Patellar Fractures: Difference between revisions
Lise De Wael (talk | contribs) No edit summary |
No edit summary |
||
| (81 intermediate revisions by 17 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> '''Original Editor '''- [[User:Rachael Lowe|Rachael Lowe]] | |||
'''Original | |||
''' | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | </div> | ||
== Definition/Description == | |||
[[Patella]] fractures are caused by direct trauma or compressive force, or as the indirect result of quadriceps contractions or excessive stress to the extensor mechanism.<ref name=":1">Frobell R., Cooper R., Morris H., Arendt H. Acute knee injuries. In: Brukner P., Bahr R., Blair S., Cook J., Crossley K., McConnell J., McCrory P., Noakes T., Khan K. Clinical Sports Medicine: 4th edition. Sydney: McGraw-Hill. 2012; 626-683.</ref><ref name=":2">Schuett D., Hake M., Mauffrey C., Hammerberg E., Stahel P., Hak D. [https://www.researchgate.net/profile/Dustin_Schuett/publication/278788220_Current_Treatment_Strategies_for_Patella_Fractures/links/568ca26008aeb488ea2fdd6f/Current-Treatment-Strategies-for-Patella-Fractures.pdf Current treatment strategies for patella fractures.] Orthopedics. 2015;38(6):377-84.</ref><ref name=":3">Archdeacon M., Sanders R. Chapter 54 - Patella Fractures and Extensor Mechanism Injuries. In: Browner B.D., Jupiter J.B., Krettek C., Anderson P.A., (eds). Skeletal Trauma, 4th edition. Elsevier Health Sciences, 2008.</ref> Indirect injuries are commonly associated with tears of the retinaculum and [[Quadratus Femoris|quadriceps muscles]].<ref name=":1" /> Patella fractures make up about 1% of all skeletal injuries and are found in all age groups.<ref>Crowther M., Mandal A., Sarangi P. [https://bjsm.bmj.com/content/39/2/e6.full Propagation of stress fracture of the patella.] British journal of sports medicine 2005;39(2):e6.</ref><ref>Sweetnam R. [https://pmj.bmj.com/content/postgradmedj/40/467/531.full.pdf Patellectomy.] Postgraduate medical journal 1964 Sep;40(467):531. | |||
</ref><ref name=":13" /> | |||
== Clinically relevant anatomy == | |||
The patella is a triangular bone situated on the anterior surface of the knee at the distal end of the femur. It is the largest sesamoid bone in the body and makes part of the [[Knee|knee joint]].<ref>Cedars-Sinai. Fractured Kneecap. Cedars Sinai organisation. https://www.cedars-sinai.org/health-library/diseases-and-conditions/f/fractured-kneecap.html (accessed 25/07/2018).</ref><ref>Schunke M. Anatomische atlas Prometheus, algemene anatomie en bewegingsapparaat. Bohn Stafieu van Loghum: 2e druk. 2010.</ref><ref>Everett L. Knee and Lower Leg. In: Marx J, Walls R, Hockberger R, editors. Rosen's Emergency Medicine: Concepts and Clinical Practice. 6th ed. Philadelphia: Mosby Elsevier, 2006.</ref> The patella 's primary role is to function as a fulcrum with the aim to increase the moment arm of the quadriceps muscle and thus, knee extensive capacity. <ref name=":14" /> | |||
= | [[Vastus Medialis|Vastus medialis]] and [[Vastus Lateralis|lateralis]], as part of the quadriceps group, control movement at the [[patella]].<ref>Orthopaedia. Collaborative Orthopaedic Knowledgebase, http://www.orthopaedia.com/display/Main/Patella+fractures (accessed November 10, 2010).</ref> The medial retinaculum, formed by the vastus medialis and quadriceps aponeurosis and lateral retinaculum, formed by the vastus lateralis and the ilotibial band, all aid in the extension of the knee. <ref name=":13" /> | ||
The extensor mechanism as a whole plays a major role in patella fractures. The extensor mechanism consists of the quadriceps, quadriceps tendon, retinaculum, patella tendon, tibial tubercle and patellofemoral and patellotibial ligaments.<ref name=":11" /> See the page on the [[patella]] for more details on the anatomy. | |||
{| | |||
|- | |||
|[[File:658px-Knee diagram.svg.png|center|thumb]] | |||
|[[File:Knee joint.png|center|thumb]] | |||
|} | |||
== | == Epidemiology == | ||
