Muscle Injuries
Original Editors - Els Van Haver
Top Contributors - Els Van Haver, Naomi O'Reilly, Wanda van Niekerk, Kim Jackson, Lucinda hampton, Vidya Acharya, Nina Lefeber, Admin, Evan Thomas, Jess Bell, Maxime Tuerlinckx, Uchechukwu Chukwuemeka, Mande Jooste, 127.0.0.1, Rachael Lowe and Claire Knott
Introduction[edit | edit source]
Skeletal muscle injuries represent a great part of all traumas in sports medicine, with an incidence from 10% to 55% of all sustained injuries. They should be treated with the necessary precaution since a failed treatment can postpone an athlete’s return to the field with weeks or even months and increase the risk of re-injury.
Types of Skeletal Muscle Injuries[edit | edit source]
Literature does not reveal great consensus when it comes to classifying muscle injuries, despite their clinical importance. However, the most differentiating factor is the trauma mechanism. Muscle injuries can, therefore, be broadly classified as either traumatic (acute) or overuse (chronic) injuries.
Acute injuries are usually the result of a single traumatic event and cause a macro-trauma to the muscle. There is an obvious link between the cause and noticeable symptoms. They mostly occur in contact sports such as rugby, soccer and basketball because of their dynamic and high collision nature[1][2].
Overuse, chronic or exercise-induced injuries are subtler and usually occur over a longer period of time. They result from repetitive micro-trauma to the muscle. Diagnosis is more challenging since there is a less obvious link between the cause of the injury and the symptoms[1]. The below video gives a brief talk on these chronic injuries.
[3]Muscle Strains[edit | edit source]
A strain to the muscle or muscle tendon is the equivalent of a sprain to ligaments. It is a contraction-induced injury in which muscle fibres tear due to extensive mechanical stress. This mostly occurs as a result of a powerful eccentric contraction or over-stretching of the muscle. Muscles will most likely tear during sudden acceleration or deceleration.[4] Therefore, it is typical for non-contact sports with a dynamic character such as sprinting, jumping.[5]
Grade I (Mild)[edit | edit source]
- Involves only a small number of fibres in the muscle.
- There is no decrease in strength and there is full active and passive range of motion.
- Localised pain
- Pain and tenderness are often delayed to the next day.
Grade II (Moderate)[edit | edit source]
- Involves a significant number of muscle fibres torn
- Acute and significant pain is accompanied by swelling
- Pain is reproduced on muscle contraction
- Strength is reduced
- Movement is limited by pain
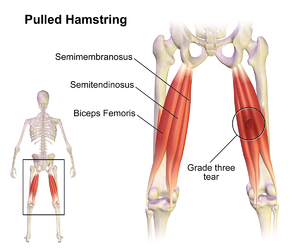
Grade III (Severe)[edit | edit source]
- A complete tear/rupture of the muscle. This means either the tendon is separated from the muscle belly or the muscle belly is actually torn in 2 parts.
- Severe swelling and pain and a complete loss of function are characteristic for this type of strain.
- This is seen most frequently at the musculotendinous junction.
A number of factors predispose an athlete to muscle strains:
Common Strain Injuries[edit | edit source]
- Hamstring Strain
- Quadriceps Muscle Contusion
- Calf Strain
- Groin Strain
- Rotator Cuff Tears
- Rupture Long Head Biceps
- Achilles Rupture
Muscle Contusion[edit | edit source]
A muscle contusion is usually the result of a direct blow from an opposition player or contact with equipment in collision sports, such as football, rugby and hockey. The blow causes local muscle damage with associated bleeding.[4] A bruise, or contusion, is a type of haematoma of tissue in which capillaries and sometimes venules are damaged by trauma, allowing blood to seep, haemorrhage, or extravasate into the surrounding interstitial tissues. Bruises, which do not blanch under pressure, can involve capillaries at the level of skin, subcutaneous tissue, muscle, or bone. As a type of haematoma, a bruise is caused by internal bleeding into the interstitial tissues which do not break through the skin, usually initiated by blunt trauma, which causes damage through physical compression and deceleration forces. Trauma sufficient to cause bruising can occur across a wide range of sports. Bruises often induce pain, but small bruises are not normally dangerous alone. Sometimes bruises can be serious, leading to other more life-threatening forms of haematoma, such as when associated with serious injuries, including fractures and more severe internal bleeding. The likelihood and severity of bruising depend on many factors, including type and healthiness of affected tissues.
