Transcranial Electrical Nerve Stimulation for Dementia: Difference between revisions
No edit summary |
mNo edit summary |
||
| Line 11: | Line 11: | ||
== '''Cognitive Impairment Assessment''' == | == '''Cognitive Impairment Assessment''' == | ||
Evaluating the person with dementia requires standardised neuropsychological assessment tools. Among this tools, the most common one universally use is Mini Mental Status Examination<ref>[https://www.ncbi.nlm.nih.gov/pubmed/1202204 Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”: a practical method for grading the cognitive state of patients for the clinician. Journal of psychiatric research. 1975 Nov 1;12(3):189-98.]</ref> and for functional status, Functional Activities Questionnaire (FAQ) for older adults might be used<ref>[https://consultgeri.org/try-this/dementia/issue-d13 Mayo AM. Use of the Functional Activities Questionnaire in older adults with dementia. Try This: Best Practices in Nursing Care to Older Adults with Dementia D. 2012;13.]</ref>. More so, this tools can be used to monitor the person with major neurocognitive impairment progress on the intervention. | Evaluating the person with dementia requires standardised neuropsychological assessment tools. Among this tools, the most common one universally use is Mini Mental Status Examination<ref>[https://www.ncbi.nlm.nih.gov/pubmed/1202204 Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”: a practical method for grading the cognitive state of patients for the clinician. Journal of psychiatric research. 1975 Nov 1;12(3):189-98.]</ref> and for functional status, Functional Activities Questionnaire (FAQ) for older adults might be used<ref>[https://consultgeri.org/try-this/dementia/issue-d13 Mayo AM. Use of the Functional Activities Questionnaire in older adults with dementia. Try This: Best Practices in Nursing Care to Older Adults with Dementia D. 2012;13.]</ref>. More so, this tools can be used to monitor the person with major neurocognitive impairment progress on the intervention. | ||
== | == Mini Mental State Examination == | ||
Mini Mental State Examination is used to screen cognitive status of the older adults by screening of the cognitive domains like language, memory, attention and soon<ref>Folstein MF, Folstein SE, McHugh PR "Mini-mental state". A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975 Nov; 12(3):189-98.</ref>. This tool is easy to administer and it takes about 10-20 minutes to administer it. | |||
Person with neurocognitive impairment perform differently on the different domains of the tool. The person with [[Alzheimer's Disease|Alzheimer's disease]] perform lesser in test of orientation to time and place and the recall part of the memory test when compared with those with Lewy bodies, vascular and Parkinson type of neurocognitive impairment . | |||
lower score on the item that evaluates their orientation to time and place, and recall part of the memory test when compared to patients with dementia with Lewy bodies.<ref>Ala, TA; Hughes, LF; Kyrouac, GA; Ghobrial, MW; Elble, RJ. "The Mini-Mental Status exam may help in the differentiation of dementia with Lewy bodies and Alzheimer's disease". ''International Journal of Geriatric Psychiatry''. June 2002;'''17''' (6): 503–9. </ref><ref>Jefferson, AL; Cosentino, SA; Ball, SK; Bogdanoff, B; Leopold, N; Kaplan, E; Libon, DJ. "Errors produced on the mini-mental status examination and neuropsychological test performance in Alzheimer's disease, ischemic vascular dementia, and Parkinson's". ''The Journal of Neuropsychiatry and Clinical Neurosciences''. 2002;'''14''' (3): 311–20. </ref><ref>Palmqvist, S; Hansson, O; Minthon, L; Londos, E. "Practical suggestions on how to differentiate dementia with Lewy bodies from Alzheimer's disease with common cognitive tests". ''International Journal of Geriatric Psychiatry''. December 2009;'''24''' (12): 1405–12. </ref> However, it should not be used to exclusively diagnose or differentiate the different types of dementia.<ref>Arevalo-Rodriguez I.; Smailagic N.; Ciapponi A.; Sanchez-Perez E.; Giannakou A.; Figuls M.; Cullum S. "Mini-Mental Status Examination (MMSE) for the detection of Alzheimer's disease and other dementias in people with mild cognitive impairment (MCI)". 2015. </ref><ref>Creavin ST, Wisniewski S, Noel-Storr AH, et al. Mini-Mental State Examination (MMSE) for the detection of dementia in clinically unevaluated people aged 65 and over in community and primary care populations. ''Cochrane Database Syst Rev''. 2016;(1):CD011145.</ref> | |||
