The Physiotherapy Management of Thalassaemia and Sickle Cell Anaemia
Original Editors - Mariam Hashem
Top Contributors - Mariam Hashem, Tarina van der Stockt, Kim Jackson, Lucinda hampton, Jess Bell, Aminat Abolade and Stacy Schiurring
Thalassaemia[edit | edit source]
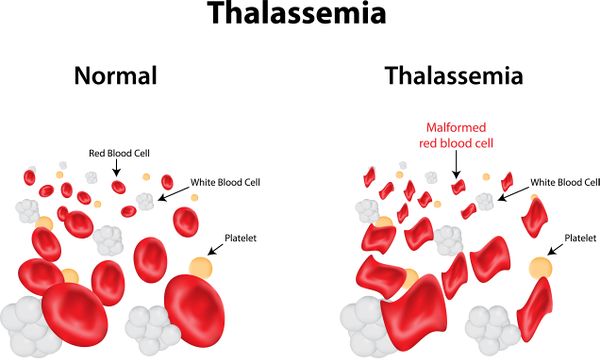
Thalassaemia is one of the most common inherited diseases worldwide. It is defined as an autosomal recessive blood disorder that results from reduction or absence in the production of globin chains that make up the haemoglobin (Hb) leading to abnormal destruction of erythrocytes and consequently decreased oxygen delivery[1][2]. As a result, patients have a range of symptoms and complications that impose a large burden on individuals and the healthcare systems[3].
Thalassaemia is derived from the Greek word "Thalassa" which means ''sea''[4]. It's also referred to as ''Mediterranean Anaemia''. It mainly affects individuals originating from the Mediterranean area, Middle East, Transcaucasia, Central Asia, Indian subcontinent, and Southeast Asia[5].
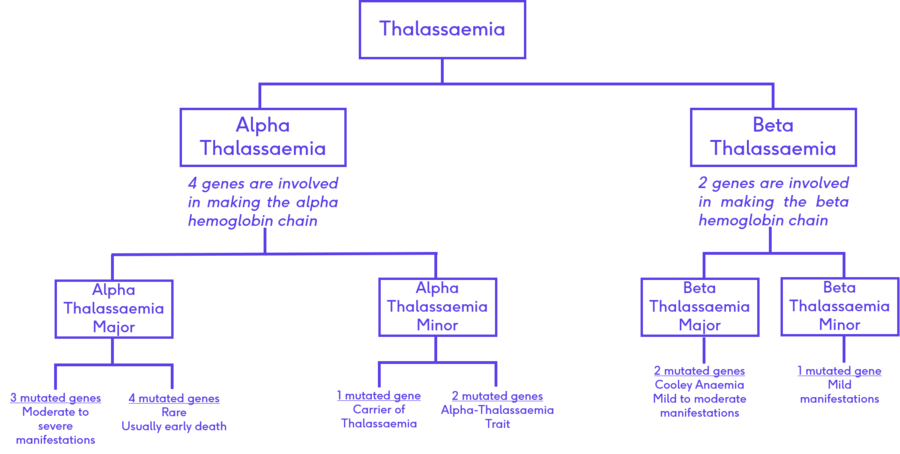
There are two types of Thalassaemia: α- and β- and complex thalassemias depending on the type of the involved globin chain. Alpha Thalassaemia is developed when the alpha gene is affected and likewise, in beta-thalassemia, the globin chain is affected or the abnormal haemoglobin involved is beta-globin gen[6].
The incidence rate is about 4.4 of every 10000 live births globally and approximately about 5% of all population[5]. It is estimated that there are 270 million carriers of Alpha thalassemia genes. More than 95% of children have alpha thalassemia are Asian, Indian, or Middle Eastern[7]. About 80 to 90 million people are carriers of β-thalassemia genes, that’s about 1% to 1.5% of the worldwide population[8]
It has been estimated that the globally there are 9million carriers of Thalassaemia and Sickle cell anaemia become pregnant each year[9].
Clinically, Thalassemia is classified into three forms[6]:
- Thalassemia major: this is a severe form of anaemia where patients need continuous blood transfusions throughout their lives.
- Thalassemia intermedia: mild to moderate anaemia, patients occasionally need blood transfusions
- Thalassemia minor or trait: patients have mild symptoms and they usually don’t need blood transfusions.
The Alpha haemoglobin chain is formed of four genes, Alpha Thalassaemia is classified according to the number of mutated genes[11][5]:
- A person is a carrier when one gene is mutated
- Alpha Thalassaemia Trait: when two genes are mutated leading to mild manifestations
- Alpha Thalassaemia Major: when three genes are mutated leading to moderate to sever symptoms
- Rarely, four genes might be mutated leading to an early death.
Beta haemoglobin chain is formed of two genes[5]:
Beta Thalassaemia Minor develops when one gene is mutated. Patients experience mild symptoms
Cooley's Anaemia or Beta Thalassaemia Major develops when two genes are mutated leading to moderate to severe manifestation
Symptoms & Complications[edit | edit source]
The severity of symptoms depends on the type and number of mutated genes. Thalassaemia has different symptoms[12][5]:
- Pain
- Fatigue
- Brittle bones
- Poor appetite
- Liability to infection
- Dark urine
- Generalized body weakness
Complications[5]:
- Anaemia due to the deficiency of haemoglobin.
