Somatic Symptom Disorder: Difference between revisions
No edit summary |
No edit summary |
||
| Line 101: | Line 101: | ||
The diagnostic criteria for SSD focuses not only on somatic symptoms but also on psychological responses, including the patient's emotions, thinking and behavior of their symptoms. The severity of SSD can also be diagnosed as mild, moderate or severe. Diagnosis may or may not include another diagnosed medical conditions. Medically unexplained symptoms are no longer included in the diagnostic criteria and are discouraged. Describing the patients symptoms as medically unexplained is inaccurate because oftentimes symptoms are unexamined. In addition, patients suffering from somatic complaints may feel that medical professionals view their symptoms as inauthentic. <br> | The diagnostic criteria for SSD focuses not only on somatic symptoms but also on psychological responses, including the patient's emotions, thinking and behavior of their symptoms. The severity of SSD can also be diagnosed as mild, moderate or severe. Diagnosis may or may not include another diagnosed medical conditions. Medically unexplained symptoms are no longer included in the diagnostic criteria and are discouraged. Describing the patients symptoms as medically unexplained is inaccurate because oftentimes symptoms are unexamined. In addition, patients suffering from somatic complaints may feel that medical professionals view their symptoms as inauthentic. <br> | ||
Dimsdale JE, Creed F, Escobar J, et al. Somatic symptom disorder: an important change in DSM. J Psychosom Res. 2013;75(3):223-8. | Dimsdale JE, Creed F, Escobar J, et al. Somatic symptom disorder: an important change in DSM. J Psychosom Res. 2013;75(3):223-8.<br> | ||
The interrater reliability of diagnoses for SSD was listed as 0.61 in adult diagnoses. B-type criteria also has good test-retest reliability among physicians with an ICC of 0.680. Global rating of the severity of a patient's symptoms was found to have acceptable reliability with an ICC of 0.483. <br> | The interrater reliability of diagnoses for SSD was listed as 0.61 in adult diagnoses. B-type criteria also has good test-retest reliability among physicians with an ICC of 0.680. Global rating of the severity of a patient's symptoms was found to have acceptable reliability with an ICC of 0.483. <br> | ||
Revision as of 16:42, 11 March 2014
Original Editors - Lauren Rouse & Laura Stigler from Bellarmine University's Pathophysiology of Complex Patient Problems project.
Top Contributors - Lauren Rouse, Laura Stigler, Elaine Lonnemann, Admin, Wendy Walker, WikiSysop, Kim Jackson and Vidya Acharya
Definition/Description
[edit | edit source]
Somatic symptom disorder (SSD), as defined by the DSM-V code, occurs in individuals experiencing exaggerated and disrupted physical symptoms in multiple areas of the body, accompanied by exaggerated thoughts impairing activities of daily living. Diagnosis of SSD requires that the individual has experienced these symptoms for at least six months. This disorder has recently been updated from DSM-IV code of "somatization disorder" to the DSM-V code of "SSD". The prior diagnosis required patient complaints from four different symptom groups; however, this is no longer required with the DSM-V code1. In addition, patients experiencing these symptoms associated with other comorbidities such as heart disease, osteoarthritis, or cancer were previously excluded from the DSM-IV diagnostic code. The DSM-V definition now includes these patients under the diagnostic code of SSD, even if the psychological symptoms were secondary to the primary diagnosis. These patients are considered appropriate for psychological treatment; however, a full psychological evaluation is needed to rule out other possible disorders2.
The DSM-V code has been implemented for a variety of reasons:
- The previous diagnosis of "somatoform disorders" is an ambiguous term and is not easily translatable between different languages, as it blends Latin and Greek roots. Somatic symptom disorder has made the diagnosis easily translatable.
- The previous DSM-IV diagnostic code utilized Medically Unexplained Symptoms as the definining characteristic. This terminology is no longer acceptable. Patients may feel their complaints are deemed illegitimate in the medical community. Medical diagnosis should also never be made on the absence of symptoms. Finally, these symptoms are often unexamined rather than unexplained.
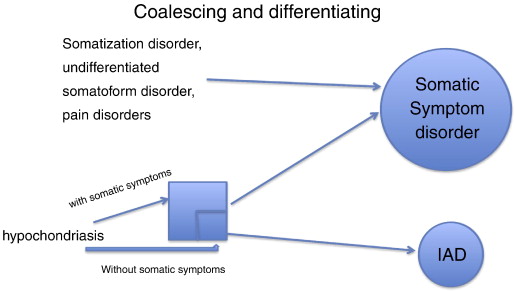
- Overlap between somatization disorder, undifferentiated somatoform disorder, hypochondriasis, and pain disorder made the DSM-IV code confusing and disorganized. The new code sets a boundary between SSD and illness anxiety disorder.
