> |
| | </div> |
| | == Presentations == |
| | <div class="coursebox"> |
| | {| width="100%" cellspacing="4" cellpadding="4" border="0" class="FCK__ShowTableBorders" |
| | |- |
| | | align="center" | <imagemap> |
| | Image:Achilles tendonopathy intervention.png|200px|border|left| |
| | rect 0 0 830 452 [https://connect.regis.edu/p41113266/] |
| | desc none |
| | </imagemap> |
| | | [https://connect.regis.edu/p41113266/ '''Achilles Tendonopathy: Intervention'''] |
| | This presentation, created by Shannon Petersen, Clebert LeBlanc, Amy Lavrich, & Kelly Coleman as part of the Regis University OMPT Fellowship, discusses the current best evidence for interventions for Achilles Tendonopathy. |
|
| |
|
| <u>Eccentric exercise program:</u> <ref>Rompe JD, F. J. (2008). Eccentric loading compared with shock wave treatment for chronic insertional achilles tendinopathy. A randomized, controlled trial. J Bone Joint Surg Am. , (1):52-61.fckLR Level 1B</ref>, <ref>Roos EM, E. M. (2004). Clinical improvement after 6 weeks of eccentric exercise in patients with mid-portion Achilles tendinopathy -- a randomized trial with 1-year follow-up. Scand J Med Sci Sports , (5):286-95.fckLR Level 1B</ref><br> 12 weeks <br> perform exercises 1 to 2 times per day (7 days /week)<br> 3 x 15 repeats <br> Recommended to endure pain during exercises, as long as it does not increase progressively over different days. (Should disappear 1 to 2 hours after the exercise)<br>Relative rest in between exercise sessions <br>General warm-up and stretching (for patients with limited dorsiflexion) to be integrated in the exercise sessions.
| | [https://connect.regis.edu/p41113266/ Achilles Tendonopathy: Intervention/ View the presentation] |
|
| |
|
| '''Heel drops''': from toe stance lowering controllably to maximal dorsalflexion. (progression: uni- -> bilateral, with stretched -> bent knee, speed, let patient carry more than 100% of his/her body weight)10<br>You can also perform this exercise with a slightly bent knee, so that the soleul muscle is activated.<br>The calfmuscle should only be loaded eccentrically with the injured leg. The patients must use the uninjured leg (and/or) their arms to get back to the start position, so they don’t perform a concentric loading. When the eccentric loading can be performed painless, a backpack with extra weight can be added, to reach another level of painful training. <ref>Brett L Woodley, R. J.‐W. (2007). Chronic tendinopathy: effectiveness of eccentric exercise. Br J Sports Med , 41(4): 188–198.fckLR Level 1A</ref>, <ref>Fahlström M, J. P. (2003). Chronic Achilles tendon pain treated with eccentric calf-muscle training. Knee Surg Sports Traumatol Arthrosc , (5):327-33.</ref>, <ref>John J. Wilson, T. M. (2005). Common overuse tendon problems: A review and recommendations for treatment. University of Wisconsin Medical School, Madison, Wisconsin , 1-8.fckLR Level 1A</ref>, <ref>MIKA PAAVOLA, M. P. (2002). Current Concepts Review Achilles Tendinopathy . THE JOURNAL OF BONE AND JOINT SURGERY, INCORPORATED , 2062-2076.</ref>, <ref>Rompe JD, F. J. (2008). Eccentric loading compared with shock wave treatment for chronic insertional achilles tendinopathy. A randomized, controlled trial. J Bone Joint Surg Am. , (1):52-61.fckLR Level 1B</ref>, <ref>Silbernagel KG, T. R. (2001). Eccentric overload training for patients with chronic Achilles tendon pain--a randomised controlled study with reliability testing of the evaluation methods. Scand J Med Sci Sports , (4):197-206.fckLR Level 1B</ref>, <ref>Stasinopoulos D, S. I. (2004). Comparison of effects of exercise programme, pulsed ultrasound and transverse friction in the treatment of chronic patellar tendinopathy. Clin Rehabil , 18(4):347-52.fckLR Level 1B</ref><br> <br>[[Image:Heeldrops.png]]
| | |} |
| | | </div> |
| <br>
| | == References == |
| | |
| = Differential Diagnosis =
| |
| | |
| = <br>Key Evidence =
| |
| | |
| = <br>Resources = | |
| | |
| = <br>Case Studies <br><br> = | |
| | |
| = Recent Related Research =
| |
| | |
| <br>
| |
|
| |
|
| = References<br> =
