Neuropathic Pain: Difference between revisions
No edit summary |
No edit summary |
||
| Line 6: | Line 6: | ||
== Definition == | == Definition == | ||
[[File:Painful.jpeg|right|frameless]] | [[File:Painful.jpeg|right|frameless]] | ||
The International Association for the Study of Pain (2011) defines neuropathic [[Pain Behaviours|pain]] as ‘pain caused by a lesion or disease of the [[Sensation|somatosensory]] nervous system’. | The International Association for the Study of Pain (2011) defines neuropathic [[Pain Behaviours|pain]] as ‘pain caused by a lesion or disease of the [[Sensation|somatosensory]] nervous system’. | ||
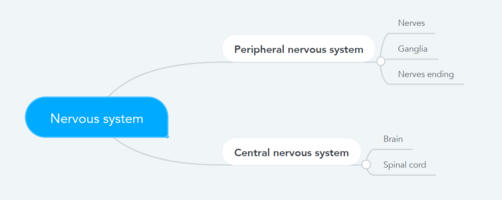
It can result from damage anywhere along the neuraxis: peripheral nervous system, spinal or supraspinal nervous system<ref name=":1">PPM [https://www.practicalpainmanagement.com/pain/neuropathic/pathophysiology-neuropathic-pain The Pathophysiology of Neuropathic Pain] Available:https://www.practicalpainmanagement.com/pain/neuropathic/pathophysiology-neuropathic-pain (accessed 30.10.2021)</ref>. | |||
# Central neuropathic pain is defined as ‘pain caused by a lesion or disease of the central somatosensory nervous system’. | # Central neuropathic pain is defined as ‘pain caused by a lesion or disease of the central somatosensory nervous system’. | ||
| Line 32: | Line 34: | ||
== Pathophysiology == | == Pathophysiology == | ||
The mechanism underlying neuropathic pain is not | Neuropathic pain is the result of disease or injury to the peripheral or central nervous system and the lesion may occur at any point. These damaged nerve fibers send incorrect signals to other pain centers. The impact of a nerve fiber injury includes a change in nerve function—both at the site of the injury and areas around the injury<ref name=":1" />. | ||
The mechanism underlying neuropathic pain is not clear. Several animal studies have shown that many mechanisms may be involved. | |||
* First order [[Neurone|neuron]]<nowiki/>s may increase their firing if they are partially damaged and increase the number of sodium channels. | * First order [[Neurone|neuron]]<nowiki/>s may increase their firing if they are partially damaged and increase the number of sodium channels. | ||
* Ectopic discharges are a result of enhanced depolarization at certain sites in the fiber, leading to spontaneous pain and movement-related pain. | * Ectopic discharges are a result of enhanced depolarization at certain sites in the fiber, leading to spontaneous pain and movement-related pain. | ||
* Inhibitory [[Interneurons|circuits]] may be impaired at the level of the dorsal horn or [[Brainstem|brain stem]] (or both) allowing pain impulses to travel unopposed. See [[Pain Facilitation and Inhibition]] | * Inhibitory [[Interneurons|circuits]] may be impaired at the level of the dorsal horn or [[Brainstem|brain stem]] (or both) allowing pain impulses to travel unopposed. See [[Pain Facilitation and Inhibition]] | ||
* In addition, there may be alterations in the central processing of pain when (due to [[Chronic Pain and the Brain|chronic pain]] and use of some drugs), second- and third-order neurons may develop a “memory” of pain and become sensitized. | * In addition, there may be alterations in the central processing of pain when (due to [[Chronic Pain and the Brain|chronic pain]] and use of some drugs), second- and third-order neurons may develop a “memory” of pain and become sensitized. There is then heightened sensitivity of spinal neurons and reduced activation thresholds. <ref name=":0" /> | ||
See also Mechanisms of peripheral neuropathic pain: implications for musculoskeletal physiotherapy https://www.physio-pedia.com/images/d/db/NeuropathicPain.hysio.pdf?utm_source=physiopedia&utm_medium=search&utm_campaign=ongoing_internal | |||
See also Mechanisms of peripheral neuropathic pain: implications for musculoskeletal physiotherapy https://www.physio-pedia.com/images/d/db/NeuropathicPain.hysio.pdf?utm_source=physiopedia&utm_medium=search&utm_campaign=ongoing_internal | |||
== Clinical Features == | == Clinical Features == | ||