A 2016 study found the incidence of patella fracture to be 13.1/100,000 per year with an increasing incidence with increasing age<ref name=":12">Larsen P., Court-Brown C., Vedel J., Vistrup S., Elsoe R. Incidence and Epidemiology of Patellar Fractures. Orthopedics; 2016 Nov 1;39(6):e1154-e1158.</ref>. Females accounted for 56% of patella fractures and males accounted for 44% of patella fractures. <ref name=":12" /> A newer Swedish study also found that older (>65 years old) females had a higher percentage of patellar fractures (64%) compared to males . <ref name=":15">Kruse M, Wolf O, Mukka S, Brüggemann A. [https://link.springer.com/article/10.1007/s00068-022-01993-0 Epidemiology, classification and treatment of patella fractures: an observational study of 3194 fractures from the Swedish Fracture Register]. European Journal of Trauma and Emergency Surgery. 2022 May 30:1-8.</ref> Most fractures were caused by low-energy trauma, with 70% due to simple falls, especially in the winter months. <ref name=":15" /> | |||
Patella fractures are not associated with an increased mortality rate, as the relative risk of death was 0.9.<ref>Larsen P., Elsoe R. [https://www.sciencedirect.com/science/article/pii/S0020138318303590 Patella fractures are not associated with an increased risk of mortality in elderly patients]. Injury 2018; 49(10):1901-1904.</ref> In a recent study, the average mortality rate at one year after patella fractures was 2.8%, increasing to 6.2% in the geriatric population. | |||
== Complications == | |||
* Injuries (sprain/rupture) to ligaments and tendons attached to the patella | |||
* [[Avascular Necrosis|Avascular necrosis]]<ref name=":4">Medscape. Patella Fracture Imaging. http://emedicine.medscape.com/article/394270-overview&gt (accessed 25/07/2018). | |||
</ref> | |||
* [[Post-traumatic arthritis]] | |||
* Osteochondral damage to [[Patellofemoral Joint|patellofemoral joint]] | |||
* Stiffness | |||
* Non-union | |||
* Malunion | |||
* Concomitant injuries (e.g. injuries to the [[Hip Anatomy|acetabulum]], [[femur]] and [[tibia]]) | |||
* Long term complications:<ref>Insall JN. Fractured kneecap: treatments. Institute for Orthopaedics and sports medicine 2007.</ref> | |||
** Stiffness | |||
** Extension weakness | |||
** Patellofemoral arthritis. | |||
<ref name=":1" /> | |||
== Characteristics/Clinical Presentation == | == Characteristics/Clinical Presentation == | ||
=== Types of fractures === | |||
Patella fractures are classified as either displaced or non-displaced. Displaced fractures are unstable and can be further classified as:<ref name=":5" /> | |||
* Comminuted: As a result of direct trauma (mostly due to blows or falls on flexed knee) | |||
** Can cause damage to the articular cartilage of patella and femoral condyles. | |||
* Transverse/stellate: As a result of muscle contraction/extensive stress on the extensor mechanism, e.g. explosive quadriceps contraction after jumping from height. | |||
** Most common type<ref name=":12" /> | |||
** Proximal blood supply may be compromised | |||
** Usually as a result of hyper-flexion of the knee | |||
* Marginal: As a result of a fall on the knee | |||
* Vertical/longitudinal | |||
* Lower/upper pole | |||
* Osteochondral | |||
* Sleeve (only in paediatric patients) | |||
<ref name=":2" /><ref name=":3" /><ref name=":4" /><ref name=":5">Whittle P. Fractures of the Lower Extremity. In: Canale S., Beaty J., (eds). Campbell's Operative Orthopaedics. 11th ed. Philadelphia: Mosby Elsevier, 2008.</ref><ref name=":14">Melvin S.J., Mehta S. [https://journals.lww.com/jaaos/Abstract/2011/04000/Patellar_Fractures_in_Adults.4.aspx Patellar fractures in adults.] Journal of the American Academy of Orthopaedic Surgeons 2011;19(4):198-207.</ref><ref name=":7">Walters J. (ed). Orthopaedics - A guide for practitioners. 4th Edition. Cape Town: University of Cape Town, 2010.</ref> | |||
= | The prognosis of the injury depends on the amount of chondral damage at the time of injury. Functional outcome depends on the ability to achieve pain-free and stable range of motion in an early stage. <ref name=":6">Mehling I., Mehling A., Rommens P. [https://www.sciencedirect.com/science/article/pii/S026808900600168X Comminuted patellar fractures.] Current Orthopaedics 2006;20(6):397-404.</ref> | ||
== Differential diagnosis == | |||
* Bipartite patella<ref name=":1" /> | |||