Muscle Cramp[edit | edit source]
Muscle cramps are sudden, involuntary muscle contractions or over-shortening. While cramps are generally temporary and non-damaging, they can cause mild-to-excruciating pain and paralysis-like immobility of the affected muscle. The onset is usually sudden, and it resolves on its own over a period of several seconds, minutes, or hours. Cramps may occur in a skeletal muscle or smooth muscle.
Muscle cramps during exercise are very common, even in elite athletes. Muscles that cramp the most often are the calves, thighs, and arches of the foot. Such cramping is associated with strenuous physical activity and can be intensely painful; however, they can even occur while inactive/relaxed. Around 40% of people who experience skeletal cramps are likely to endure extreme muscle pain and may be unable to use the entire limb that contains the "locked-up" muscle group. It may take up to seven days for the muscle to return to a pain-free state.
According to Brukner & Kahn[4] disturbances at various levels of the central and peripheral nervous system and skeletal muscle are involved in the mechanism of cramp and may explain the diverse range of conditions in which cramp occurs. Other popular theories as to the cause of cramps include dehydration, low potassium or low sodium levels, inadequate carbohydrate intake or excessively tight muscles but these hypotheses appear to be falling out of favour as the weight of evidence supports the ‘neural excitability’ hypothesis.[4]
Muscle Soreness[edit | edit source]
Muscle soreness after exercise is commonly referred to as delayed onset muscle soreness (DOMS). DOMS is common in individuals who engage in strenuous and unaccustomed exercise and physical activity. It is classified as a grade 1 muscle strain injury and is characterised by localised tenderness and soreness. It typically peaks between 24 to 72 hours after a bout of exercise but eventually disappears after five to seven days.[9] Soreness is accompanied by a prolonged strength loss, a reduced range of motion, and elevated levels of creatine kinase in the blood. These are taken as indirect indicators of muscle damage, and biopsy analysis has documented damage to the contractile elements. The exact cause of the soreness response is not known but thought to involve an inflammatory reaction to the damage.[10]
Pain perceived during exercise is considered to result from a combination of factors including acids, ions, proteins, and hormones. Although it is commonly believed that lactic acid is responsible for this pain, evidence suggests that it is not the only factor.[10]
Repair Process[edit | edit source]
Regardless of the underlying cause, the processes occurring in injured muscles tend to follow the same pattern. Functional recovery, however, varies from one type of injury to another. Two phases can be distinguished in the repair process[6][11][12].
Destruction Phase [edit | edit source]
Starts with the actual trauma that causes muscle fibres to tear. Immediate necrosis of myofibres takes place due to deterioration of the sarcoplasm, a process that is halted within hours after the trauma by lysosomal vesicles forming a temporary membrane[8]. An inflammatory process takes place as a reaction to the torn blood vessels. Specialised cells start removing necrotised parts of the fibres[13].
Repair and Remodelling Phase[edit | edit source]
The actual repair of the injured muscle takes place. Myofibres start regenerating out of satellite cells (= undifferentiated reserve cells) and a connective tissue scar is being formed in the gap between the torn muscle fibres. In the first 10 days after the trauma, this scar tissue is the weakest point of the affected muscle. After 10 days, however, eventual re-rupture will rather affect adjacent muscle tissue than the scar tissue itself, although full recovery (up to the point of pre-injury strength) can take a relatively long time. Vascularisation of the injured area is a prerequisite for recovering from a muscle injury. New capillaries originate from the remaining injured blood vessels and find their way to the centre of the injured area. Early mobilisation plays a very important role since it stimulates the vascularisation process. Similar wise, intramuscular nerves will regenerate to re-establish the nerve-muscle contact[14][15].
Diagnostic Procedures[edit | edit source]
Both for acute and chronic injuries, thorough subjective examination is primary in identifying muscle injuries. Particular attention to the history of occurrence of the trauma is needed. A clinical examination and testing of the muscle function together with the patient's recollection of what happened, are mostly sufficient for making the right diagnosis. In some cases, additional tests (MRI, X-ray, Ultrasound, CT Scan) may be required to determine the extent of the injury or to identify possible additional injuries.