Traits that differentiate neuropathic pain from other types of pain include pain and sensory symptoms lasting beyond the healing period. It is characterized in humans by spontaneous pain, allodynia (the experience of non-noxious stimuli as painful), and causalgia (constant burning pain). | |||
* Spontaneous pain includes sensations of ‘pins and needles,’ shooting, burning, stabbing and paroxysmal pain (electric-shock like) often associated with dysesthesias and paresthesias. These sensations not only affect the patient’s sensory system, but also the patient’s well-being, mood, focus and thinking. | |||
* Neuropathic pain consists of both “negative” symptoms (sensory loss and numbness) and “positive” symptoms (paresthesias, spontaneous pain, increased sensation of pain)<ref name=":1" />. | |||
* The onset of pain may be delayed, the commonest example being central poststroke pain ([[Thalamus|thalamic]]), which may start months or years after the initiating stroke. | |||
* Pain is often of mixed [[Nociception|nociceptive]] and neuropathic types, eg mechanical spinal pain with [[radiculopathy]] or [[myelopathy]]. | |||
== Assessment == | == Assessment == | ||
One of the challenges, in regards to neuropathic pain, is the ability to assess it. There is a dual component to this: assessing quality, intensity and improvement; and accurately diagnosing neuropathic pain. | |||
There are, however, some diagnostic tools that may assist clinicians in evaluating neuropathic pain. eg nerve conduction studies and sensory-evoked potentials can identify and quantify the extent of damage to sensory, but not nociceptive, pathways by monitoring neurophysiological responses to electrical stimuli. | |||
Mechanical sensitivity to tactile stimuli is measured with von Frey hairs, pinprick with weighted needles, vibration sensitivity with vibrameters and thermal pain with thermodes. | |||
It is also very important to perform a thorough neurological evaluation to identify motor, sensory and autonomic dysfunctions. Finally, there are numerous questionnaires used to distinguish neuropathic pain from nociceptive pain<ref name=":1" />.e.g., the Neuropathic Questionnaire11 and ID Pain. | |||
== Management == | |||
[[File:Neuro-HTtens-300x200.jpg|alt=|right|frameless]]Neuropathic pain often responds poorly to standard pain treatments and occasionally may get worse instead of better over time. For some people, it can lead to serious disability. A multidisciplinary approach that combines therapies, however, can be a very effective way to provide relief from neuropathic pain.<ref name="p2" /> Other kinds of treatments can also help with neuropathic pain including: Physical therapy; Counselling; Relaxation therapy; [[Massage|Massage therapy]]; [[Acupuncture]] | |||
A number of pharmacological treatments can be used to manage neuropathic pain outside of specialist pain management services. However, there is considerable variation in how treatment is initiated, the dosages used and the order in which drugs are introduced, whether therapeutic doses are achieved and whether there is correct sequencing of therapeutic classes. | |||
A further issue is that a number of commonly used treatments are unlicensed for treating neuropathic pain, which may limit their use. These factors may lead to inadequate pain control, with considerable morbidity. | |||
Commonly used pharmacological treatments include antidepressants (tricyclic antidepressants, selective serotonin reuptake inhibitors [SSRIs] and serotonin–norepinephrine reuptake inhibitors [SNRIs]), antiepileptic (anticonvulsant) drugs, topical treatments and opioid analgesics. In addition to their potential benefits, all of these drug classes are associated with various adverse effects<ref name=":0" />. | |||
Effective management of the condition can also help prevent further nerve damage<ref>http://www.webmd.com/pain-management/guide/neuropathic-pain</ref>. | |||
In cases that are difficult to treat, a pain specialist may use an invasive or implantable device to effectively manage the pain. Electrical stimulation of the nerves involved in neuropathic pain may significantly control the pain symptoms.<ref name="p2">http://www.webmd.com/pain-management/guide/neuropathic-pain</ref> | |||