The Mini-Cog and revised Addenbrooke's Cognitive Examination are preferred alternatives to the Mini-Mental State Examination for dementia screening, and the Montreal Cognitive Assessment is a preferred alternative to detect mild cognitive impairment.<ref name=":0">Tsoi KK, Chan JY, Hirai HW, Wong SY, Kwok TC. Cognitive tests to detect dementia: a systematic review and meta-analysis. ''JAMA Intern Med''. 2015;175(9):1450–1458.</ref> | The Mini-Cog and revised Addenbrooke's Cognitive Examination are preferred alternatives to the Mini-Mental State Examination for dementia screening, and the Montreal Cognitive Assessment is a preferred alternative to detect mild cognitive impairment.<ref name=":0">Tsoi KK, Chan JY, Hirai HW, Wong SY, Kwok TC. Cognitive tests to detect dementia: a systematic review and meta-analysis. ''JAMA Intern Med''. 2015;175(9):1450–1458.</ref> | ||
Revision as of 07:01, 19 February 2020
Description[edit | edit source]
Although Transcutaneous electrical nerve stimulation is known for non-pharmacological pain control, some scholars showed that it might also be used for brain stimulation in person with dementia[1][2]. Application of TENS electrodes to head is called Cranial Electrical Nerve Stimulation (CES) or transcranial stimulation and it is one of the methods used to stimulate the brain of a person with dementia[1]. Despite a recent evidence that CES alone or combine with physical therapy improves some functional activities in person with possible cognitive impairment[3], trans-cranial electrical nerve stimulation is not a common practice among physiotherapists who are one of the experts in managing person with dementia. This paper will therefore provide information on the CES method of application to stimulate the brain of a person with dementia.
Dementia(Major Neurocognitive disorder)[edit | edit source]
DSM-5 detailed on the definition and diagnosis of neurocognitive disorders[4]. Dementia now addressed as a major neurocognitive disorder according to DSM-5 on neurocognitive disorder, is an impairment in one or more cognitive domain with functional status impairment[4], which is of concern to both patient and patient relative. A cognitive impairment without significant impact on the functional activities of the person with dementia is termed mild neurocognitive impairment. Neuropsychological and behavioural characteristics such as anxiety, depression…and sleeping disturbances are prominent feature of dementia[5][6]. This characteristics including neurocognitive impairment might improve with trans cranial electrical nerve stimulation[1][7][8]. Scholars affirmed that TENS might stimulate brain and improve both the cognitive impairment and the neuropsychological characteristics of the dementia[1]
Cognitive Impairment Assessment[edit | edit source]
Evaluating the person with dementia requires standardised neuropsychological assessment tools. Among this tools, the most common one universally use is Mini Mental Status Examination[9] and for functional status, Functional Activities Questionnaire (FAQ) for older adults might be used[10]. More so, this tools can be used to monitor the person with major neurocognitive impairment progress on the intervention.
Mini Mental State Examination[edit | edit source]
Mini Mental State Examination is used to screen cognitive status of the older adults by screening of the cognitive domains like language, memory, attention and soon[11]. This tool is easy to administer and it takes about 10-20 minutes to administer it.