* [[Multiligament Injured Knee Dislocation|Knee dislocation]] | |||
* [[Patellar dislocation|Patella dislocation]] | |||
== | == Diagnosis == | ||
=== Interview === | |||
* Details regarding accident | |||
* Mechanism of injury | |||
* Pain at knee | |||
* Complaints of difficulty standing or snapping sensation at knee | |||
<ref name="p4">Günal I., Karatosun V. [https://journals.lww.com/clinorthop/Fulltext/2001/08000/Patellectomy__An_Overview_With_Reconstructive.12.aspx Patellectomy: an overview with reconstructive procedures.] Clinical Orthopaedics and Related Research 2001;389:74-8.</ref><ref name=":8">McRae R., Esser M. Practical fracture treatment E-book. Churchill Livingstone/ Elsevier; 2002.</ref><ref name=":9">Fourati MK. Reeducation du genou après fracture de la rotule. Ann. Kinésitherapie 1986.</ref> | |||
== | === Physical examination === | ||
* Observation: | |||
** Whole extremity | |||
** Swollen, bruised knee | |||
** Deformity around knee | |||
** Possible wounds (open fracture) | |||
* Palpation (often done after local anesthetics to eliminate pain): | |||
** Tenderness around patella | |||
** Palpable gap (for displaced fractures) | |||
* Rule out concomitant injuries: | |||
** e.g. fractures of the acetabulum, femur and tibia | |||
* Haemarthrosis | |||
* Range of motion: | |||
** Acute: | |||
*** Limited knee and painful knee flexion and extension | |||
*** Often unable to do straight leg raise | |||
** Chronic: | |||
*** Full knee flexion with extension lag | |||
* Distal pulses | |||
* Assess compartment of the leg | |||
* Neurological assessment | |||
<ref name=":7" /><ref name="p4" /><ref>Scolaro J, Bernstein J, Ahn J. [https://link.springer.com/article/10.1007/s11999-010-1537-8 In brief: patellar fractures]. Clinical Orthopaedics and Related Research®. 2011 Apr;469(4):1213-5.</ref> | |||
== | === Special investigations === | ||
[[X-Rays|X-rays]]: | |||
* AP view: | |||
** May be difficult to see patella | |||
* Lateral view: | |||
** Undisplaced - < 2mm separation | |||
** Displaced - > 2mm separation, step deformity noted | |||
* Sky view | |||
* Used for regular monitoring of healing process and any possible complications | |||
{| | |||
|- | |||
|[[File:Patella fracture.JPG|thumb|AP view]] | |||
|[[File:Patella fracture latview.jpg|thumb|Lateral view]] | |||
|} | |||
* [[CT Scans|CT scan]]: Usually not needed | |||
* [[MRI Scans|MRI]]: Diagnosis of associated injuries to nearby tendons and ligaments | |||
* Bone scans: To identify stress fractures | |||
<ref name=":7" /><ref name=":8" /><ref name=":9" /><ref name=":11" /> | |||
== Outcome measures == | |||
* [http://www.physio-pedia.com/Knee_Injury_and_Osteoarthritis_Outcome_Score Knee injury and osteoarthritis outcome score] | |||
* [http://www.physio-pedia.com/Knee_outcome_survey Knee outcome survey] | |||
* [http://www.physio-pedia.com/Lower_Extremity_Functional_Scale_%28LEFS%29 Lower extremity function scale] | |||
* [http://www.physio-pedia.com/McGill_Pain_Questionnaire McGill pain questionnaire] | |||
== Medical management == | |||
* In acute cases, local anesthetics can be given to eliminate pain.<ref name="p4" /> This helps to aid in the assessment and diagnosis of the patella fracture. | |||
== | === Conservative management === | ||
Indication: Nondisplaced fracture (mostly vertical, horizontal and comminuted fractures) with extensor mechanism in place <ref name=":1" /><ref name=":6" /> | |||
Management:<ref name=":7" /><ref name=":6" /><ref name=":11">Duke Orthopaedics. Wheeless’ textbook of Orthopaedics. Fractures of the patella.http://www.wheelessonline.com/ortho/fractures_of_the_patella (accessed November 10 2010).</ref><ref name=":10">American Academy of Orthopaedic Surgeons. Diseases and conditions - Patellar (Kneecap) Fractures. http://orthoinfo.aaos.org/topic.cfm?topic=A00523 (accessed November 10 2010).</ref> | |||
* Fracture immobilized with POP cylinder cast or range of motion brace locked in extension (4-6 weeks): | |||
** As healing takes place, knee flexion can gradually be increased | |||
** Range of motion brace must be worn until union (on X-rays) and clinical signs of healing (not tender on palpation) are present | |||
* Crutch walking 6-8 weeks | |||