=== Physical therapy management | === Physical therapy management === | ||
[[File:Mirror therapy.jpg|right|frameless]] | [[File:Mirror therapy.jpg|right|frameless]] | ||
Physical therapy, exercise and movement representation techniques (that is, treatments such as mirror therapy and motor imagery that use the observation and/or imagination of normal pain-free movements) have been suggested to be beneficial in neuropathic pain management. eg [[Mirror Therapy|mirror therapy]] and motor imagery are effective in the treatment of pain and disability associated with [[Complex Regional Pain Syndrome (CRPS)|complex regional pain syndrome]] type I and type II. The quality of evidence supporting these interventions for neuropathic pain is weak and needs further investigation | Physical therapy, exercise and movement representation techniques (that is, treatments such as mirror therapy and motor imagery that use the observation and/or imagination of normal pain-free movements) have been suggested to be beneficial in neuropathic pain management. eg [[Mirror Therapy|mirror therapy]] and motor imagery are effective in the treatment of pain and disability associated with [[Complex Regional Pain Syndrome (CRPS)|complex regional pain syndrome]] type I and type II. The quality of evidence supporting these interventions for neuropathic pain is weak and needs further investigation | ||
[[Transcutaneous Electrical Nerve Stimulation (TENS)|TENS]] is effective in the treatment of painful peripheral neuropathy, and very low level laser therapy has been shown to be effective in patients with neuropathic pain<ref name="p7" />. | [[Transcutaneous Electrical Nerve Stimulation (TENS)|TENS]] is effective in the treatment of painful peripheral neuropathy, and very low level laser therapy has been shown to be effective in patients with neuropathic pain<ref name="p7">http://www.omicsonline.org/physical-therapy-modalities-and-rehabilitation-techniques-in-the-treatment-of-neuropathic-pain-jpmr.1000124.pdf</ref>. | ||
[[File:Laserfornp.jpg|alt=|right|frameless|300x300px]] | [[File:Laserfornp.jpg|alt=|right|frameless|300x300px]] | ||
Neurostimulation techniques including transcranial magnetic stimulation (TMS) and cortical electrical stimulation (CES), spinal cord stimulation (SCS) and deep brain stimulation (DBS) have also been found effective in the treatment of neuropathic pain. | Neurostimulation techniques including transcranial magnetic stimulation (TMS) and cortical electrical stimulation (CES), spinal cord stimulation (SCS) and [[Deep Brain Stimulation|deep brain stimulation]] (DBS) have also been found effective in the treatment of neuropathic pain. | ||
[[Therapeutic Exercise|Exercise]]: exercising for just 30 minutes a day on at least three or four days a week will help you with chronic pain management by increasing:<ref name="p0" />[[Muscle Strength Testing|Muscle Strength]]; Endurance; Stability in the joints; Flexibility in the muscles and joints<br>Keeping a consistent exercise routine will also help control pain. Regular therapeutic exercise will help you maintain the ability to move and function physically, rather than becoming disabled by your chronic pain. There are studies showing that exercise may be an important part of the treatment and prevention of neuropathic pain after chemotherapy. Although more information is required and detailed exercise prescriptions do not yet exist for patients receiving cancer treatment.<ref>Majithia N, Loprinzi CL, Smith TJ.[https://pubmed.ncbi.nlm.nih.gov/27854104/ New Practical Approaches to Chemotherapy-Induced Neuropathic Pain: Prevention, Assessment, and Treatment.] Oncology (Williston Park). 2016 Nov 15;30(11)</ref> It has been also found that physical exercise, such as forced treadmill running and swimming, can sufficiently improve mechanical allodynia and heat hyperalgesia in animal models of neuropathic pain. <ref>Kami K, Tajima F, Senba E. [https://pubmed.ncbi.nlm.nih.gov/27484434/#:~:text=Physical%20exercise%2C%20such%20as%20forced,and%20spinal%20nerve%20ligation%20models. Exercise-induced hypoalgesia: potential mechanisms in animal models of neuropathic pain.] Anat Sci Int. 2016 Aug 2. [Epub ahead of print]</ref> | |||