Person with neurocognitive impairment perform differently on the different domains of the tool. The person with Alzheimer's disease perform lesser in test of orientation to time and place and the recall part of the memory test when compared with those with Lewy bodies, vascular and Parkinson type of neurocognitive impairment .
lower score on the item that evaluates their orientation to time and place, and recall part of the memory test when compared to patients with dementia with Lewy bodies.[12][13][14] However, it should not be used to exclusively diagnose or differentiate the different types of dementia.[15][16]
The Mini-Cog and revised Addenbrooke's Cognitive Examination are preferred alternatives to the Mini-Mental State Examination for dementia screening, and the Montreal Cognitive Assessment is a preferred alternative to detect mild cognitive impairment.[1]
Scoring and Interpretation of Scores[edit | edit source]
The Mini-mental state examination is scored on a scale of 0-30 with scores > 25 interpreted as normal cognitive status.
- Severe cognitive impairment: 0-17
- Mild cognitive impairment: 18-23
- No cognitive impairment: 24-30
Interpretation of the mental status examination must take into account the patient's native language, education level, and culture as these factors can affect perfromance.[17]
Validity[edit | edit source]
In 14 studies, the MMSE had a sensitivity of 88.3% (95% confidence interval [CI], 81.3% to 92.9%) and a specificity of 86.2% (95% CI, 81.8% to 89.7%) for dementia, with a score cutoff of 23 to 25 indicating significant impairment.[1] A more recent meta-analysis of 108 cohort studies found a sensitivity of 81% (95% CI, 78% to 84%) and specificity of 89% (95% CI, 87% to 91%)[18]
Cranial Electrical Nerve Stimulation (CES) intervention[edit | edit source]
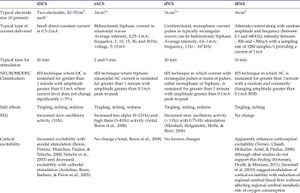
Using electrotherapy modalities like TENS requires assessment like skin sensation test to determine if the intervention will be appropriate. CES application requires several parameter based on the objectives to achieve in the person with dementia[8] [19] . Moreno-Duarte[8] affirmed that low level intensity transcranial electrical nerve stimulation is the major documented intensity level of CES application and there are four methods to this: transcranial direct current stimulation (tDCS), transcranial pulsed current stimulation (tPCS), transcranial alternating current stimulation(tACS) and transcranial random noise stimulation (tRNS)(see figure 1 for the summary of the parameters used)[8]. Although, there is still some controversial in the use of CES among person with dementia, yet there are supporting evidence that using CES either combined with physiotherapy intervention or not improves cognitive, physical activities and behavioural characteristics[3][20]
Figure 1
CES in Physiotherapy Practice for Brain Stimulation[edit | edit source]
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 Cameron MH, Lonergan E, Lee H. Transcutaneous electrical nerve stimulation (TENS) for dementia. Cochrane Database of Systematic Reviews. 2003(3). Cite error: Invalid
<ref>tag; name ":0" defined multiple times with different content - ↑ Schabrun SM. Transcranial direct current stimulation: a place in the future of physiotherapy?. Physical Therapy Reviews. 2010 Aug 1;15(4):320-6.
- ↑ 3.0 3.1 Yotnuengnit P, Bhidayasiri R, Donkhan R, Chaluaysrimuang J, Piravej K. Effects of transcranial direct current stimulation plus physical therapy on gait in patients with Parkinson disease: a randomized controlled trial. American journal of physical medicine & rehabilitation. 2018 Jan 1;97(1):7-15.
- ↑ 4.0 4.1 American Psychiatric Association. Diagnostic and statistical manual of mental disorders (DSM-5®). American Psychiatric Pub; 2013 May 22.
- ↑ Burke AD, Goldfarb D, Bollam P, Khokher S. Diagnosing and Treating Depression in Patients with Alzheimer’s Disease. Neurology and therapy. 2019 Aug 1:1-26.
- ↑ Müller-Spahn F. Behavioral disturbances in dementia. Dialogues in clinical neuroscience. 2003 Mar;5(1):49.
- ↑ Das N, Spence JS, Aslan S, Vanneste S, Mudar R, Rackley A, Quiceno M, Chapman SB. Cognitive training and transcranial direct current stimulation in mild cognitive impairment: A randomized pilot trial. Frontiers in Neuroscience. 2019;13:307.