* Rehabilitation to restore full range of motion, strength, and return to function | |||
== | === Surgical intervention === | ||
Indication: Significant displacement with extensor mechanism not intact<ref name=":1" />or articular step off >2-3mm or fracture displacement >1-4 mm. <ref name=":13">Posner A., Zimmerman J. [https://www.scientificarchives.com/admin/assets/articles/pdf/surgical-management-of-patella-fractures-a-review-20220302120317.pdf Surgical management of patella fractures: a review.] Archives of Orthopaedics 2022; 3(1):17-21. </ref> | |||
Aim: Restore extensor function, align articular incongruities, and allow early motion<ref name=":6" /><ref name=":9" /><ref>Shang ZG. Patellar fractures treatment and management. Unbound medline 2013;26(6):445-8.</ref><ref name=":0">Strauss J. ORIF Patella Fracture Post-Operative Rehabilitation Protocol, Hospital for Joint Diseases, 2008.</ref> | |||
Management:<ref name=":1" /><ref name=":7" /> | |||
* Transverse/simple, comminuted mid-patella fracture: Open reduction and internal fixation using tension band wire technique using pins and wires and 'a figure of eight' to press the pieces together | |||
** POP cast in extension for 6 weeks | |||
[[File:Patella ORIF.png|center|thumb|Tension band wire ORIF]] | |||
* Proximal/distal <1/3 - simple or comminuted: Excision of small piece & tendon repair | |||
** POP cast for 6 weeks | |||
* Longitudinal (uncommon): Interfragmentary screw fixation | |||
* Comminuted fracture/irreducible or irreparable fracture or when cartilage too badly damaged: Partial vs complete patellectomy:<ref name="p4" /> | |||
** Quadriceps muscles is is attached to the patellar ligament to ensure function of the extensor apparatus during a complete patellectomy<ref name="p4" /> | |||
** Patellectomy: Relatively old procedure, <u>last treatment of choice</u> due to significant loss of extension | |||
* Repair of bilateral vastus muscles | |||
* Rehabilitation same as with conservative management<br> | |||
'''Later stages''': | |||
Manipulation under anesthesia or the arthroscopic releasing of adhesions is required when athrofibrosis occurs.<ref name=":6" /> | |||
== | == Physiotherapy management == | ||
As clinical healing phases do not always correlate with theoretical healing, the surgeon will guide rehabilitation while taking X-ray findings into consideration. The following is a guide to be used in the rehabilitation of a patient after a patella fracture, but it is always good to discuss treatment plans with the referring orthopaedic surgeons. | |||
=== Conservative management === | |||
Conservative management are used when the extensor mechanism is still intact.<ref name=":1" /> | |||
== | ==== Phase 1: 0-6 weeks ==== | ||
* Range of motion (as per surgeon): | |||
** Range of motion brace locked in extension 2-3 weeks | |||
** Controlled motion brace at 2-3 weeks | |||
** Exercises: | |||
*** Open kinetic chain strengthening and knee range of motion at 3-4 weeks - focus on active flexion & extension in inner ranges | |||
*** Quadriceps | |||
*** Hamstring | |||
*** Gluts sets | |||
*** SLR | |||
*** Open and closed kinetic chains hip strengthening exercises | |||
*** Circulatory drills | |||
* Weight-bearing: | |||
** Partial weight-bearing in brace | |||
** May stand tandem | |||
** Weight-bearing restrictions normally apply for 6-8 weeks<ref name=":11" /><ref name=":10" /> | |||
** Duration of crutches/weight-bearing restrictions as per surgeon | |||
* Patella mobilization | |||
* Pain & oedema management using [[cryotherapy]] | |||
<ref name=":1" /><ref name=":0" /> | |||
== | ==== Phase II: 6-12 weeks ==== | ||
* Range of motion knee brace as per surgeon | |||
* Range of motion: | |||
** Progress to full knee flexion & extension | |||
* Exercises: | |||
< | ** Stationary bike with seat elevated and no resistance | ||
< | ** Progress closed kinetic chain exercises: Mini squats, step up, retro step, etc | ||
** Progress resistance on hip exercises | |||
== References | ** Proprioception | ||
** Lunges from weeks 8-10 | |||
<ref name=":0" /> | |||
=== Post-operative rehabilitation === | |||