- Hepatosplenomegaly: abnormal enlargement of the abdomen.
- Iron overload as a result of repeated blood transfusion. Consequently, a patient may develop further complications such as:
- Endocrine complications such as diabetes, glucose intolerance, decreased production of growth hormone and hypogonadism
- Cardiac disorders, for example, congestive heart failure or arrhythmias
- Hepatic disorders such as cirrhosis and liability to have HCV
Diagnosis[13]:
The diagnosis is based on the Red Blood Cells (RBC) count specifically the number of erythrocytes.
Another important blood mark in the diagnosis of Thalassaemia are genetic testing, Haemoglobin electrophoresis and reticulocyte count (the number of young RBCs formed from bone marrow)
Medical management[14]:
Although Thalassaemia has a wide range of symptoms and classifications, there are general principals of medical management.
Accurate diagnosis is crucial. The family history should be documented and studied to help assess relative risks and future decisions of the family. Medical management includes[5]:
- Regular transfusions with observations to prevent unnecessary complications [15]
- Folic acid supplements are also included in the long term management
- Chelation therapy which refers to the extraction the iron excess to prevent iron overload.
- STEM cell transplantation
- Genetic therapy
- Bone marrow transplantation.
- Psychological therapy
Sickle Cell Anaemia[edit | edit source]
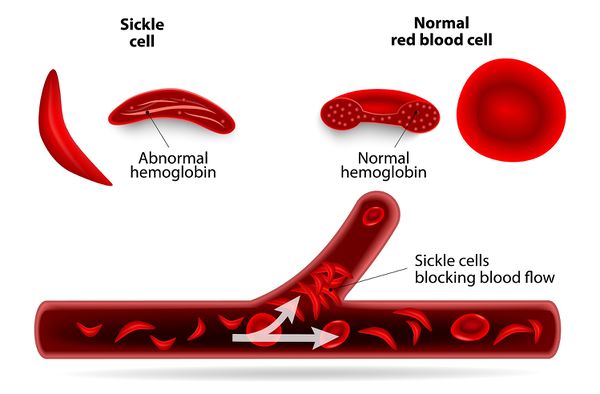
Sickle cell anaemia is an autosomal recessive inherited group of blood disorders characterized by the presences of atypical haemoglobin molecules (haemoglobin S) leading to distortion of erythrocytes red blood cells into a sickle, or crescent, shape. It is characterized by the presences of abnormal haemoglobin, excessive erythrocytes destruction. The crescent or sickle-shaped erythrocytes are approximately 15 microns[16].
Sickle cell anaemia was diagnosed in 1910 by Dr Ernest who described the red blood cells of a patient with anaemia symptoms as “having the shape of a sickle”[17]
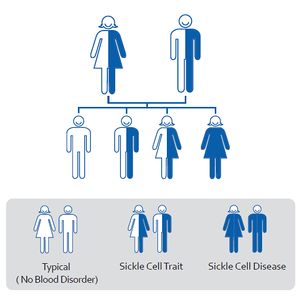
Sickle Cell Anemia is inherited in an autosomal recessive manner due to mutation of the HBB gene leading to Hemoglobin S production[18]
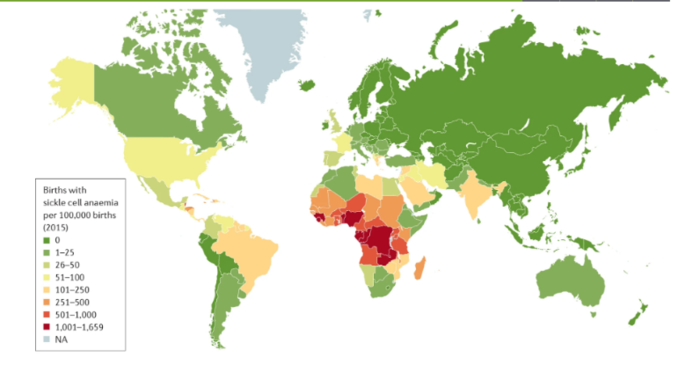
Sickle Cell anaemia mainly affects people with African origins but it has spread globally. The estimated prevalence rate is 250,000 children are born annually with sickle cell anaemia worldwide[19]. Around 1% of all births in Africa are inheriting sickle cell disease, causing 6–15% of all deaths in children younger than 5 years[20].
Classification[edit | edit source]
There are several types of sickle cell anaemia but the most common are: Sickle Cell Anemia (SS), Sickle Hemoglobin-C Disease (SC), Sickle Beta-Plus Thalassemia and Sickle Beta-Zero Thalassemia[21].