- Diagnostic criteria for previous DSM codes was confusing and unreliable, leading to strong specificity with weak sensitivity.
- Previous inclusion of "Undifferentiated Somatoform Disorder" in the DSM-IV code loosely defined the diagnosis making proper diagnosis inaccurate.
- Non-psychiatric physicians have rarely diagnosed the disorder due to the confusing nature of previous codes preventing accurate prevalence statistics of previous DSM codes. The new code has been implemented in attempt to improve communication between medical professionals of various backgrounds.
Dimsdale J, Creed F, Levenson J, et al. Somatic Symptom Disorder: An important change in DSM. Journal Of Psychosomatic Research [serial online]. September 2013;75(3):223-228. Available from: PsycINFO, Ipswich, MA. Accessed March 7, 2014.
Prevalence[edit | edit source]
Information about the prevalence of SSD is lacking due to the recent changes in the DSM-V code in 2013. The prevalence of the DSM-IV code of somatization disorder is more widely known and the following data has been obtained:
- For restrictive diagnoses, rates are low in community samples (0.1%) but this may be due to reporting bias3
- The disorder may be as high as 2% in community dwelling women, whereas some cases are reported to be as high as 11.6% of the population3
- The female-to-male ratio is 10:1 and may begin in childhood, adolescence, or early adulthood3.
- Older adults diagnosed with somatization disorder is a rare finding. Older patients should be referred to a medical specialist for an underlying medical illness or consider depression as the primary cause of the individual’s perception of pain3.
- 25% in neurology outpatient medical settings (P Fink, M)
- 27% in primary care (P Fink, L)
3. Van noorden MS, Giltay EJ, Van der wee NJ, Zitman FG. [The Leiden Routine Outcome Monitoring Study: mood, anxiety and somatoform disorders in patients attending a day clinic]. Tijdschr Psychiatr. 2014;56(1):22-31.
P Fink, M Steen Hansen, L SondergaardSomatoform disorders among first-time referrals to a neurology service
P Fink, L Sørensen, M Engberg, M Holm, P Munk-Jørgensen. Somatization in primary care. Prevalence, health care utilization, and general practitioner recognition. Psychosomatics, 4 (Jul–Aug 1999), pp. 330–338
Statistical prevalence on the prior DSM IV code is inaccurate do to the confusing description of the disoder; therefore, non-psychiatric physicians have rarely diagnosed somatoform disorders. In addition, psychiatric physicians used ambiguous terminology in diagnosis of patients with this disorder. Lack of consensus among the medical community has lead to inaccurate prevalence statistics. Despite the frequency encountered in clinics and studies in medical studies, prevalence among Anthem Blue Cross insured individuals was 0.00002 out of 28 million subscribers and appeared rarely in the medical databases of Medicare, Medicaid and Veteran's Administration. Creation of the new DSM V code is attempting to provide a straightforward and simplified definition of the disorder so that medical professionals are able to effectively communicate the medical diagnosis of SSD.
Dimsdale J, Creed F, Levenson J, et al. Somatic Symptom Disorder: An important change in DSM. Journal Of Psychosomatic Research [serial online]. September 2013;75(3):223-228. Available from: PsycINFO, Ipswich, MA. Accessed March 7, 2014.
Characteristics/Clinical Presentation[edit | edit source]
Associated Co-morbidities[edit | edit source]
add text here
Medications[edit | edit source]
Pharmacotherapy is not effective unless there are associated co-morbidites to SSD such as depression or anxiety.
www.inkling.com/read/behavioral-science-in-medicine-barbara-fadem-2nd/chapter-16/somatic-symptom-formaly. Accessed March 10th, 2014
Diagnostic Tests/Lab Tests/Lab Values[edit | edit source]
Criteria for SSD as defined by the American Psychiatric Assocation (APA):
| Table 1. |
| Criteria for Somatic Symptom Disorder. |
|
A. One or more somatic symptoms that are distressing or result in significant disruption of daily life. |
|
B. Excessive thoughts, feelings, behaviors related to the somatic symptoms or associated health concerns as manifested by at least one of the following: |
|
|
C. Although any one somatic symptom may not be continuously present, the state of being symptomatic is persistent (typically more than 6 months). |
| Reprinted with permission from the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, (Copyright (c) 2013). American Psychiatric Association. All rights reserved. |
The diagnostic criteria for SSD focuses not only on somatic symptoms but also on psychological responses, including the patient's emotions, thinking and behavior of their symptoms. The severity of SSD can also be diagnosed as mild, moderate or severe. Diagnosis may or may not include another diagnosed medical conditions. Medically unexplained symptoms are no longer included in the diagnostic criteria and are discouraged. Describing the patients symptoms as medically unexplained is inaccurate because oftentimes symptoms are unexamined. In addition, patients suffering from somatic complaints may feel that medical professionals view their symptoms as inauthentic.