Surgical intervention are done in cases where there are significant displacement and the extensor mechanism is not intact. Open reduction and internal fixation using the tension band wire technique is normally the treatment of choice.<ref name=":1" /> | |||
==== Phase I: 0-2 weeks ==== | |||
* Range of motion brace: | |||
** Locked in extension (if POP cast not used) | |||
** Only to be taken off for physiotherapy sessions, 0-30° knee flexion range of motion allowed at first. | |||
* Mobilization: | |||
** Knee locked in extension with range of motion brace | |||
* Exercises: | |||
** Isometric quadriceps/hamstring/adductor/abductor strengthening | |||
** Resisted ankle exercises (e.g. with theraband) | |||
==== Phase II: 2-6 weeks ==== | |||
* Range of motion brace (if applicable): | |||
** To be worn for weight-bearing activities, locked in extension | |||
** May be removed at night | |||
* Range of motion: | |||
** 5° of flexion can be added each week to achieve 90° by week 6 | |||
* Exercises: | |||
** Isometric quadriceps/hamstring/adductor/abductor strengthening | |||
** Resisted ankle exercises (e.g. with theraband) | |||
** Initiate SLR | |||
==== Phase III: 6-10 weeks ==== | |||
* Range of motion brace: | |||
** Unlocked; to be worn for weight-bearing activities | |||
* Range of motion: | |||
** Progress to full range of motion by week 10 | |||
* Exercises: As previous phase | |||
==== Phase IV: 10-12 weeks ==== | |||
* Range of motion brace: Discontinue | |||
* Range of motion: Full | |||
* Exercises: As previous phase | |||
** Start with stationary cycling | |||
==== Phase V: Up to 3-6 months ==== | |||
Return to normal activities as tolerated. | |||
== References == | |||
<references /><span style="font-size: 13.28px; line-height: 1.5em;"> </span><span style="font-size: 13.28px; line-height: 1.5em;"> </span><span style="font-size: 13.28px; line-height: 1.5em;"> </span><span style="font-size: 13.28px; line-height: 1.5em;"> </span><br> | |||
< | <br> | ||
[[Category:Vrije_Universiteit_Brussel_Project | [[Category:Injury]] | ||
[[Category:Knee_Injuries]] | |||
[[Category:Knee]] | |||
[[Category:Conditions]] | |||
[[Category:Knee - Conditions]] | |||
[[Category:Musculoskeletal/Orthopaedics|Orthopaedics]] | |||
[[Category:Vrije_Universiteit_Brussel_Project]] | |||
[[Category:Primary Contact]] | |||
[[Category:Acute Care]] | |||
[[Category:Fractures]] | |||
Latest revision as of 00:06, 11 January 2023
Top Contributors - Marie Avau, Leana Louw, Lise De Wael, Admin, Angeliki Chorti, Rachael Lowe, Debby Decock, Patti Cavaleri, Kim Jackson, Aminat Abolade, Manisha Shrestha, 127.0.0.1, Evan Thomas, Scott Buxton, Oyemi Sillo, WikiSysop, Karen Wilson and Claire Knott
Definition/Description[edit | edit source]
Patella fractures are caused by direct trauma or compressive force, or as the indirect result of quadriceps contractions or excessive stress to the extensor mechanism.[1][2][3] Indirect injuries are commonly associated with tears of the retinaculum and quadriceps muscles.[1] Patella fractures make up about 1% of all skeletal injuries and are found in all age groups.[4][5][6]
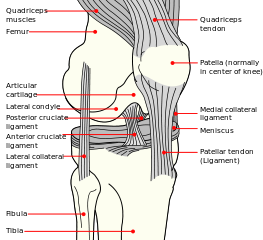
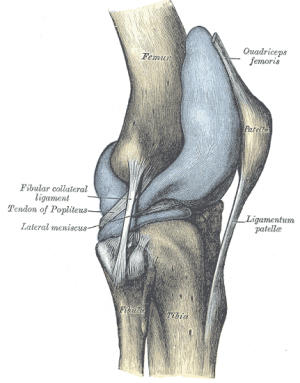
Clinically relevant anatomy[edit | edit source]
The patella is a triangular bone situated on the anterior surface of the knee at the distal end of the femur. It is the largest sesamoid bone in the body and makes part of the knee joint.[7][8][9] The patella 's primary role is to function as a fulcrum with the aim to increase the moment arm of the quadriceps muscle and thus, knee extensive capacity. [10]
Vastus medialis and lateralis, as part of the quadriceps group, control movement at the patella.[11] The medial retinaculum, formed by the vastus medialis and quadriceps aponeurosis and lateral retinaculum, formed by the vastus lateralis and the ilotibial band, all aid in the extension of the knee. [6]
The extensor mechanism as a whole plays a major role in patella fractures. The extensor mechanism consists of the quadriceps, quadriceps tendon, retinaculum, patella tendon, tibial tubercle and patellofemoral and patellotibial ligaments.[12] See the page on the patella for more details on the anatomy.
