Whiplash Associated Disorders
Original Editor - Hannah Norton
Top Contributors - Kim Jackson, Rachael Lowe, Okebanama Nelson Onyebuchi, Lucinda hampton, Tarina van der Stockt, Admin, Hannah Norton, Van Horebeek Erika, Sigrid Bortels, Anouck Leo, WikiSysop, Steffen Kistmacher, Robin Tacchetti, Joshua Samuel, Ine Van de Weghe, Simisola Ajeyalemi, Rucha Gadgil, 127.0.0.1, Wanda van Niekerk, Jess Bell and Olajumoke Ogunleye
Clinically Relevant Anatomy
[edit | edit source]
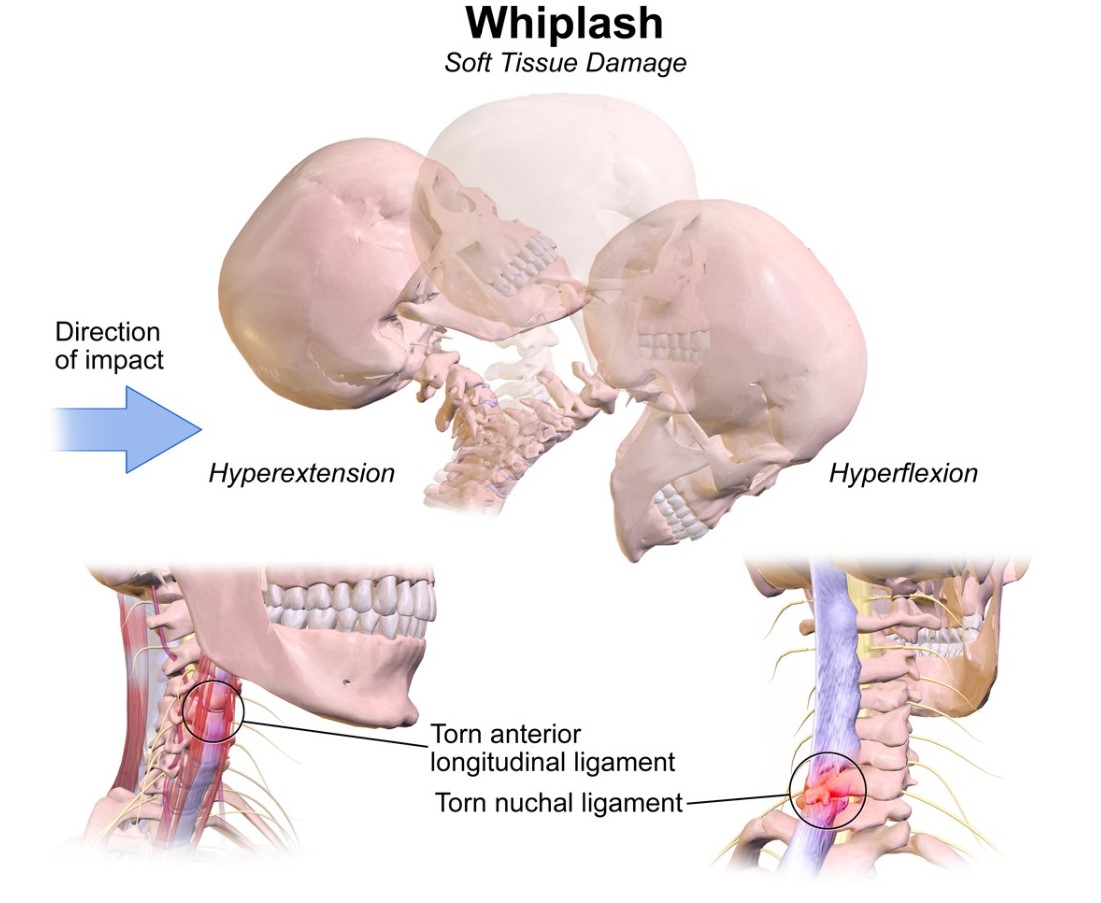
Whiplash and whiplash associated disorders (WAD) affects variable areas of the cervical spine, depending on the force and direction of impact as well as many other factors. In a whiplash injury, bony structures, ligamentous structures, muscles, neurological structures, and other connective tissue may be affected. Anatomic causes of pain can be any of these structures, with the strain injury resulting in secondary edema, hemorrhage, and inflammation.
