Whiplash Associated Disorders
Original Editor - Hannah Norton
Top Contributors - Kim Jackson, Rachael Lowe, Okebanama Nelson Onyebuchi, Lucinda hampton, Tarina van der Stockt, Admin, Hannah Norton, Van Horebeek Erika, Sigrid Bortels, Anouck Leo, WikiSysop, Steffen Kistmacher, Joshua Samuel, Ine Van de Weghe, Simisola Ajeyalemi, Rucha Gadgil, 127.0.0.1, Wanda van Niekerk, Jess Bell, Olajumoke Ogunleye and Robin Tacchetti
Clinically Relevant Anatomy
[edit | edit source]
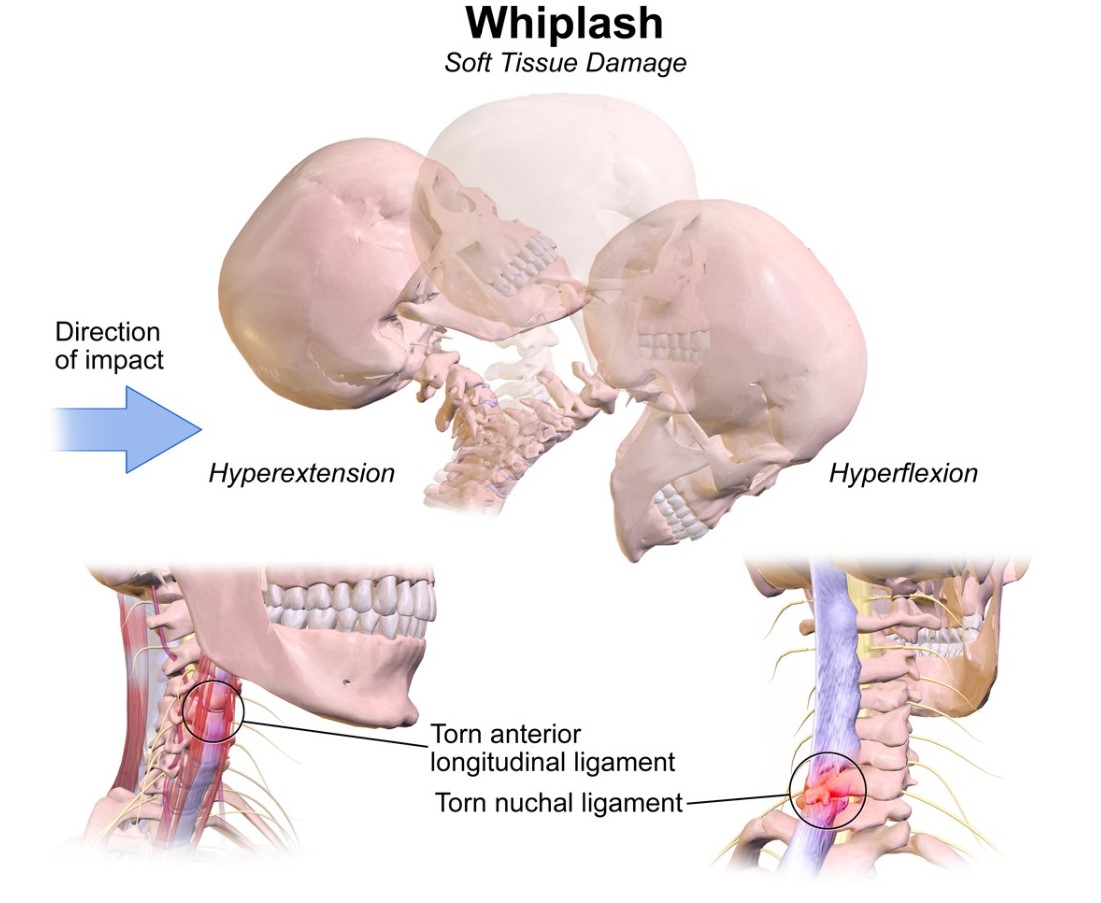
Whiplash and whiplash associated disorders (WAD) affects variable areas of the cervical spine, depending on the force and direction of impact as well as many other factors. In a whiplash injury, bony structures, ligamentous structures, muscles, neurological structures, and other connective tissue may be affected. Anatomic causes of pain can be any of these structures, with the strain injury resulting in secondary edema, hemorrhage, and inflammation.