The video below gives a good insight into diagnostic procedures for muscle injuries[16]Physiotherapy Treatment[edit | edit source]
Acute Skeletal Muscle Injuries[edit | edit source]
These two acronyms (PEACE and LOVE) include the full range of soft tissue injury management from immediate care to subsequent management. It also highlights the importance of patient education and addressing the psychosocial factors involved that will aid recovery. It also highlights the potential harmful effects of using anti-inflammatory medication for recovery.[17]
"Immediately after a soft tissue injury, do no harm and let PEACE guide your approach"[17]
P = Protect[edit | edit source]
E = Elevate[edit | edit source]
A = Avoid anti-inflammatory modalities[edit | edit source]
- anti-inflammatory medications may negatively affect long-term tissue healing
- avoid ice
- use of ice is mostly analgesic
- although it is widely accepted as an intervention there is very little high quality evidence that supports the use of ice in the treatment of soft tissue injuries[23]
- ice may potentially disrupt inflammation, angiogenesis and revascularisation
- ice may potentially delay neutrophil and macrophage infiltration
- ice may potentially increse immature myofibers
- this can result in impaired tissue regeneration and redundant collagen synthesis[24]
E = Educate[edit | edit source]
- It is our responsibility as physiotherapists to educate our patients on the many benefits of an active approach to recovery instead of a passive approach[20]
- Early passive therapy approaches such as electrotherapy, manual therapy or acupuncture after an injury has a minimal effect on pain and function when compared to an active approach[20]
- If physiotherapists nurture a patient's "need to be fixed" it may create dependence to the physio and actually contribute to persistent symptoms[25]
- Patients need to be better education on their condition
- Load management will avoid overtreatment of an injury
- Overtreatment may increase the likelihood of injections or surgery and higher costs[26]
- It is critical for physiotherapists to educate their patients and set realistic expectations about recovery times[17]
"After the first days have passed, soft tissues need LOVE"
L = Load[edit | edit source]
- Patients with musculoskeletal disorders benefit from an active approach with movement and exercises[27]
- Normal activities should continue as soon as symptoms allow for it
- Early mechanical stress is indicated
- Optimal loading without increasing pain
O = Optimism[edit | edit source]
- The brain plays a significant part in rehabilitation interventions[28]
- Barriers of recovery include psychological factors such as:
- catastrophisation
- depression
- fear
- research shows that these factors may more explain the variation in symptoms and limitations after an ankle sprain than the degree of pathophysiology[29]
V = Vascularisation[edit | edit source]
- Musculoskeletal injury management needs to include cardiovascular physical activity[28]
- more research is needed on specific dosage, but pain free cardiovascular activity is a motivation booster and it increases blood flow to injured structures
- Benefits of early mobilisation and aerobic exercise in people with musculoskeletal disorders include:
- improvement in function
- improvement in work status
- reduces the need for pain medication[31]
E = Exercise[edit | edit source]
- Evidence supports the use of exercise therapy in the treatment of ankle sprains and it reduces the risk of a recurring injury
- Benefits of exercise:
- restores mobility
- restores strength
- restores proprioception, early after an injury[21]
- Avoid pain to promote optimal repair in the subacute phase
- Use pain as a guide to progress exercises gradually to increased levels of difficulty[17]
Evidence for early mobilisation[edit | edit source]
After first aid, therapy must be tailor-made according to the severity and extent of the injury. A short period of immobilisation after the trauma prevents excessive formation of scar tissue (which will have a deleterious effect on mobility and strength of the healed muscle) and prevents re-rupture by allowing the scar tissue to gain sufficient strength to bear contraction forces. Immobilisation should not be continued after the acute phase (first few days) to avoid the negative effects such as muscle atrophy, retarded strength recovery and excessive formation of connective tissue within the muscle[14].
Early mobilisation already starts after a few days, if the acute phase has passed without further complications and recovery seems to be progressing. In comparison to immobilisation, mobilisation induces significant histological changes such as increased vascularisation of the injured area, better regeneration of muscle fibres and more parallel orientation. It has the additional advantage that the muscle will sooner gain its original strength[6][32][7].
The active treatment needs to be built up gradually from isometric exercises to isotonic exercises. Only if those exercises can be performed without pain, isokinetic training should be started.
As muscle injuries generally recover well with conservative treating, surgical intervention is only to be considered in cases with very specific indications[6]:
- Large intramuscular haematoma
- Complete muscle tear ( strain of third degree)
- Partial strain (2nd degree) if more than half of the muscle belly is affected
- Scar adhesions that cause persistent pain and limited extension (>4-6 months)
Chronic Skeletal Muscle Injuries[edit | edit source]
Overuse sports injuries outnumber acute, instantaneous injuries in almost every athletic activity. Because they do not instantly, disable the person, they attract less medical attention than acute injuries. Their frequency of occurrence is almost always underestimated in surveys of athletic injuries. The treatment of overuse sports injuries is made difficult by various factors e.g. an insidious onset. When athletes actually present for treatment, the injuries are well established and more difficult to manage successfully.