Sickle Hemoglobin-D Disease (Hemoglobin SD), Hemoglobin SE, And Sickle Hemoglobin-O Disease (Hemoglobin SO) are less common and are usually less severe types[22]
References[edit | edit source]
- ↑ Medline Plus. Thalassemia [Internet]. US National Libraray of Medicine. 2020 [cited 2020 Jul 21]. Available from: https://medlineplus.gov/ency/article/000587.htm
- ↑ Cao A, Kan YW. The prevention of thalassemia. Cold Spring Harbor perspectives in medicine. 2013 Feb 1;3(2):a011775.
- ↑ Lai K, Huang G, Su L, He Y. The prevalence of thalassemia in mainland China: evidence from epidemiological surveys. Scientific reports. 2017 Apr 19;7(1):1-1.
- ↑ Saggar SA. Thalassemia: Cultural and Historical Perspectives [Internet]. Science Museum. 2019 [cited 2020 Jul 12]. Available from: https://blog.sciencemuseum.org.uk/thalassemia-cultural-and-historical-perspectives/
- ↑ 5.0 5.1 5.2 5.3 5.4 5.5 5.6 Kora A. The Physiotherapy Management of Thalassaemia and Sickle Cell Anaemia. Physioplus Course 2020
- ↑ 6.0 6.1 Aszhari FR, Rustam Z, Subroto F, Semendawai AS. Classification of thalassemia data using random forest algorithm. InJournal of Physics: Conference Series 2020 Mar 1 (Vol. 1490, No. 1, p. 012050). IOP Publishing.
- ↑ Cheerva A. What is the global prevalence of alpha thalassemia syndromes? [Internet]. Medscape. 2018 [cited 2020 Jul 18]. Available from: https://www.medscape.com/answers/955496-156159/what-is-the-global-prevalence-of-alpha-thalassemia--thalassemia-syndromes
- ↑ Prevalence and Clinical Presentation of Beta Thalassemia [Internet]. HCPLive Network. 2020 [cited 2020 Jul 18]. Available from: https://rarediseases.org/rare-diseases/thalassemia-major/
- ↑ Modell B, Darlison M. Global epidemiology of haemoglobin disorders and derived service indicators. Bulletin of the World Health Organization. 2008;86:480-7.
- ↑ What is Thalassemia? . Available from:https://www.youtube.com/watch?v=JxuupecxHO8[last accessed 30/09/2020]
- ↑ Thalassemia [Internet]. Mayo Foundation for Medical Education and Research. 2020 [cited 2020 Jul 21]. Available from:https://www.mayoclinic.org/diseases-conditions/thalassemia/symptoms-causes/syc-20354995
- ↑ Nienhuis AW, Nathan DG. Pathophysiology and clinical manifestations of the β- thalassemias. Cold Spring Harb Perspect Med. 2012;2(12):1–13.
- ↑ Clevland Clinic. Thalassemias: Diagnosis and Tests [Internet]. 2020 [cited 2020 Jul 21].Available from: https://my.clevelandclinic.org/health/diseases/14508-thalassemias/diagnosis-and-tests
- ↑ Olivieri NF, Brittenham GM. Management of the thalassemias. Cold Spring Harb Perspect Med. 2013;3(6):1–14.
- ↑ Allen A, Fisher C, Premawardhena A, Peto T, Allen S, Arambepola M, Thayalsutha V, Olivieri N, Weatherall DBlood. 2010 Dec 9; 116(24):5368-70.
- ↑ Robinson IB, Sarnat BG. Roentgen Studies of the Maxillae and Mandible in Sickle-Cell Anemia. Radiology [Internet]. 1952 Apr 1;58(4):517–23. Available from: https://doi.org/10.1148/58.4.517
- ↑ Winter WP. A Brief History of Sickle Cell Disease [Internet]. Howard University Hospitals. 2020 [cited 2020 Aug 3]. Available from: http://www.sicklecell.howard.edu/ABriefHistoryofSickleCellDisease.htm
- ↑ Mumal I. Inheritance of Sickle Cell Disease [Internet]. Sickle Cell Disease News. 2020 [cited 2020 Aug 3]. Available from: https://sicklecellanemianews.com/inheritance-sickle-cell-anemia/
- ↑ Lervolino LG, Baldin PEA, Picado SM, Calil KB, Viel AA, Campos LAF. Prevalence of sickle cell disease and sickle cell trait in national neonatal screening studies. Rev Bras Hematol Hemoter. 2011;33(1):49–54.
- ↑ Uyoga S, Macharia AW, Mochamah G, Ndila CM, Nyutu G, Makale J, et al. The epidemiology of sickle cell disease in children recruited in infancy in Kilifi, Kenya: a prospective cohort study. Lancet Glob Heal [Internet]. 2019;7(10):e1458–66. Available from: http://dx.doi.org/10.1016/S2214-109X(19)30328-6
- ↑ Types of Sickle Cell Disease [Internet]. Sickle Cell Association of the National Capital Area. 2017 [cited 2020 Aug 3]. Available from: http://scancainc.org/learn/types-of-sickle-cell-disease/
- ↑ Types of Sickle Cell Anemia [Internet]. Global Blood Therapeutics Inc. 2020 [cited 2020 Aug 3]. Available from: https://sicklecellspeaks.com/understanding-sickle-cell/types-of-sickle-cell/