| | References will automatically be added here, see [[Adding References|adding references tutorial]]. |
|
| |
|
| 1. T E O Schubert, C. W. (2005). Achilles tendinosis is associated with sprouting of substance P positive nerve fibres. Ann Rheum Dis , 1083-1086.<br> Level 3B<br>2. K M Khan, a. p. (2002). Time to abandon the “tendinitis” myth: Painful, overuse tendon conditions have a non-inflammatory pathology . BMJ , 324:626.<br> Level 2A<br>3. Evelyn Bass, L. (2012). Tendinopathy: Why the Difference Between Tendinitis and Tendinosis Matters. Int J Ther Massage Bodywork. , 5(1): 14–17.<br> Level 2C<br>4. John J. Wilson, T. M. (2005). Common overuse tendon problems: A review and recommendations for treatment. University of Wisconsin Medical School, Madison, Wisconsin , 1-8.<br> Level 1A<br>5. MIKA PAAVOLA, M. P. (2002). Current Concepts Review Achilles Tendinopathy . THE JOURNAL OF BONE AND JOINT SURGERY, INCORPORATED , 2062-2076.<br>6. Dijk, M. N. (2011). Mid-portion Achilles tendinopathy: why painful? An evidence-based philosophy. Knee Surg Sports Traumatol Arthrosc , 19(8): 1367–1375.<br> Level 5<br>7. KL. Luscombe, P. S. (2003). Achilles tendinopathy. Trauma , 215-225.<br> Level 2C<br>8. Hammer, W. I. (1999). Functional Soft Tissue Examination and Treatment by Manual Methods. Aspen: Jones & Bartlett Learning.<br>9. Shibuya N, T. J. (2012). Is calcaneal inclination higher in patiënts with insertional achilles tendinosis? A case- controlled, cross-sectional study. The journal of foot and ankle surgery , 757-761.<br> Level 3B <br>10. Healy, N. T. (2010). Ultrasound-guided treatments for chronic Achilles tendinopathy: an update and current status . Skeletal Radiol , 39:425–434.<br> Level 5<br>11. Alex Scott, R. P. (2011). Conservative treatment of chronic Achilles tendinopathy. CMAJ , 183(10): 1159–1165.<br> Level 1A<br>12. Stasinopoulos D, S. I. (2004). Comparison of effects of exercise programme, pulsed ultrasound and transverse friction in the treatment of chronic patellar tendinopathy. Clin Rehabil , 18(4):347-52.<br> Level 1B<br>13. James Henry Cyriax, P. J. (1993). Illustrated manual of orthopaedic medicine. Oxford: Elsevier Health Sciences.<br>14. Joseph MF, T. K. (2012). Deep friction massage to treat tendinopathy: a systematic review of a classic treatment in the face of a new paradigm of understanding. J Sport Rehabil. , 21(4):343-53.<br> Level 3A <br>15. Rompe JD, F. J. (2008). Eccentric loading compared with shock wave treatment for chronic insertional achilles tendinopathy. A randomized, controlled trial. J Bone Joint Surg Am. , (1):52-61.<br> Level 1B<br>16. Sten Rasmussen, M. C. (2008). Shockwave therapy for achilles tendinopathy. A double-blind, randomized clinical trail of efficacy. Acta Orthopaedica , 249-256.<br> Level 1B<br>17. Bleakley C, M. S. (2004). The use of ice in the treatment of acute soft-tissue injury: a systematic review of randomized controlled trials. Am J Sports Med , (1):251-61.<br> Level 1A<br>18. Dykstra JH, H. H. (2009). Comparisons of cubed ice, crushed ice, and wetted ice on intramuscular and surface temperature changes. J Athl Train. , (2):136-41.<br> Level 2A<br>19. Brett L Woodley, R. J.‐W. (2007). Chronic tendinopathy: effectiveness of eccentric exercise. Br J Sports Med , 41(4): 188–198.<br> Level 1A<br>20. Roos EM, E. M. (2004). Clinical improvement after 6 weeks of eccentric exercise in patients with mid-portion Achilles tendinopathy -- a randomized trial with 1-year follow-up. Scand J Med Sci Sports , (5):286-95.<br> Level 1B<br>21. Fahlström M, J. P. (2003). Chronic Achilles tendon pain treated with eccentric calf-muscle training. Knee Surg Sports Traumatol Arthrosc , (5):327-33.<br> Level 4<br>22. Silbernagel KG, T. R. (2001). Eccentric overload training for patients with chronic Achilles tendon pain--a randomised controlled study with reliability testing of the evaluation methods. Scand J Med Sci Sports , (4):197-206.<br> Level 1B<br>
| | <references /> |
|
| |
|
| [[Category:Vrije_Universiteit_Brussel_Project]] | | [[Category:Ankle]] [[Category:EIM_Residency_Project]] [[Category:Musculoskeletal/Orthopaedics]] |