Injury occurs when cumulative forces exceed the tissue’s ability to withstand such forces— either due to isolated macro traumatic events or repetitive micro-traumatic events. Often, specific biomechanical or physiological factors predispose an athlete to injury. A physiotherapist should properly identify and assist the athlete in correcting these conditions to treat, prevent, and possibly reverse the detrimental effects. As always, prevention is always the best treatment but, failing that, the next best thing is proper and successful rehabilitation.[33]
Clinical Bottom Line[edit | edit source]
Treatment of muscle injuries usually has good outcomes. Physiotherapists must ensure the muscle is rehabilitated in all functional aspects before resuming usual activities or high demand sporting activities. The management of soft tissue injuries, whether it is a hamstring strain or an ankle sprain, should not just focus on short-term damage control.[17] Clinicians should also focus on long-term outcomes and focus on treating the person with the injury and not just treating the injury of the person.[17]
References[edit | edit source]
- ↑ 1.0 1.1 Best TM. Soft-tissue injuries and muscle tears. Clin Sports Med. Jul 1997; 16(3):419-34
- ↑ Beiner J, Jokl P. Muscle Contusion Injuries: Current Treatment Options. J Am Acad Orthop Surg July 2001; 9:227-237
- ↑ Universal Hospitals Common muscle and sports injuries Available from: https://www.youtube.com/watch?v=EkdllXH5AME (last accessed 7.6.2019)
- ↑ 4.00 4.01 4.02 4.03 4.04 4.05 4.06 4.07 4.08 4.09 4.10 4.11 Brukner P. Brukner & Khan's Clinical Sports Medicine. McGraw-Hill Education; 2017.
- ↑ Garrett WE. Muscle strain injuries. Am J Sports Med. 1996; 24:S2-88
- ↑ 6.0 6.1 6.2 6.3 6.4 Tero AH Järvinen, Teppo LN Järvinen, Minna Kääriäinen, Hannu Kalimo, Markku Järvinen. Basic Science Update: Muscle Treatment. Am J Sports;May;33:745-­‐764
- ↑ 7.0 7.1 Järvinen M, Tero AH. Muscle strain injuries. Rheumatology. 2010(2); 12: 155-161
- ↑ 8.0 8.1 Kneeland JP. MR imaging of muscle and tendon injury. Eur J Radiol. Nov 1997; 25(3):198-208
- ↑ Ranchordas MK, Rogerson D, Soltani H, Costello JT. Antioxidants for preventing and reducing muscle soreness after exercise. Cochrane Database of Systematic Reviews. 2017(12).
- ↑ 10.0 10.1 Miles MP, Clarkson PM. Exercise-induced muscle pain, soreness, and cramps. The Journal of sports medicine and physical fitness. 1994 Sep;34(3):203-16.
- ↑ Kalimo H, Rantanen J, Järvinen M. Muscle injuries in sports. Baillieres Clin Orthop. 1997;2: 1-24
- ↑ Huard J, Li Y, Fu FH. Muscle injuries and repair: Current trends in research. J Bone Joint Surg AM. 2002; 84:822-832
- ↑ Kasemkijwattana C, Menetrey J, Somogyl G, et al. Development of approaches to improve the healing following muscle contusion. Cell Transplant. Nov-Dec 1998; 7(6):585-98
- ↑ 14.0 14.1 Järvinen M, Sorvari T. A histochemical study of the effect of mobilization and immobilization on the metabolism of healing muscle injury. In: Landry F, ed. Sports Medicine. Miami, Fla: Symposia Specialists, Orban WAR; 1978:177-181
- ↑ Nozaki M, Li Y, Zhu J, et al. Improved muscle healing after contusion injury by the inhibitory effect of suramin on myostatin, a negative regulator of muscle growth. Am J Sports Med Dec 2008; 36(12): 2354-62
- ↑ Chris Beaulieu Muscle injuries and interventions. Available from: https://www.youtube.com/watch?v=MPqjFEhEBB4&app=desktop (last accessed 7.6.2019)
- ↑ 17.0 17.1 17.2 17.3 17.4 17.5 17.6 17.7 Dubois B, Esculier J. Soft-tissue injuries simply need PEACE and LOVE. British Journal of Sports Medicine 2020;54:72-73.