Mechanism of Injury / Pathological Process
[edit | edit source]
The mechanism of injury is variable, usually involving a motor vehicle accident but also including causes such as sports injury, child abuse, blows to the head from a falling object, or similar accelleration-decceleration event.
Clinical Presentation[edit | edit source]
The most common presentation will be sub-occipital headaches and/or neck pain that is constant or motion-induced. There may be up to 48 hrs delay of symptom onset from the initial injury. Other signs include neurologic signs, dizziness, tinnitus, visual disturbances, UE radicular pain, difficulty sleeping due to pain, and difficulty concentrating/poor memory. (eMedicine) It is important to provide a thorough spinal exam and neurologic exam in patient with WAD to screen for delayed-onset of cervical spine instability or myelopathy. [1]
QTFC (Quebec Task Force Classification)
[edit | edit source]
The Quebec Task Force was a task force sponsored by a public insurer in Canada. They submitted recommendations regarding classification and treatment of WAD, which was used to develop a guide for managing whiplash in 1995. An updated report was published in 2001. Each of the grades corresponds to a specific treatment recommendation.
| QTFC Grade |
Clinical presentation |
| 0 |
No complaint about neck pain No physical signs |
| I |
Nec complaints of pain, stiffness or tenderness only No physical signs |
| II |
Neck complaint Musculoskeletal signs including
|
| III |
Neck complaint Musculosceletal signs Neurological signs including:
|
| IV |
Neck complaint and fracture or dislocation |
MQTFC (Modified Quebec Task Force Classification) [2]
|
Proposed classification grade |
Physical and psychological impairments present |
| WAD 0 |
No complaints about neck pain No physical signs |
| WAD I |
No complaints of pain, stiffness or tenderness only No physical signs |
| WAD IIA |
Neck complaint Motor impairment
Sensory Impairment
|
| WAD IIB |
Neck complaint Motor impairment
Sensory Impairment
Psychological impairment
|
| WAD IIC |
Neck complaint
Motor impairment
Sensory Impairment
Psychological impairment
|
| WAD III |
Neck complaint Motor impairment
Sensory Impairment
Neurological signs of conduction loss including:
Psychological impairment
|
| WAD IV |
Fracture or dislocation |
Diagnostic Procedures[edit | edit source]
Canadian C-Spine Rule (CCR): algorithm to determine the necessity for cervical spine radiography in alert and stable patients presenting with trauma and cervical spine injury. [3]
Management / Interventions
[edit | edit source]
Management approaches for patients with WAD are poorly researched. These patients often do not fit into treatment categories as defined for other cervical pain problems due to multiple factors, and even within the WAD group there are multiple variances which warrant individualized treatment approaches. The most recent evidence supports the use of Sterling's classification system for WAD. [4]
ACUTE WHPLASH
[edit | edit source]
Whiplash – associated disorder (WAD) is a debilitating and costly condition of at least 6-month duration. Although the majority of patients with whiplash show no physical signs [5] studies have shown that as many as 50% of victims of whiplash injury (grade 1 or 2 WAD) will still be experiencing chronic neck pain and disability six months later [6]. In most cases, symptoms are short lived, but a substantial minority go on to develop LWS (late whiplash syndrome), i.e. persistence of significant symptoms beyond 6 months after injury [7].
Treatment in acute whiplash can be delayed and confused by multiple social, economic, and psychological factors [8]. Psychological factors such as depression, anxiety, expectations for recovery, and high psychological distress have been identified as important prognostic factors for WAD patients. Coping strategies such as diverting attention and increasing activity are related with positive outcomes [5]. In order to avoid chronicity, it is important to screen for prognostic factors in time. According to Walton et al, there are 9 significant predictors [5]:
- No postsecondary education
- Female gender
- History of previous neck pain
- Baseline neck pain intensity above 55/100
- Presence of neck pain at baseline
- Presence of headache at baseline
- Catastrophizing: there is evidence of catastrophizing and reinterpreting pain sensations being maladaptive for patients exposed to whiplash trauma [9].