< | Physical therapy tackles the physical side of the [[Inflammation Acute and Chronic|inflammation]], stiffness, and soreness with exercise, manipulation, and [[massage]], but it also works to help the body heal itself by encouraging the production of the body's natural pain-relieving chemicals. This two-pronged approach is what helps make physical therapy so effective as a pain treatment.<ref name="p0">[https://www.everydayhealth.com/pain-management/physical-activity-and-therapy.aspx Physical Therapy for Pain Management].By Diana Rodriguez | Medically reviewed by Pat F. Bass III, MD, MPH</ref> {{#ev:youtube|hDu_WdRNDzo}}<ref>Victoria Pain Specialists. Neuropathic Pain.</ref> | ||
== References == | == References == | ||
Revision as of 06:46, 30 October 2021
Original Editor - Kerstin McPherson
Top Contributors - Andeela Hafeez, Melissa Coetsee, Kerstin McPherson, Vanessa Rhule, Riccardo Ugrin, Lucinda hampton, Kim Jackson, Admin, Evan Thomas, Chrysolite Jyothi Kommu, WikiSysop, Vidya Acharya, Kapil Narale, Temitope Olowoyeye, Jo Etherton, Lauren Lopez, Amanda Ager, 127.0.0.1, Wendy Walker, Carina Therese Magtibay and Oyemi Sillo
Definition[edit | edit source]
The International Association for the Study of Pain (2011) defines neuropathic pain as ‘pain caused by a lesion or disease of the somatosensory nervous system’.
It can result from damage anywhere along the neuraxis: peripheral nervous system, spinal or supraspinal nervous system[1].
- Central neuropathic pain is defined as ‘pain caused by a lesion or disease of the central somatosensory nervous system’.
- Peripheral neuropathic pain is defined as ‘pain caused by a lesion or disease of the peripheral somatosensory nervous system’.
Neuropathic pain is very challenging to manage because of the heterogeneity of its aetiologies, symptoms and underlying mechanisms[2].
Causes[edit | edit source]
Conditions frequently associated with neuropathic pain can be categorized into two major group, pain due to damage in the central nervous system and pain due to damage to the peripheral nervous system.
Central nervous system causes include:
- Cortical and sub-cortical strokes, traumatic spinal cord injuries, syringomyelia and syringobulbia, trigeminal and glossopharyngeal neuralgias, neoplastic and other space-occupying lesions.
Peripheral nervous system causes include:
- Nerve compression/ entrapment neuropathies (eg carpal tunnel syndrome, thoracic outlet syndrome or piriformis syndrome [3]) , ischemic neuropathy,
- post traumatic neuropathy (occurs after injury or medical procedures, such as surgery or injection)[3]
- nerve root compression,
- post-amputation stump and phantom limb pain (the exact cause of phantom limb pain is unknown, it appears to result when the nerves and the brain send faulty signals to the limb as the circuitry attempts to "rewire" itself[3]),
- postherpetic neuralgia (can occur following a viral infection of herpes zoster "shingles" in the nervous system)[3] and cancer-related neuropathies.
Following a peripheral origin, central sensitization may develop as a result of ectopic neuronal activity in the spinal cord dorsal horn, implying a potential autonomous pain-generating mechanism.[4]
Pathophysiology[edit | edit source]
Neuropathic pain is the result of disease or injury to the peripheral or central nervous system and the lesion may occur at any point. These damaged nerve fibers send incorrect signals to other pain centers. The impact of a nerve fiber injury includes a change in nerve function—both at the site of the injury and areas around the injury[1].
The mechanism underlying neuropathic pain is not clear. Several animal studies have shown that many mechanisms may be involved.
- First order neurons may increase their firing if they are partially damaged and increase the number of sodium channels.
- Ectopic discharges are a result of enhanced depolarization at certain sites in the fiber, leading to spontaneous pain and movement-related pain.