Mechanism of Injury / Pathological Process
[edit | edit source]
The mechanism of injury is variable, usually involving a motor vehicle accident but also including causes such as sports injury, child abuse, blows to the head from a falling object, or similar accelleration-decceleration event.
Clinical Presentation[edit | edit source]
The most common presentation will be sub-occipital headaches and/or neck pain that is constant or motion-induced. There may be up to 48 hrs delay of symptom onset from the initial injury. Other signs include neurologic signs, dizziness, tinnitus, visual disturbances, UE radicular pain, difficulty sleeping due to pain, and difficulty concentrating/poor memory. (eMedicine) It is important to provide a thorough spinal exam and neurologic exam in patient with WAD to screen for delayed-onset of cervical spine instability or myelopathy. [1]
QTFC (Quebec Task Force Classification)
[edit | edit source]
The Quebec Task Force was a task force sponsored by a public insurer in Canada. They submitted recommendations regarding classification and treatment of WAD, which was used to develop a guide for managing whiplash in 1995. An updated report was published in 2001. Each of the grades corresponds to a specific treatment recommendation.
| QTFC Grade |
Clinical presentation |
| 0 |
No complaint about neck pain No physical signs |
| I |
Nec complaints of pain, stiffness or tenderness only No physical signs |
| II |
Neck complaint Musculoskeletal signs including
|
| III |
Neck complaint Musculosceletal signs Neurological signs including:
|
| IV |
Neck complaint and fracture or dislocation |
MQTFC (Modified Quebec Task Force Classification) [2]
|
Proposed classification grade |
Physical and psychological impairments present |
| WAD 0 |
No complaints about neck pain No physical signs |
| WAD I |
No complaints of pain, stiffness or tenderness only No physical signs |
| WAD IIA |
Neck complaint Motor impairment
Sensory Impairment
|
| WAD IIB |
Neck complaint Motor impairment
Sensory Impairment
Psychological impairment
|
| WAD IIC |
Neck complaint
Motor impairment
Sensory Impairment
Psychological impairment
|
| WAD III |
Neck complaint Motor impairment
Sensory Impairment
Neurological signs of conduction loss including:
Psychological impairment
|
| WAD IV |
Fracture or dislocation |
Diagnostic Procedures[edit | edit source]
Canadian C-Spine Rule (CCR): algorithm to determine the necessity for cervical spine radiography in alert and stable patients presenting with trauma and cervical spine injury. [3]
Management / Interventions
[edit | edit source]
Management approaches for patients with WAD are poorly researched. These patients often do not fit into treatment categories as defined for other cervical pain problems due to multiple factors, and even within the WAD group there are multiple variances which warrant individualized treatment approaches. The most recent evidence supports the use of Sterling's classification system for WAD. [4]
ACUTE WHPLASH
[edit | edit source]
Whiplash – associated disorder (WAD) is a debilitating and costly condition of at least 6-month duration. Although the majority of patients with whiplash show no physical signs 1 studies have shown that as many as 50% of victims of whiplash injury (grade 1 or 2 WAD) will still be experiencing chronic neck pain and disability six months later ². In most cases, symptoms are short lived, but a substantial minority go on to develop LWS (late whiplash syndrome), i.e. persistence of significant symptoms beyond 6 months after injury 3.
Treatment in acute whiplash can be delayed and confused by multiple social, economic, and psychological factors 4. Psychological factors such as depression, anxiety, expectations for recovery, and high psychological distress have been identified as important prognostic factors for WAD patients. Coping strategies such as diverting attention and increasing activity are related with positive outcomes 1. In order to avoid chronicity, it is important to screen for prognostic factors in time. According to Walton et al, there are 9 significant predictors 1:
- No postsecondary education
- Female gender
- History of previous neck pain
- Baseline neck pain intensity above 55/100
- Presence of neck pain at baseline
- Presence of headache at baseline
- Catastrophizing: there is evidence of catastrophizing and reinterpreting pain sensations being maladaptive for patients exposed to whiplash trauma 14.