- WAD grade 2 or 3
- No seat belt in use at time of collision [5]
Education provided by physiotherapist or general practitioner is important in prevention of chronic whiplash. The most important goals of the interventions are:
- Reassuring the patient
- Modulating maladaptive cognitions about WAD
- Activating the patient [5]
There is strong evidence for most forms of verbal education for whiplash patients in order to reduce pain, enhance neck mobility, and improve outcome. In acute patients oral information is equally efficacious as an active exercise program. In acute whiplash patients, a short oral education session is effective in reducing pain and enhancing mobility and recovery. Different types of education [5]:
1. Oral Education: there is strong evidence for providing oral education concerning the whiplash mechanisms and emphasizing physical activity and correct posture. It has better effect on pain, cervical mobility, and recovery, compared to rest and neck collars. Furthermore oral education would be as effective as active physiotherapy and mobilization.
2. Psycho – educational video: A brief psycho-educational video at bedside seems to have a profound effect on subsequent pain and medical utilization in acute whiplash patients, compared to the usual care [5].
3. Advice according to The Whiplash Book [7]:
- Reassurance that prognosis following a whiplash injury is good.
- Encouragement to return to normal activities as soon as possible using exercises to facilitate recovery
- Reassurance that pain is normal following a whiplash injury and patients should use analgesia consistently to control this
- Advice against using a soft collar [7].
Conclusions of the Cochrane review (Gross A., et al., Patient education for neck pain 2012):
With the exception of one trial, this review has not shown effectiveness for educational interventions, including advice to activate, advice on stress-coping skills, workplace ergonomics and self-care strategies. Future research should be founded on sound adult learning theory and learning skill acquisition [10].
EVIDENCE CONCERNING IMMOBILIZATION
| AUTHOR |
CONCLUSION |
LEVEL |
| Quebec Task Force 1988 [11] |
Prolonged immobilization may increase scar tissue in the neck and reduce cervical mobility | 2B |
| Mealey et al 1986 [12] |
Initial immobilization after whiplash injuries gave rise to prolonged symptoms. A more rapid improvement can be achieved by early active management without any consequent increase in discomfort | 3A |
| Borchgrevink GE et al 2008 [13] |
Advice to “act as usual” plus NSAIDs significantly improved some symptoms (including pain during daily activities, neck stiffness, memory, concentration, and headache) after 6 months compared with immobilisation plus 14 days' sick leave plus NSAIDs | 1A |
| Teasell R.W. et al 2010 [14] |
Immobilization with a soft collar is less effective than active mobilization and no more effective than advice to act as usual. Active mobilization is associated with reduced pain intensity and limited evidence that mobilization may also improve ROM, although it is not clear whether active mobilization is any more effective than advice to act as usual. | 1A |
EVIDENCE CONCERNING THE USE OF (SOFT) COLLAR
| AUTHOR |
CONCLUSION |
LEVEL |
| Schnabel et al 2004 [15] |
Early exercise therapy is superior to the collar therapy in reducing pain intensity and disability for whiplash injury | 2B |
| Binder A. 2008 [13] |
Instruction on mobilization exercises may be more effective than a soft collar at reducing pain at 6 weeks in people treated within 48 hours of a whiplash injury who all also took NSAIDs |
1A |
| Schnabel M et al 2008 [13] |
Exercises significantly reduce the proportion of people with neck pain at 6 weeks compared with a soft collar and significantly reduce pain and disability at 6 weeks | 1A |
EVIDENCE CONCERNING THE ADVICE TO “ACT AS NORMAL”
| AUTHOR |
CONCLUSION |
LEVEL |
| Binder A 2008 [13] |
Advice to "act as usual" plus NSAIDs may be more effective at 6 months than immobilization plus 14 days sick leave plus NSAIDs at improving neck stiffness in people with acute whiplash | 1A |
| Borchgrevink GE et al 2008 [13] |
Advice to “act as usual” plus NSAIDs significantly improved some symptoms (including pain during daily activities, neck stiffness, memory, concentration, and headache) after 6 months compared with immobilisation plus 14 days' sick leave plus NSAIDs | 1A |
| Yadla S et al 2008 [16] |
