Yoga and mindfulness for pelvic health
This article is currently under review and may not be up to date. Please come back soon to see the finished work! (25/06/2019)
Definitions[edit | edit source]
Yoga:
"A Hindu spiritual and ascetic discipline, a part of which, including breath control, simple meditation, and the adoption of specific bodily postures, is widely practised for health and relaxation." [1]
Mindfulness:
"Mindfulness is the basic human ability to be fully present, aware of where we are and what we’re doing, and not overly reactive or overwhelmed by what’s going on around us." [2]
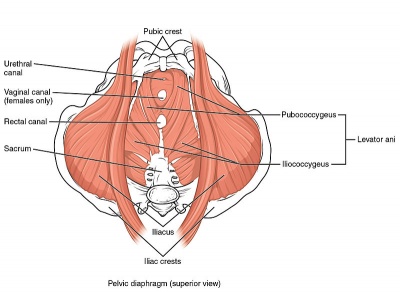
Clinically Relevant Anatomy[edit | edit source]
Please see the page "Pelvic Floor Anatomy," for further details regarding anatomy.
Roles of the Pelvic Floor[edit | edit source]
Yoga and mindfulness training[edit | edit source]
Yoga has been suggested to be useful in managing a range of medical conditions, including musculoskeletal conditions, cardiovascular conditions, stress, depression, and anxiety.[3] Yoga may function as either an alternative method of pelvic floor muscle training or a supplement to such training. Yoga may also address mental health and quality of life issues, through potential effects on depression, stress, and anxiety, and help patients manage their medical condition.[4]
Physiotherapists with knowledge of the pelvic floor can successfully integrate yoga practices into their therapy to improve various pelvic health issues.
Urinary Incontinence
Urinary incontinence is usually initially managed by conservative therapies. Many reviews of these conservative interventions, such as lifestyle advice, bladder training, and pelvic floor muscle training used either alone or in combination with other active treatments such as biofeedback.[5][6][7] Additionally studies have found that yoga can improve urinary incontinence symptoms.[8][9][10]
A randomized trial of ambulatory women aged 40 years and older, studied the effects of Iyengar yoga, a form of Hatha yoga on urinary incontinence. On average, 85% decrease in stress incontinence frequency compared to a 25% increase in controls, however, no significant differences in reduction in urgency incontinence. Specific yoga poses that are believed to be helpful include the Utkatasana (chair pose), Trikonasana (triangle pose), and the Malasana (squat pose).[9]
Another randomized trial assessed the feasibility of a group-based therapeutic yoga program for ambulatory middle-aged and older women with incontinence. All participants were provided with written, evidence-based information about behavioral incontinence self-management techniques (pelvic floor exercises, bladder training), the yoga group was provided with additional Iyengar-based yoga techniques. Over 3 months, total incontinence frequency decreased by an average of 76% from baseline in the yoga and 56% in the control group (P = .07 for between-group difference). Stress incontinence frequency also decreased by an average of 61% in the yoga group and 35% in controls (P = .045 for between-group difference), but changes in urgency incontinence frequency did not differ significantly between groups.[10]
Yoga may help improve general body alignment, flexibility, strength, control, and awareness, all of which are thought to assist in strengthening the pelvic floor muscles.[3] Yoga may therefore function as either an alternative method of pelvic floor muscle training or a supplement to such training.
Interstitial Cystitis/Bladder Pain Syndrome
Mindfulness-based stress reduction (MBSR) is a standardized meditation program that may be an effective therapy for Interstitial Cystitis/Bladder Pain Syndrome (IC/BPS). A randomized control trial recruited women who were undergoing first and second line treatments and assessed the addition of an 8-week MBSR class. First line treatments include relaxation/stress management, pain management and self-care/behavioral modification, and the second line therapy involves physical therapy, as well as oral or intravesical medications.[11]
Pelvic Organ Prolapse
Sweta et al. (2018) studied the effect of three months of Mulabandha yoga for females with symptomatic mild pelvic organ prolapse. Participants found a significant improvement in chief complaints like perennial pain, P/V discharge, perineal muscle laxity and feeling of "something coming out."[12]
Chronic Pelvic Pain
Chronic pelvic pain can be challenging to manage due to the multifactorial and heterogeneous nature of this issue.