Epidemiology[edit | edit source]
A 2016 study found the incidence of patella fracture to be 13.1/100,000 per year with an increasing incidence with increasing age[13]. Females accounted for 56% of patella fractures and males accounted for 44% of patella fractures. [13] A newer Swedish study also found that older (>65 years old) females had a higher percentage of patellar fractures (64%) compared to males . [14] Most fractures were caused by low-energy trauma, with 70% due to simple falls, especially in the winter months. [14]
Patella fractures are not associated with an increased mortality rate, as the relative risk of death was 0.9.[15] In a recent study, the average mortality rate at one year after patella fractures was 2.8%, increasing to 6.2% in the geriatric population.
Complications[edit | edit source]
- Injuries (sprain/rupture) to ligaments and tendons attached to the patella
- Avascular necrosis[16]
- Post-traumatic arthritis
- Osteochondral damage to patellofemoral joint
- Stiffness
- Non-union
- Malunion
- Concomitant injuries (e.g. injuries to the acetabulum, femur and tibia)
- Long term complications:[17]
- Stiffness
- Extension weakness
- Patellofemoral arthritis.
Characteristics/Clinical Presentation[edit | edit source]
Types of fractures[edit | edit source]
Patella fractures are classified as either displaced or non-displaced. Displaced fractures are unstable and can be further classified as:[18]
- Comminuted: As a result of direct trauma (mostly due to blows or falls on flexed knee)
- Can cause damage to the articular cartilage of patella and femoral condyles.
- Transverse/stellate: As a result of muscle contraction/extensive stress on the extensor mechanism, e.g. explosive quadriceps contraction after jumping from height.
- Most common type[13]
- Proximal blood supply may be compromised
- Usually as a result of hyper-flexion of the knee
- Marginal: As a result of a fall on the knee
- Vertical/longitudinal
- Lower/upper pole
- Osteochondral
- Sleeve (only in paediatric patients)
The prognosis of the injury depends on the amount of chondral damage at the time of injury. Functional outcome depends on the ability to achieve pain-free and stable range of motion in an early stage. [20]
Differential diagnosis[edit | edit source]
- Bipartite patella[1]
- Knee dislocation
- Patella dislocation
Diagnosis[edit | edit source]
Interview[edit | edit source]
- Details regarding accident
- Mechanism of injury
- Pain at knee
- Complaints of difficulty standing or snapping sensation at knee
Physical examination[edit | edit source]
- Observation:
- Whole extremity
- Swollen, bruised knee
- Deformity around knee
- Possible wounds (open fracture)
- Palpation (often done after local anesthetics to eliminate pain):
- Tenderness around patella
- Palpable gap (for displaced fractures)
- Rule out concomitant injuries:
- e.g. fractures of the acetabulum, femur and tibia
- Haemarthrosis
- Range of motion:
- Acute:
- Limited knee and painful knee flexion and extension
- Often unable to do straight leg raise
- Chronic:
- Full knee flexion with extension lag
- Acute:
- Distal pulses
- Assess compartment of the leg
- Neurological assessment
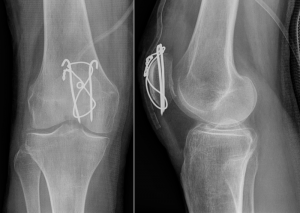
Special investigations[edit | edit source]
- AP view:
- May be difficult to see patella
- Lateral view:
- Undisplaced - < 2mm separation
- Displaced - > 2mm separation, step deformity noted
- Sky view
- Used for regular monitoring of healing process and any possible complications
- CT scan: Usually not needed
- MRI: Diagnosis of associated injuries to nearby tendons and ligaments
- Bone scans: To identify stress fractures
Outcome measures[edit | edit source]
- Knee injury and osteoarthritis outcome score
- Knee outcome survey
- Lower extremity function scale
- McGill pain questionnaire
Medical management[edit | edit source]
- In acute cases, local anesthetics can be given to eliminate pain.[21] This helps to aid in the assessment and diagnosis of the patella fracture.