- WAD grade 2 or 3
- No seat belt in use at time of collision 1
Education provided by physiotherapist or general practitioner is important in prevention of chronic whiplash. The most important goals of the interventions are:
- Reassuring the patient
- Modulating maladaptive cognitions about WAD
- Activating the patient 1
There is strong evidence for most forms of verbal education for whiplash patients in order to reduce pain, enhance neck mobility, and improve outcome. In acute patients oral information is equally efficacious as an active exercise program. In acute whiplash patients, a short oral education session is effective in reducing pain and enhancing mobility and recovery. Different types of education1:
1. Oral Education: there is strong evidence for providing oral education concerning the whiplash mechanisms and emphasizing physical activity and correct posture. It has better effect on pain, cervical mobility, and recovery, compared to rest and neck collars. Furthermore oral education would be as effective as active physiotherapy and mobilization.
2. Psycho – educational video: A brief psycho-educational video at bedside seems to have a profound effect on subsequent pain and medical utilization in acute whiplash patients, compared to the usual care 1.
3. Advice according to The Whiplash Book ³:
- Reassurance that prognosis following a whiplash injury is good.
- Encouragement to return to normal activities as soon as possible using exercises to facilitate recovery
- Reassurance that pain is normal following a whiplash injury and patients should use analgesia consistently to control this
- Advice against using a collar ³.
Conclusions of the Cochrane review (Gross A., et al., Patient education for neck pain 2012):
With the exception of one trial, this review has not shown effectiveness for educational interventions, including advice to activate, advice on stress-coping skills, workplace ergonomics and self-care strategies. Future research should be founded on sound adult learning theory and learning skill acquisition.
Differential Diagnosis
[edit | edit source]
Cervical radiculopathy
Facticious disorder
Polymyalgia Rheumatica
Traumatic Brain Injury
Cervical herniated disk
Cervical myelopathy
Cervical osteoarthritis
Infection or osteomyelitis
Inflammatory rheumatologic disease
Malingering
Psychogenic pain disorder
Referred pain from cardiothoracic structures
Tumor or malignancy of cervical spine
Vascular abnormality of cervical structures
Key Evidence[edit | edit source]
Resources
[edit | edit source]
www.som.uq.edu.au/whiplash
Case Studies[edit | edit source]
add links to case studies here (case studies should be added on new pages using the case study template)
Recent Related Research (from Pubmed)[edit | edit source]
Failed to load RSS feed from http://eutils.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=1-3FRwfkWFsJ5dYt0p2AoMPYz9dXTssSdfQhdkGhALv98wFkZ9|charset=UTF-8|short|max=10: Error parsing XML for RSS
References[edit | edit source]
References will automatically be added here, see adding references tutorial.
- ↑ Delfini R, Dorizzi A, Facchinetti G, Faccioli F, Galzio R, Vangelista T. Delayed post-traumatic cervical instability. Surg Neurol. 1999;51:588-95.
- ↑ Sterling M., Man Ther. 2004 May;9(2):60-70. A proposed new classification system for whiplash associated disorders--implications for assessment and management.
- ↑ Stiell IG, Clement CM, McKnight RD, Brison R, Schull MJ, Rowe BH, Worthington JR, Eisenhauer MA, Cass D, Greenberg G, MacPhail I, Dreyer J, Lee JS, Bandiera G, Reardon M, Holoroyd B, Lesiuk H, Wells GA. The Canadian c-spine rule versus the NEXUS low-risk criteria in patients with trauma. N Engl J Med. 2003;349(26): 2510-2518.
- ↑ Sterling M, Jull G, Kenardy J. Physical and psychological factors maintain long-term predictive capacity post-whiplash injury. Pain. 2006;122:102-108.