Early mobilization and return to activity may offer the best chance for recovery. | 1A |
| Teasell R.W. et al 2010 [14] |
It does not appear that providing educational information during the acute phase provides a significant measurable benefit. There is some indication that oral and/or video presentation of educational information may be more effective than the distribution of pamphlets. | 1A |
EVIDENCE CONCERNING PHYSICAL THERAPY
| AUTHOR |
CONCLUSION |
LEVEL |
| Verhagen AP 2008 [13] |
Limited evidence that active and passive interventions seemed more effective than no treatment. Less convincing evidence about active interventions compared with passive ones | 1A |
| Binder A 2008 [13] |
Instruction on mobilization exercises may be more effective than a soft collar at reducing pain at 6 weeks in people treated within 48 hours of a whiplash injury who all also took NSAIDs | 1A |
| Lamb S et al 2013 [17] |
Physiotherapy is recommended by several clinical guidelines. Recommended treatments include manual therapy, exercise, advice, and recognition of anxiety and psychological problems | 2A |
| Schnabel M et al 2008 [13] |
Exercises significantly reduced the proportion of people with neck pain at 6 weeks compared with a soft collar and significantly reduced pain and disability at 6 weeks | 1A |
| Scholten – Peeters G et al 2008 [13] |
No significant difference between physiotherapy (exercise or mobilization) and usual care in pain intensity, headache, or work activities measured at 8, 12, 26, or 52 weeks | 1A |
| Söderlund A 2008 [13] |
No significant difference between a regular exercise regimen versus the same exercise regimen plus instructions in disability or pain after 3 or 6 months | 1A |
| Binder A 2008 [13] |
Multimodal treatment (postural training, psychological support, eye fixation exer- cises, and manual treatment) may be more effective at improving pain at 1 and 6 months in people with whiplash due to a road traffic accident in the previous 2 months | 1A |
| Teasell R.W. et al 2010 [14] |
Exercise programs are significantly more effective in reducing pain intensity over both the short and medium term. Conversely, supplemental exercise programs added to mobilization programs may not be any more beneficial than mobilization programs alone. | 1A |
| Drescher K et al 2008 [18] |
Moderate evidence to support the use of postural exercises for decreasing pain and time off work in the treatment of patients with acute whiplash-associated disorders. No evidence exists to support the use of postural exercises for increasing neck range of motion. Conflicting evidence in support of neck stabilization exercises in the treatment of patients with acute whiplash-associated disorders. |
1A |
Example physical therapy:http://www.physio-pedia.com/Manual_Therapy_and_Exercise_for_Neck_Pain:_Clinical_Treatment_Tool-kit
Differential Diagnosis
[edit | edit source]
Cervical radiculopathy
Facticious disorder
Polymyalgia Rheumatica
Traumatic Brain Injury
Cervical herniated disk
Cervical myelopathy
Cervical osteoarthritis
Infection or osteomyelitis
Inflammatory rheumatologic disease
Malingering
Psychogenic pain disorder
Referred pain from cardiothoracic structures
Tumor or malignancy of cervical spine
Vascular abnormality of cervical structures
Key Evidence[edit | edit source]
Resources
[edit | edit source]
www.som.uq.edu.au/whiplash
Case Studies[edit | edit source]
add links to case studies here (case studies should be added on new pages using the case study template)
Recent Related Research (from Pubmed)[edit | edit source]
Failed to load RSS feed from http://eutils.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=1-3FRwfkWFsJ5dYt0p2AoMPYz9dXTssSdfQhdkGhALv98wFkZ9|charset=UTF-8|short|max=10: Error parsing XML for RSS
References[edit | edit source]
References will automatically be added here, see adding references tutorial.
- ↑ Delfini R, Dorizzi A, Facchinetti G, Faccioli F, Galzio R, Vangelista T. Delayed post-traumatic cervical instability. Surg Neurol. 1999;51:588-95.
- ↑ Sterling M., Man Ther. 2004 May;9(2):60-70. A proposed new classification system for whiplash associated disorders--implications for assessment and management.
- ↑ Stiell IG, Clement CM, McKnight RD, Brison R, Schull MJ, Rowe BH, Worthington JR, Eisenhauer MA, Cass D, Greenberg G, MacPhail I, Dreyer J, Lee JS, Bandiera G, Reardon M, Holoroyd B, Lesiuk H, Wells GA. The Canadian c-spine rule versus the NEXUS low-risk criteria in patients with trauma. N Engl J Med. 2003;349(26): 2510-2518.