Conservative management[edit | edit source]
Indication: Nondisplaced fracture (mostly vertical, horizontal and comminuted fractures) with extensor mechanism in place [1][20]
- Fracture immobilized with POP cylinder cast or range of motion brace locked in extension (4-6 weeks):
- As healing takes place, knee flexion can gradually be increased
- Range of motion brace must be worn until union (on X-rays) and clinical signs of healing (not tender on palpation) are present
- Crutch walking 6-8 weeks
- Rehabilitation to restore full range of motion, strength, and return to function
Surgical intervention[edit | edit source]
Indication: Significant displacement with extensor mechanism not intact[1]or articular step off >2-3mm or fracture displacement >1-4 mm. [6]
Aim: Restore extensor function, align articular incongruities, and allow early motion[20][23][26][27]
- Transverse/simple, comminuted mid-patella fracture: Open reduction and internal fixation using tension band wire technique using pins and wires and 'a figure of eight' to press the pieces together
- POP cast in extension for 6 weeks
- Proximal/distal <1/3 - simple or comminuted: Excision of small piece & tendon repair
- POP cast for 6 weeks
- Longitudinal (uncommon): Interfragmentary screw fixation
- Comminuted fracture/irreducible or irreparable fracture or when cartilage too badly damaged: Partial vs complete patellectomy:[21]
- Quadriceps muscles is is attached to the patellar ligament to ensure function of the extensor apparatus during a complete patellectomy[21]
- Patellectomy: Relatively old procedure, last treatment of choice due to significant loss of extension
- Repair of bilateral vastus muscles
- Rehabilitation same as with conservative management
Later stages:
Manipulation under anesthesia or the arthroscopic releasing of adhesions is required when athrofibrosis occurs.[20]
Physiotherapy management[edit | edit source]
As clinical healing phases do not always correlate with theoretical healing, the surgeon will guide rehabilitation while taking X-ray findings into consideration. The following is a guide to be used in the rehabilitation of a patient after a patella fracture, but it is always good to discuss treatment plans with the referring orthopaedic surgeons.
Conservative management[edit | edit source]
Conservative management are used when the extensor mechanism is still intact.[1]
Phase 1: 0-6 weeks[edit | edit source]
- Range of motion (as per surgeon):
- Range of motion brace locked in extension 2-3 weeks
- Controlled motion brace at 2-3 weeks
- Exercises:
- Open kinetic chain strengthening and knee range of motion at 3-4 weeks - focus on active flexion & extension in inner ranges
- Quadriceps
- Hamstring
- Gluts sets
- SLR
- Open and closed kinetic chains hip strengthening exercises
- Circulatory drills
- Weight-bearing:
- Patella mobilization
- Pain & oedema management using cryotherapy
Phase II: 6-12 weeks[edit | edit source]
- Range of motion knee brace as per surgeon
- Range of motion:
- Progress to full knee flexion & extension
- Exercises:
- Stationary bike with seat elevated and no resistance
- Progress closed kinetic chain exercises: Mini squats, step up, retro step, etc
- Progress resistance on hip exercises
- Proprioception
- Lunges from weeks 8-10
Post-operative rehabilitation[edit | edit source]
Surgical intervention are done in cases where there are significant displacement and the extensor mechanism is not intact. Open reduction and internal fixation using the tension band wire technique is normally the treatment of choice.[1]
Phase I: 0-2 weeks[edit | edit source]
- Range of motion brace:
- Locked in extension (if POP cast not used)
- Only to be taken off for physiotherapy sessions, 0-30° knee flexion range of motion allowed at first.
- Mobilization:
- Knee locked in extension with range of motion brace
- Exercises:
- Isometric quadriceps/hamstring/adductor/abductor strengthening
- Resisted ankle exercises (e.g. with theraband)
Phase II: 2-6 weeks[edit | edit source]
- Range of motion brace (if applicable):
- To be worn for weight-bearing activities, locked in extension
- May be removed at night
- Range of motion:
- 5° of flexion can be added each week to achieve 90° by week 6
- Exercises:
- Isometric quadriceps/hamstring/adductor/abductor strengthening
- Resisted ankle exercises (e.g. with theraband)
- Initiate SLR
Phase III: 6-10 weeks[edit | edit source]
- Range of motion brace:
- Unlocked; to be worn for weight-bearing activities
- Range of motion:
- Progress to full range of motion by week 10
- Exercises: As previous phase
Phase IV: 10-12 weeks[edit | edit source]
- Range of motion brace: Discontinue
- Range of motion: Full
- Exercises: As previous phase
- Start with stationary cycling
Phase V: Up to 3-6 months[edit | edit source]
Return to normal activities as tolerated.
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 1.8 1.9 Frobell R., Cooper R., Morris H., Arendt H. Acute knee injuries. In: Brukner P., Bahr R., Blair S., Cook J., Crossley K., McConnell J., McCrory P., Noakes T., Khan K. Clinical Sports Medicine: 4th edition. Sydney: McGraw-Hill. 2012; 626-683.
- ↑ 2.0 2.1 Schuett D., Hake M., Mauffrey C., Hammerberg E., Stahel P., Hak D. Current treatment strategies for patella fractures. Orthopedics. 2015;38(6):377-84.
- ↑ 3.0 3.1 Archdeacon M., Sanders R. Chapter 54 - Patella Fractures and Extensor Mechanism Injuries. In: Browner B.D., Jupiter J.B., Krettek C., Anderson P.A., (eds). Skeletal Trauma, 4th edition. Elsevier Health Sciences, 2008.