When taught in a way that emphasizes awareness and control over individual muscle groups, yoga can be used to help women identify and stretch their pelvic floor muscles in order to improve pelvic pain associated with pelvic floor hypertonicity. Yoga techniques that promote deep breathing and relaxation can also reduce anxiety and perceived stress as well as influence autonomic nervous system balance as potential modulators of chronic pelvic pain.[13]
A study conducted by Huang et al. (2017) examined the effect of Iyengar-based yoga techniques on pain severity, sexual function, and well-being of women. Women demonstrated improvements in scores on IPP subscales for daily activities, emotional well-being, and sexual function
Yoga has been examined for chronic pelvic pain with women with endometriosis and it resulted in significantly lower pain and improved quality of life.[14]
Dysmenorrhea
Irritable Bowel Syndrome
Kuttner et al. examined the effect of yoga for adolescents with irritable bowel syndrome and its affect on assessing gastrointestinal symptoms, pain, functional disability, coping, anxiety and depression. The yoga intervention consisted of a 1 h instructional session, demonstration and practice, followed by four weeks of daily home practice guided by a video.[15]
Resources[edit | edit source]
References[edit | edit source]
- ↑ Oxford dictionaries. Available from:https://en.oxforddictionaries.com/definition/yoga
- ↑ Mindful. Available from: https://www.mindful.org/what-is-mindfulness/
- ↑ 3.0 3.1 Tenfelde S, Logan R, Abernethy M. Yoga for the Pelvic Floor. Beginnings. 2014;34(1).
- ↑ Shrestha N, Lassi ZS, Panda S, Chiaramonte D, Skoetz N, Wieland LS. Yoga for treatment of urinary incontinence in women. The Cochrane database of systematic reviews. 2017 May;2017(5).
- ↑ Ayeleke RO, Hay‐Smith EJ, Omar MI. Pelvic floor muscle training added to another active treatment versus the same active treatment alone for urinary incontinence in women. Cochrane Database of Systematic Reviews. 2013(11).
- ↑ Dumoulin C, Hay‐Smith EJ, Mac Habée‐Séguin G. Pelvic floor muscle training versus no treatment, or inactive control treatments, for urinary incontinence in women. Cochrane database of systematic reviews. 2014(5).
- ↑ Wallace SA, Roe B, Williams K, Palmer M. Bladder training for urinary incontinence in adults. Cochrane Database of systematic reviews. 2004(1).
- ↑ Kim GS, Kim EG, Shin KY, Choo HJ, Kim MJ. Combined pelvic muscle exercise and yoga program for urinary incontinence in middle‐aged women. Japan Journal of Nursing Science. 2015 Oct;12(4):330-9.
- ↑ 9.0 9.1 Huang AJ, Jenny HE, Chesney MA, Schembri M, Subak LL. A group-based yoga therapy intervention for urinary incontinence in women: a pilot randomized trial. Female pelvic medicine & reconstructive surgery. 2014 May;20(3):147.
- ↑ 10.0 10.1 Huang AJ, Chesney M, Lisha N, Vittinghoff E, Schembri M, Pawlowsky S, Hsu A, Subak L. A group-based yoga program for urinary incontinence in ambulatory women: feasibility, tolerability, and change in incontinence frequency over 3 months in a single-center randomized trial. American journal of obstetrics and gynecology. 2019 Jan 1;220(1):87-e1.
- ↑ Kanter G, Komesu YM, Qaedan F, Jeppson PC, Dunivan GC, Cichowski SB, Rogers RG. Mindfulness-based stress reduction as a novel treatment for interstitial cystitis/bladder pain syndrome: a randomized controlled trial. International urogynecology journal. 2016 Nov 1;27(11):1705-11.
- ↑ Sweta KM, Godbole A, Awasthi HH, Pandey U. Effect of mula bandha yoga in mild grade pelvic organ prolapse: A randomized controlled trial. International journal of yoga. 2018 May;11(2):116.
- ↑ Huang AJ, Rowen TS, Abercrombie P, Subak LL, Schembri M, Plaut T, Chao MT. Development and Feasibility of a Group-Based Therapeutic Yoga Program for Women with Chronic Pelvic Pain. Pain Medicine. 2017 Apr 15;18(10):1864-72.
- ↑ Gonçalves AV, Barros NF, Bahamondes L. The practice of hatha yoga for the treatment of pain associated with endometriosis. The journal of alternative and complementary medicine. 2017 Jan 1;23(1):45-52.
- ↑ Kuttner L, Chambers CT, Hardial J, Israel DM, Jacobson K, Evans K. A randomized trial of yoga for adolescents with irritable bowel syndrome. Pain Research and Management. 2006;11(4):217-24.