Communicable Diseases
Original Editor - Your name will be added here if you created the original content for this page.
Top Contributors - Naomi O'Reilly, Lucinda hampton, Kim Jackson, Tony Lowe, Admin, Vidya Acharya, Khloud Shreif, Olajumoke Ogunleye, Niha Mulla, 127.0.0.1, Laura Ritchie, Oyemi Sillo, Tarina van der Stockt, WikiSysop and Jess Bell
Introduction[edit | edit source]
According to the World Health Organisation “over 13 million people die each year from Infectious and Parasitic Diseases: One in two deaths in some developing countries. Poor people, women, children, and the elderly are the most vulnerable. Infectious diseases continue to be the world’s leading killer of young adults and children” [1].
Socioeconomic, environmental and behavioural factors, as well as international travel and migration, foster and increase the spread of Communicable Diseases. Vaccine-preventable, foodborne, zoonotic, health care-related and communicable diseases pose significant threats to human health and may sometimes threaten international health security [2].
What are Communicable Diseases[edit | edit source]
Communicable disease is one that is spread from one person to another through a variety of methods. How these diseases spread depends on the specific disease or infectious agent and include:
- Physical contact with an infected person, such as through Touch (e.g. Staphylococcus), Sexual Intercourse (e.g. Gonorrhea, HIV), Fecal/Oral Transmission (Hepatitis A), or Droplets (Influenza, Tuberculosis)
- Contact with a contaminated surface or object (Norovirus), Food (Salmonella, E. Coli), Blood (HIV, Hepatitis B), or Water (Cholera);
- Bites from insects or animals capable of transmitting disease (e.g. Mosquito: Malaria, Zika Virus and Yellow Fever; Flea: Plague; Tick: Lyme Disease); and
- Travel through the air (e.g. Tuberculosis or Measles)
Refresh your knowledge of some common communicable diseases:
• Pneumonia
• HIV/AIDS
• Tuberculosis
• Malaria
Review your knowledge of Antibiotic Resistant Diseases which are frequent within the Hospital Setting.
• Methicillin-Resistant Staphylococcus Aureus (MRSA)
• Clostridium Difficile Infection (CDif)
You can also check out our Infectious Disease Category which provides information on many other infectious conditions:
• Infectious Diseases
Risk Factors[edit | edit source]
Modifiable Risk Factors[edit | edit source]
Refer to characteristics that individuals or societies can change to reduce risk of infectious disease and improve health outcomes. WHO typically refers to four major ones for Commuicable Disease: Hygiene, Vaccinations and Food Preparation methods.
Signs & Symptoms [edit | edit source]
Depending on the etiology (eg. virus, bacteria), the systems involved (e.g. respiratory, cardiovascular, central nervous system) and stage of disease (e.g. acute, chronic) the clinical manifestations of Communicable Diseases will vary widely and may be local to the site of infection (eg, cellulitis, abscess) or systemic (most often fever). Manifestations may also develop in multiple organ systems and severe, generalised infections may have life-threatening manifestations (eg, sepsis, septic shock). [3] [4]
Cardiovascular [edit | edit source]
- Tachycardia
- Bradycardia
- Hypotension
- Tachypnea
- Dyspnea
- Cough
- Hoarseness
- Sore Throat
- Nasal Drainage
- Sputum Production
- Oxygen Desaturation
- Decreased Activity/Exercise Tolerance
Central Nervous System [edit | edit source]
- Altered Conciousness
- Confusion
- Delirium
- Stupor
- Coma
- Seizure
- Headache
- Photophobia
- Memory Loss
- Stiff Neck
- Myalgia
Endocrinology
[edit | edit source]
- Increased Thyroid-stimulating Hormone
- Increased Vasopressin
- Increased Insulin
- Increased Glucagon
- Hyperglycemia
- Hypoglycemia
Gastrointestinal[edit | edit source]
- Nausea
- Vomitting
- Diarrhea
Geniturinary[edit | edit source]
- Heamaturia
- Dysuria
- Oliguria
- Proteinuria
- Urgency
- Frequency
Haematology[edit | edit source]
- Increased Immature Neutrophils
- Increased Mature Neutrophils
- Release Granulocytes
- Increased Leukocytes
- Thrombocytopenia
Integumentary[edit | edit source]
- Purulent Drainage
- Skin Rash
- Red Streaks
- Bleeding from Gums
- Bleeding into Joints
- Erythema
- Joint Effusions
Systemic[edit | edit source]
- Fever
- Chills
- Malaise
- Enlarged Lymph Nodes
- Changes in Mental Status
- Fatigue
- Lethargy
- Altered Appetite
Implications for Physiotherapy[edit | edit source]
As healthcare workers it is important that we recognise the symptoms of the most important infectious diseases and direct those affected to appropriate treatment as quickly as possible. It is also important to be aware of the role physiotherapy has in treating and advising patients presenting with these diseases (e.g. the benefits of exercise for patients with HIV/AIDS).