- ↑ Crowther M., Mandal A., Sarangi P. Propagation of stress fracture of the patella. British journal of sports medicine 2005;39(2):e6.
- ↑ Sweetnam R. Patellectomy. Postgraduate medical journal 1964 Sep;40(467):531.
- ↑ 6.0 6.1 6.2 Posner A., Zimmerman J. Surgical management of patella fractures: a review. Archives of Orthopaedics 2022; 3(1):17-21.
- ↑ Cedars-Sinai. Fractured Kneecap. Cedars Sinai organisation. https://www.cedars-sinai.org/health-library/diseases-and-conditions/f/fractured-kneecap.html (accessed 25/07/2018).
- ↑ Schunke M. Anatomische atlas Prometheus, algemene anatomie en bewegingsapparaat. Bohn Stafieu van Loghum: 2e druk. 2010.
- ↑ Everett L. Knee and Lower Leg. In: Marx J, Walls R, Hockberger R, editors. Rosen's Emergency Medicine: Concepts and Clinical Practice. 6th ed. Philadelphia: Mosby Elsevier, 2006.
- ↑ 10.0 10.1 Melvin S.J., Mehta S. Patellar fractures in adults. Journal of the American Academy of Orthopaedic Surgeons 2011;19(4):198-207.
- ↑ Orthopaedia. Collaborative Orthopaedic Knowledgebase, http://www.orthopaedia.com/display/Main/Patella+fractures (accessed November 10, 2010).
- ↑ 12.0 12.1 12.2 12.3 Duke Orthopaedics. Wheeless’ textbook of Orthopaedics. Fractures of the patella.http://www.wheelessonline.com/ortho/fractures_of_the_patella (accessed November 10 2010).
- ↑ 13.0 13.1 13.2 Larsen P., Court-Brown C., Vedel J., Vistrup S., Elsoe R. Incidence and Epidemiology of Patellar Fractures. Orthopedics; 2016 Nov 1;39(6):e1154-e1158.
- ↑ 14.0 14.1 Kruse M, Wolf O, Mukka S, Brüggemann A. Epidemiology, classification and treatment of patella fractures: an observational study of 3194 fractures from the Swedish Fracture Register. European Journal of Trauma and Emergency Surgery. 2022 May 30:1-8.
- ↑ Larsen P., Elsoe R. Patella fractures are not associated with an increased risk of mortality in elderly patients. Injury 2018; 49(10):1901-1904.
- ↑ 16.0 16.1 Medscape. Patella Fracture Imaging. http://emedicine.medscape.com/article/394270-overview> (accessed 25/07/2018).
- ↑ Insall JN. Fractured kneecap: treatments. Institute for Orthopaedics and sports medicine 2007.
- ↑ 18.0 18.1 Whittle P. Fractures of the Lower Extremity. In: Canale S., Beaty J., (eds). Campbell's Operative Orthopaedics. 11th ed. Philadelphia: Mosby Elsevier, 2008.
- ↑ 19.0 19.1 19.2 19.3 19.4 Walters J. (ed). Orthopaedics - A guide for practitioners. 4th Edition. Cape Town: University of Cape Town, 2010.
- ↑ 20.0 20.1 20.2 20.3 20.4 Mehling I., Mehling A., Rommens P. Comminuted patellar fractures. Current Orthopaedics 2006;20(6):397-404.
- ↑ 21.0 21.1 21.2 21.3 21.4 Günal I., Karatosun V. Patellectomy: an overview with reconstructive procedures. Clinical Orthopaedics and Related Research 2001;389:74-8.
- ↑ 22.0 22.1 McRae R., Esser M. Practical fracture treatment E-book. Churchill Livingstone/ Elsevier; 2002.
- ↑ 23.0 23.1 23.2 Fourati MK. Reeducation du genou après fracture de la rotule. Ann. Kinésitherapie 1986.
- ↑ Scolaro J, Bernstein J, Ahn J. In brief: patellar fractures. Clinical Orthopaedics and Related Research®. 2011 Apr;469(4):1213-5.
- ↑ 25.0 25.1 American Academy of Orthopaedic Surgeons. Diseases and conditions - Patellar (Kneecap) Fractures. http://orthoinfo.aaos.org/topic.cfm?topic=A00523 (accessed November 10 2010).
- ↑ Shang ZG. Patellar fractures treatment and management. Unbound medline 2013;26(6):445-8.
- ↑ 27.0 27.1 27.2 Strauss J. ORIF Patella Fracture Post-Operative Rehabilitation Protocol, Hospital for Joint Diseases, 2008.