- Inhibitory circuits may be impaired at the level of the dorsal horn or brain stem (or both) allowing pain impulses to travel unopposed. See Pain Facilitation and Inhibition
- In addition, there may be alterations in the central processing of pain when (due to chronic pain and use of some drugs), second- and third-order neurons may develop a “memory” of pain and become sensitized. There is then heightened sensitivity of spinal neurons and reduced activation thresholds. [2]
See also Mechanisms of peripheral neuropathic pain: implications for musculoskeletal physiotherapy https://www.physio-pedia.com/images/d/db/NeuropathicPain.hysio.pdf?utm_source=physiopedia&utm_medium=search&utm_campaign=ongoing_internal
Clinical Features[edit | edit source]
Traits that differentiate neuropathic pain from other types of pain include pain and sensory symptoms lasting beyond the healing period. It is characterized in humans by spontaneous pain, allodynia (the experience of non-noxious stimuli as painful), and causalgia (constant burning pain).
- Spontaneous pain includes sensations of ‘pins and needles,’ shooting, burning, stabbing and paroxysmal pain (electric-shock like) often associated with dysesthesias and paresthesias. These sensations not only affect the patient’s sensory system, but also the patient’s well-being, mood, focus and thinking.
- Neuropathic pain consists of both “negative” symptoms (sensory loss and numbness) and “positive” symptoms (paresthesias, spontaneous pain, increased sensation of pain)[1].
- The onset of pain may be delayed, the commonest example being central poststroke pain (thalamic), which may start months or years after the initiating stroke.
- Pain is often of mixed nociceptive and neuropathic types, eg mechanical spinal pain with radiculopathy or myelopathy.
Assessment[edit | edit source]
One of the challenges, in regards to neuropathic pain, is the ability to assess it. There is a dual component to this: assessing quality, intensity and improvement; and accurately diagnosing neuropathic pain.
There are, however, some diagnostic tools that may assist clinicians in evaluating neuropathic pain. eg nerve conduction studies and sensory-evoked potentials can identify and quantify the extent of damage to sensory, but not nociceptive, pathways by monitoring neurophysiological responses to electrical stimuli.
Mechanical sensitivity to tactile stimuli is measured with von Frey hairs, pinprick with weighted needles, vibration sensitivity with vibrameters and thermal pain with thermodes.
It is also very important to perform a thorough neurological evaluation to identify motor, sensory and autonomic dysfunctions. Finally, there are numerous questionnaires used to distinguish neuropathic pain from nociceptive pain[1].e.g., the Neuropathic Questionnaire11 and ID Pain.
Management[edit | edit source]
Neuropathic pain often responds poorly to standard pain treatments and occasionally may get worse instead of better over time. For some people, it can lead to serious disability. A multidisciplinary approach that combines therapies, however, can be a very effective way to provide relief from neuropathic pain.[5] Other kinds of treatments can also help with neuropathic pain including: Physical therapy; Counselling; Relaxation therapy; Massage therapy; Acupuncture
A number of pharmacological treatments can be used to manage neuropathic pain outside of specialist pain management services. However, there is considerable variation in how treatment is initiated, the dosages used and the order in which drugs are introduced, whether therapeutic doses are achieved and whether there is correct sequencing of therapeutic classes.
A further issue is that a number of commonly used treatments are unlicensed for treating neuropathic pain, which may limit their use. These factors may lead to inadequate pain control, with considerable morbidity.
Commonly used pharmacological treatments include antidepressants (tricyclic antidepressants, selective serotonin reuptake inhibitors [SSRIs] and serotonin–norepinephrine reuptake inhibitors [SNRIs]), antiepileptic (anticonvulsant) drugs, topical treatments and opioid analgesics. In addition to their potential benefits, all of these drug classes are associated with various adverse effects[2].
Effective management of the condition can also help prevent further nerve damage[6].