- ↑ 8.0 8.1 8.2 8.3 Moreno-Duarte I, Gebodh N, Schestatsky P, Guleyupoglu B, Reato D, Bikson M, Fregni F. Transcranial electrical stimulation: transcranial direct current stimulation (tDCS), transcranial alternating current stimulation (tACS), transcranial pulsed current stimulation (tPCS), and transcranial random noise stimulation (tRNS). InThe stimulated brain 2014 Jan 1 (pp. 35-59). Academic Press.
- ↑ Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”: a practical method for grading the cognitive state of patients for the clinician. Journal of psychiatric research. 1975 Nov 1;12(3):189-98.
- ↑ Mayo AM. Use of the Functional Activities Questionnaire in older adults with dementia. Try This: Best Practices in Nursing Care to Older Adults with Dementia D. 2012;13.
- ↑ Folstein MF, Folstein SE, McHugh PR "Mini-mental state". A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975 Nov; 12(3):189-98.
- ↑ Ala, TA; Hughes, LF; Kyrouac, GA; Ghobrial, MW; Elble, RJ. "The Mini-Mental Status exam may help in the differentiation of dementia with Lewy bodies and Alzheimer's disease". International Journal of Geriatric Psychiatry. June 2002;17 (6): 503–9.
- ↑ Jefferson, AL; Cosentino, SA; Ball, SK; Bogdanoff, B; Leopold, N; Kaplan, E; Libon, DJ. "Errors produced on the mini-mental status examination and neuropsychological test performance in Alzheimer's disease, ischemic vascular dementia, and Parkinson's". The Journal of Neuropsychiatry and Clinical Neurosciences. 2002;14 (3): 311–20.
- ↑ Palmqvist, S; Hansson, O; Minthon, L; Londos, E. "Practical suggestions on how to differentiate dementia with Lewy bodies from Alzheimer's disease with common cognitive tests". International Journal of Geriatric Psychiatry. December 2009;24 (12): 1405–12.
- ↑ Arevalo-Rodriguez I.; Smailagic N.; Ciapponi A.; Sanchez-Perez E.; Giannakou A.; Figuls M.; Cullum S. "Mini-Mental Status Examination (MMSE) for the detection of Alzheimer's disease and other dementias in people with mild cognitive impairment (MCI)". 2015.
- ↑ Creavin ST, Wisniewski S, Noel-Storr AH, et al. Mini-Mental State Examination (MMSE) for the detection of dementia in clinically unevaluated people aged 65 and over in community and primary care populations. Cochrane Database Syst Rev. 2016;(1):CD011145.
- ↑ Faber RA. The neuropsychiatric mental status examination. Semin Neurol. 2009;29(3):185–193. Level of evidence C
- ↑ Lin JS, O'Connor E, Rossom RC, Perdue LA, Eckstrom E. Screening for cognitive impairment in older adults: a systematic review for the U.S. Preventive Services Task Force [published correction appears in Ann Intern Med. 2014;160(1):72]. Ann Intern Med. 2013;159(9):601–612.
- ↑ Peterchev AV, Wagner TA, Miranda PC, Nitsche MA, Paulus W, Lisanby SH, Pascual-Leone A, Bikson M. Fundamentals of transcranial electric and magnetic stimulation dose: definition, selection, and reporting practices. Brain stimulation. 2012 Oct 1;5(4):435-53.
- ↑ Elsner B, Kugler J, Pohl M, Mehrholz J. Transcranial direct current stimulation (tDCS) for improving activities of daily living, and physical and cognitive functioning, in people after stroke. Cochrane Database of Systematic Reviews. 2016(3).
- ↑ Moreno-Duarte I, Gebodh N, Schestatsky P, Guleyupoglu B, Reato D, Bikson M, Fregni F. Transcranial electrical stimulation: transcranial direct current stimulation (tDCS), transcranial alternating current stimulation (tACS), transcranial pulsed current stimulation (tPCS), and transcranial random noise stimulation (tRNS). InThe stimulated brain 2014 Jan 1 (pp. 35-59). Academic Press.