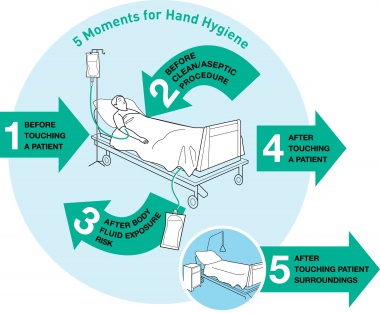
The statistics related to HealthCare Associated Infections make it clear Hand Hygiene in the healthcare environment is extremely important. As physiotherapists we need to learn how to use the alcohol hand rubs effectively and utilise these frequently. The WHO Guidelines identify 5 moments for Hand Hygiene:
- Before Touching the Patient Why? Protect the patient from acquiring germs that might be on your hands. Clean your hands prior to personal care activities like bathing, dressing, brushing and oral care, as well as non-invasive observations (taking vital signs) and treatments.
- Before Clean/Aseptic Procedure Why? Protect the patient from harmful germs, including their own, that could enter the body during procedures like needle insertions, medication administration and connecting to invasive medical devices like EEGs.
- After Body Fluid Exposure Risk Why? Protect yourself and the patient’s surroundings from harmful patient germs generated via contact with fluids like blood, saliva, mucous, semen, tears or urine.
- After Touching a Patient Why? Protect yourself and the immediate environment from harmful patient germs. After you touch a patient, you could have microorganisms on your hands that would get passed on to other patients.
- After Touching Patient Surroundings Why? Protect yourself and the immediate surroundings from harmful patient germs.
 [5] [5]
|
[6] |
Resources[edit | edit source]
Recent Related Research (from Pubmed)[edit | edit source]
Extension:RSS -- Error: Not a valid URL: Feed goes here!!|charset=UTF-8|short|max=10
References[edit | edit source]
References will automatically be added here, see adding references tutorial.
- ↑ World Health Organization. Communicable Disease Prevention, Control and Eradication. http://www.who.int/countries/eth/areas/cds/en/ (accessed 21 Dec 2016)
- ↑ World Health Organization. Infectious Diseases. http://www.who.int/topics/infectious_diseases/en/ (accessed 21 Dec 2016)
- ↑ Merck Manual Professional Version. Manifestations of Infection. http://www.merckmanuals.com/professional/infectious-diseases/biology-of-infectious-disease/manifestations-of-infection (accessed 16 Dec 2016)
- ↑ Goodman CC, Fuller KS. Pathology: implications for the physical therapist. Elsevier Health Sciences; 2014 Nov 5.
- ↑ DebMed. 5 Moments vs. 2 Moments. What is enough when it comes to Hand Hygiene?. http://blog.debmed.com/blog/5-moments-vs.-2-moments.-what-is-enough-when-it-comes-to-hand-hygiene (accessed 2 Dec 2016).
- ↑ Huang Shouyung. WHO Hand Hygiene Video https://youtu.be/s08yiZBSGOw (accessed 2 Dec 2016).