- ↑ Sterling M, Jull G, Kenardy J. Physical and psychological factors maintain long-term predictive capacity post-whiplash injury. Pain. 2006;122:102-108.
- ↑ 5.0 5.1 5.2 5.3 5.4 5.5 5.6 Meeus M, Nijs J, Hamers V, Ickmans K, Oosterwijck JV. Pain Physician. The efficacy of patient education in whiplash associated disorders: a systematic review. 2012 Sep-Oct;15(5):351-61. LEVEL 1A
- ↑ Ferrari R, Rowe BH, Majumdar SR, Cassidy JD, Blitz S, Wright SC, Russell AS. Simple Educational Intervention to Improve the Recovery from Acute Whiplash: Results of a Randomized, Controlled Trial. Acad Emerg Med. 2005 Aug;12(8):699-706. LEVEL 2A
- ↑ 7.0 7.1 7.2 Lamb SE, Gates S, Underwood MR, Cooke MW, Ashby D, Szczepura A, Williams MA, Williamson EM, Withers EJ, Mt Isa S, Gumber A; MINT Study Team. Managing Injuries of the Neck Trial (MINT): design of a randomised controlled trial of treatments for whiplash associated disorders. BMC Musculoskelet Disord. 2007 Jan 26;8:7. LEVEL 2C
- ↑ Yadla S, Ratliff JK, Harrop JS. Whiplash: diagnosis, treatment, and associated injuries. Curr Rev Musculoskelet Med. 2008 Mar;1(1):65-8. LEVEL 1A
- ↑ Carstensen TB. The influence of psychosocial factors on recovery following acute whiplash trauma. Dan Med J. 2012 Dec;59(12):B4560. LEVEL 2A
- ↑ Gross A., et al., Patient education for neck pain. COCHRANE DATABASE OF SYSTEMATIC REVIEWS. 2012;3
- ↑ Söderlund A, Olerud C, Lindberg P. Acute whiplash-associated disorders (WAD): the effects of early mobilization and prognostic factors in long-term symptomatology. Clin Rehabil. 2000 Oct;14(5):457-67. LEVEL 2B
- ↑ Mealy K, Brennan H, Fenelon GC. Early mobilization of acute whiplash injuries. Br Med J Clin Res Ed). 1986 Mar 8;292(6521):656-7. LEVEL 3A
- ↑ 13.00 13.01 13.02 13.03 13.04 13.05 13.06 13.07 13.08 13.09 13.10 Binder AI. Neck pain. Clin Evid (Online). 2008 Aug 4;2008. LEVEL 1A
- ↑ 14.0 14.1 14.2 Teasell RW, McClure JA, Walton D, Pretty J, Salter K, Meyer M, Sequeira K, Death B. A research synthesis of therapeutic interventions for whiplash-associated disorder (WAD): part 2 - interventions for acute WAD. Pain Res Manag. 2010 Sep-Oct;15(5):295-304. LEVEL 1A
- ↑ Schnabel M, Ferrari R, Vassiliou T, Kaluza G. Randomised, controlled outcome study of active mobilisation compared with collar therapy for whiplash injury. Emerg Med J. 2004 May;21(3):306-10. LEVEL 2B
- ↑ Yadla S, Ratliff JK, Harrop JS. Whiplash: diagnosis, treatment, and associated injuries. Curr Rev Musculoskelet Med. 2008 Mar;1(1):65-8. LEVEL 1A
- ↑ Lamb SE, Gates S, Williams MA, Williamson EM, Mt-Isa S, Withers EJ, Castelnuovo E, Smith J, Ashby D, Cooke MW, Petrou S, Underwood MR; Managing Injuries of the Neck Trial (MINT) Study Team. Emergency department treatments and physiotherapy for acute whiplash: a pragmatic, two-step, randomised controlled trial. Lancet. 2013 Feb 16;381(9866):546-56. LEVEL 2A
- ↑ Drescher K, Hardy S, Maclean J, Schindler M, Scott K, Harris SR. Efficacy of postural and neck-stabilization exercises for persons with acute whiplash-associated disorders: a systematic review. Physiother Can. 2008 Summer;60(3):215-23 LEVEL 1A