- ↑ Bleakley CM, Davison G. Management of acute soft tissue injury using protection rest ice compression and elevation: recommendations from the Association of Chartered Physiotherapists in sports and exercise medicine (ACPSM)[executive summary]. Association of Chartered Physiotherapists in Sports and Exercise Medicine. 2010:1-24.
- ↑ 19.0 19.1 19.2 Bleakley CM, Glasgow P, MacAuley DC. PRICE needs updating, should we call the POLICE?British Journal of Sports Medicine 2012;46:220-221.
- ↑ 20.0 20.1 20.2 Doherty C, Bleakley C, Delahunt E, Holden S. Treatment and prevention of acute and recurrent ankle sprain: an overview of systematic reviews with meta-analysis. British journal of sports medicine. 2017 Jan 1;51(2):113-25.
- ↑ 21.0 21.1 Vuurberg G, Hoorntje A, Wink LM, Van Der Doelen BF, Van Den Bekerom MP, Dekker R, Van Dijk CN, Krips R, Loogman MC, Ridderikhof ML, Smithuis FF. Diagnosis, treatment and prevention of ankle sprains: update of an evidence-based clinical guideline. British journal of sports medicine. 2018 Aug 1;52(15):956-.
- ↑ Duchesne E, Dufresne SS, Dumont NA. Impact of inflammation and anti-inflammatory modalities on skeletal muscle healing: from fundamental research to the clinic. Physical therapy. 2017 Aug 1;97(8):807-17.
- ↑ van den Bekerom MP, Struijs PA, Blankevoort L, Welling L, Van Dijk CN, Kerkhoffs GM. What is the evidence for rest, ice, compression, and elevation therapy in the treatment of ankle sprains in adults?. Journal of athletic training. 2012 Jul;47(4):435-43.
- ↑ Singh DP, Barani Lonbani Z, Woodruff MA, Parker TJ, Steck R, Peake JM. Effects of topical icing on inflammation, angiogenesis, revascularization, and myofiber regeneration in skeletal muscle following contusion injury. Frontiers in physiology. 2017 Mar 7;8:93.
- ↑ Lewis J, O’Sullivan P. Is it time to reframe how we care for people with non-traumatic musculoskeletal pain?British Journal of Sports Medicine 2018;52:1543-1544.
- ↑ Graves JM, Fulton‐Kehoe D, Jarvik JG, Franklin GM. Health care utilization and costs associated with adherence to clinical practice guidelines for early magnetic resonance imaging among workers with acute occupational low back pain. Health services research. 2014 Apr;49(2):645-65.
- ↑ 27.0 27.1 Khan KM, Scott A. Mechanotherapy: how physical therapists’ prescription of exercise promotes tissue repair. British journal of sports medicine. 2009 Apr 1;43(4):247-52.
- ↑ 28.0 28.1 Lin I, Wiles L, Waller R, Goucke R, Nagree Y, Gibberd M, Straker L, Maher CG, O’Sullivan PP. What does best practice care for musculoskeletal pain look like? Eleven consistent recommendations from high-quality clinical practice guidelines: systematic review. British journal of sports medicine. 2020 Jan 1;54(2):79-86.
- ↑ Briet JP, Houwert RM, Hageman MG, Hietbrink F, Ring DC, Verleisdonk EJ. Factors associated with pain intensity and physical limitations after lateral ankle sprains. Injury. 2016 Nov 1;47(11):2565-9.
- ↑ Bialosky JE, Bishop MD, Cleland JA. Individual expectation: an overlooked, but pertinent, factor in the treatment of individuals experiencing musculoskeletal pain. Physical therapy. 2010 Sep 1;90(9):1345-55.
- ↑ Bleakley CM, O’Connor SR, Tully MA, Rocke LG, MacAuley DC, Bradbury I, Keegan S, McDonough SM. Effect of accelerated rehabilitation on function after ankle sprain: randomised controlled trial. Bmj. 2010 May 10;340.
- ↑ Järvinen M, Lehto MUK. The effect of early mobilization and immobilization on the healing process following muscle injuries. Sports Med. 1993; 15:78-89
- ↑ Elmer G. Pinzon, MD, MPH, DABIPP and Mick Larrabee, PT, MS, SCS, EMT, CSCS Chronic Overuse Sports Injuries Available from: https://www.practicalpainmanagement.com/pain/acute/sports-overuse/chronic-overuse-sports-injuries (last accessed 7.6.2019)