Dimsdale JE, Creed F, Escobar J, et al. Somatic symptom disorder: an important change in DSM. J Psychosom Res. 2013;75(3):223-8.
The interrater reliability of diagnoses for SSD was listed as 0.61 in adult diagnoses. B-type criteria also has good test-retest reliability among physicians with an ICC of 0.680. Global rating of the severity of a patient's symptoms was found to have acceptable reliability with an ICC of 0.483.
HC Kraemer, DJ Kupfer, DE Clarke, WE Narrow, DA Regier. DSM5: how reliable is reliable enough? Am J Psychiatry, 169 (2012), pp. 13–15
Etiology/Causes
[edit | edit source]
There is no adequate evidence for the cause of SSD.
Currently, higher percentages of SSD has been found in persons with:
- Irritable bowel syndrome
- Chronic pain
- Post-traumatic stress disorder
- Antisocial personality disorder
- History if sexual or physical abuse
Available at: http://www.patient.co.uk/doctor/somatic-symptom-disorder. Accessed February 27, 2014.
Systemic Involvement[edit | edit source]
Patients diagnosed with the DSM-V disoder may present with the following systemic symptoms:
Cardiac
- Shortness of breath
- Palpitations
- Chest pain
Gastrointestinal
- Vomiting
- Abdominal pain
- Difficulty swallowing
- Nausea
- Bloating
- Diarrhea
Musculoskeletal
- Pain in the legs or arms
- Back and joint pain
Neurological
- Headaches
- Dizziness
- Amnesia
- Vision changes
- Paralysis or muscle weakness
Urogenital
- Pain during urination
- Low libido
- Dyspareunia
- Impotence
- Dysmenorrhea
Available at: http://www.patient.co.uk/doctor/somatic-symptom-disorder. Accessed February 27, 2014.
Medical Management (current best evidence)[edit | edit source]
The components of SSD currently treated include the following:
- Somatic symptoms
- Health related anxiety
- Preoccupation and rumination about health concerns
- Unhelpful illness behaviors
Treatments used as interventions for these components include:
- Cognitive therapy
- Behavioral techniques (relaxation training and mindfulness)
- Other psychotherapies
- Psychotropic medications
K Kroenke. Efficacy of treatment for somatoform disorders: a review of randomized controlled trials. Psychosom Med, 69 (2007), pp. 881–888
Physical Therapy Management (current best evidence)[edit | edit source]
add text here
Alternative/Holistic Management (current best evidence)[edit | edit source]
add text here
Differential Diagnosis[edit | edit source]
Disorders likely to be misdiagnosed as somatic symptom disorders:
- Early-stage connective tissue disorders (ex. systemic lupus erythematosus and rheumatoid arthritis)
- Central nervous system disorders (ex. brain tumor, multiple sclerosis, epilepsy, dementia, stroke, and myasthenia gravis)
- Endocrine disorders (ex. hypoglycemia, thyroid dysfunction and porphyria)
www.inkling.com/read/behavioral-science-in-medicine-barbara-fadem-2nd/chapter-16/somatic-symptom-formaly. Accessed March 10th, 2014.
Illness Anxiety Disorder
- On the left hand side of the flowchart below, disorders previously included in the DSM-IV code of somatoform disorder are listed. DSM-V has simplified its definition by placing these disorders into one of two groups, IAD (illness anxiety disorder) or Somatic Symptom disorder. This will help medical professionals in differentiating IAD and SSD.
- Somatic symptom disorder includes somatization disorder, undifferentiated somatoform disorder, pain disorders and hypochondriasis with somatic symptoms. Hypochondriasis without somatic symptoms is not considered under the realm of SSD and is considered an illness anxiety disorder.
Dimsdale J, Creed F, Levenson J, et al. Somatic Symptom Disorder: An important change in DSM. Journal Of Psychosomatic Research [serial online]. September 2013;75(3):223-228. Available from: PsycINFO, Ipswich, MA. Accessed March 7, 2014.
Case Reports/ Case Studies[edit | edit source]
add links to case studies here (case studies should be added on new pages using the case study template)
Resources
[edit | edit source]
add appropriate resources here
Recent Related Research (from Pubmed)[edit | edit source]
see tutorial on Adding PubMed Feed
Extension:RSS -- Error: Not a valid URL: addfeedhere|charset=UTF-8|short|max=10
References[edit | edit source]
see adding references tutorial.