In cases that are difficult to treat, a pain specialist may use an invasive or implantable device to effectively manage the pain. Electrical stimulation of the nerves involved in neuropathic pain may significantly control the pain symptoms.[5]
Physical therapy management[edit | edit source]
Physical therapy, exercise and movement representation techniques (that is, treatments such as mirror therapy and motor imagery that use the observation and/or imagination of normal pain-free movements) have been suggested to be beneficial in neuropathic pain management. eg mirror therapy and motor imagery are effective in the treatment of pain and disability associated with complex regional pain syndrome type I and type II. The quality of evidence supporting these interventions for neuropathic pain is weak and needs further investigation
TENS is effective in the treatment of painful peripheral neuropathy, and very low level laser therapy has been shown to be effective in patients with neuropathic pain[7].
Neurostimulation techniques including transcranial magnetic stimulation (TMS) and cortical electrical stimulation (CES), spinal cord stimulation (SCS) and deep brain stimulation (DBS) have also been found effective in the treatment of neuropathic pain.
Exercise: exercising for just 30 minutes a day on at least three or four days a week will help you with chronic pain management by increasing:[8]Muscle Strength; Endurance; Stability in the joints; Flexibility in the muscles and joints
Keeping a consistent exercise routine will also help control pain. Regular therapeutic exercise will help you maintain the ability to move and function physically, rather than becoming disabled by your chronic pain. There are studies showing that exercise may be an important part of the treatment and prevention of neuropathic pain after chemotherapy. Although more information is required and detailed exercise prescriptions do not yet exist for patients receiving cancer treatment.[9] It has been also found that physical exercise, such as forced treadmill running and swimming, can sufficiently improve mechanical allodynia and heat hyperalgesia in animal models of neuropathic pain. [10]
Physical therapy tackles the physical side of the inflammation, stiffness, and soreness with exercise, manipulation, and massage, but it also works to help the body heal itself by encouraging the production of the body's natural pain-relieving chemicals. This two-pronged approach is what helps make physical therapy so effective as a pain treatment.[8]
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 PPM The Pathophysiology of Neuropathic Pain Available:https://www.practicalpainmanagement.com/pain/neuropathic/pathophysiology-neuropathic-pain (accessed 30.10.2021)
- ↑ 2.0 2.1 2.2 NICE. Neuropathic pain in adults: pharmacological management in non-specialist settings.Available: https://www.ncbi.nlm.nih.gov/books/NBK552848/(accessed 30.9.2021)
- ↑ 3.0 3.1 3.2 3.3 Neuropathy-Nerve pain-Dr. Mary Car-Blanchard, OTD/OTR/L and the following editorial advisors: Steve Meadows, MD, Ernie F. Soto, DDS, Ronald J. Glatzer, MD, Jonathan Rosenberg, MD, Christopher M. Nolte, MD, David Ap
- ↑ Haroutounian S, Nikolajsen L, Bendtsen TF, Finnerup NB, Kristensen AD, Hasselstrøm JB, Jensen TS (2014). Primary afferent input critical for maintaining spontaneous pain in peripheral neuropathy. Pain, 155 (7), 1272-9
- ↑ 5.0 5.1 http://www.webmd.com/pain-management/guide/neuropathic-pain
- ↑ http://www.webmd.com/pain-management/guide/neuropathic-pain
- ↑ http://www.omicsonline.org/physical-therapy-modalities-and-rehabilitation-techniques-in-the-treatment-of-neuropathic-pain-jpmr.1000124.pdf
- ↑ 8.0 8.1 Physical Therapy for Pain Management.By Diana Rodriguez | Medically reviewed by Pat F. Bass III, MD, MPH
- ↑ Majithia N, Loprinzi CL, Smith TJ.New Practical Approaches to Chemotherapy-Induced Neuropathic Pain: Prevention, Assessment, and Treatment. Oncology (Williston Park). 2016 Nov 15;30(11)
- ↑ Kami K, Tajima F, Senba E. Exercise-induced hypoalgesia: potential mechanisms in animal models of neuropathic pain. Anat Sci Int. 2016 Aug 2. [Epub ahead of print]
- ↑ Victoria Pain Specialists. Neuropathic Pain.