Role of Electrodiagnosis in Ulnar Nerve Entrapments
Anatomy of Ulnar Nerve[edit | edit source]
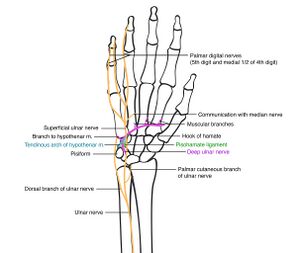
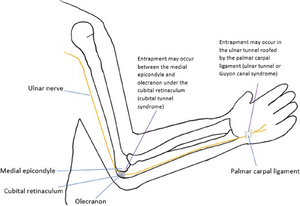
Ulnar nerve is the continuation of Medial Cord of Brachial Plexus (C8-T1). It passes in the arm medial to brachial artery . It then enters cubital tunnel and enters the forearm. It supplies Flexor Carpi Ulnaris (FCU) and Flexor Digitorum Profundus (FDP) for ring and little finger. It enters the wrist from Guyon's canal where it divides into Deep Motor branch which supplies Abductor Digiti Minimi (ADM), third and fourth Lumbrical, Interossei, Deep head of Flexor Pollicis Brevis (FPB) and Adductor Pollicis and a Superficial Sensory branch which gives sensory innervation to ulnar border of the ring finger and little finger [1]. Two sensory nerves arise from the Ulnar nerve in the forearm - Dorsal Ulnar Cutaneous Nerve which provides sensory innervation to the dorsal aspect the medial one and a half fingers and the associated dorsal hand area and a Palmar cutaneous nerve that provides innervation to the medial half of the hand.
Entrapment of Ulnar Nerve[edit | edit source]
Ulnar nerve entrapments are the second most common entrapment in Upper extremity after Median Nerve entrapment at Carpal Tunnel. Common causes include pregnancy, diabetes, occupations including repetitive elbow and wrist movements, acute trauma, iatrogenic injuries, cycling, and other recreational sports [3].Ulnar Nerve entrapments mostly occurs at two sites
- Ulnar Nerve Entrapment in Cubital Tunnel - This is an entrapment of the nerve in the cubital tunnel and occurs mainly due to compression by Osborne's ligament[1], larger coronoid process in men with lesser subcutaneous fats around it compared to women makes them more vulnerable to entrapment compared to women[4],and trauma.
- Ulnar Nerve Entrapment in Guyon's Canal - Compression of Ulnar nerve at wrist occurs in Guyon's Canal mainly due to occupations involving repetitive wrist movements and cycling activities apart from trauma. Guyon's canal is divided into three zones. Zone 1 lies proximal to the bifurcation of the nerve into Deep Palmar branch and Superficial Sensory branch. Zone 2 lies distal to zone 1 and surrounds motor branch. Zone 3 is distal to zone 2 and it surrounds only the sensory branch[1]
Clinical Presentation of Ulnar Nerve Entrapments[edit | edit source]
Patients usually present with paresthesia and sensory affection in the ring and little finger, hypothenar eminence, dorsal aspect of ulnar sensory supply of hand and ill-defined pain in the region of medial aspect of elbow. With advancing compression, intrinsic muscle weakness causing weak grip, decreased pinch strength, fatigue, clumsiness of the hand, and difficulty with fine motor tasks such as opening bottles or buttoning will be seen. More chronic conditions may lead to marked wasting of the small muscles of the hand and forearm muscles supplied by Ulnar nerve[3]Depending upon the site of compression, clinical presentation may vary. At elbow lesions, patient may present with sensory affection over dorsal hand and hypothenar region whereas this will be spared if the lesion is at wrist. Elbow lesions may present with weakness of FCU and FDP which will be spared in wrist lesions.
Looking at the fascicular arrangement of nerve fiber's, it is seen that FCU and FDP are relatively spared as their nerve fibers occupy deeper intraneural location where as the first dorsal interossei show preferential involvement. Due to the deeper location of intraneural fibers, there is relative sparing of Dorsal Ulnar Cutaneous nerve as well[6]
Role of Electrodiagnosis[edit | edit source]
Before proceeding for electrodiagnostic testing, it is imperative to do a thorough clinical assessment of the patient and establish differential diagnosis which can aid determining electrodiagnostic protocol. After a detailed assessment and looking at other investigations in a patient having sensory problem along the course of Ulnar Nerve, and weakness of Ulnar nerve supplied muscles, following differential diagnosis can be possible:
- Ulnar Nerve entrapment/lesion at wrist
- Ulnar Nerve entrapment / lesion at elbow
- Thoracic Outlet Syndrome
- C8-T1 root Cervical Radiculopathy
- Peripheral Neuropathy
Electrodiagnostic testing protocol should be decided based on these probabilities.
Electrodiagnostic testing should be able to give following conclusions[7]:
- Exact level of entrapment / lesion
- Type of nerve injury - Axonal, Demyelinating, Mixed, Conduction Block
- If there is presence of Axonal injury, exact site of injury, timing, severity, and regeneration status of the nerve
Electrodiagnostic Tests to be performed[edit | edit source]
In a case of suspected Ulnar nerve entrapment, following Tests should be employed[7]
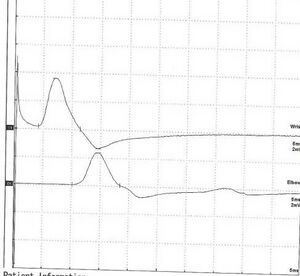
- Motor Nerve Conduction Study (MNCS / MNCV) -
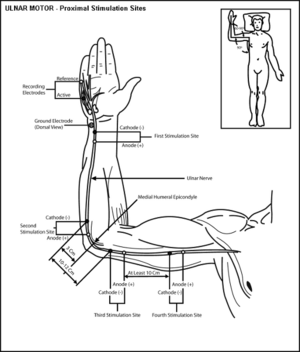
- Ulnar nerve MNCS for wrist to below elbow, below elbow to above elbow and above elbow to axilla components. If needed Ulnar nerve inching can be performed for across elbow in a suspected case of Cubital Tunnel Syndrome
- Apart from Standard Ulnar nerve MNCS (by recording from Abductor Digiti Minimi), MNCS of Ulnar nerve with recording from First Dorsal Interossie (FDI should also be performed due to preferential involvement of FDI in Ulnar nerve injuries.
- Median nerve MNCS for wrist to elbow and elbow to axilla component. This is done to rule out any other general form of neural affections.
- Sensory Nerve Conduction Study (SNCS / SNC) -
- Ulnar SNCS for Superficial Sensory branch
- Dorsal Ulnar Cutaneous Nerve (DUC) - to rule in/out Entrapment at elbow
- Medial Antebrachial Cutaneous Nerve - to rule in / out Thoracic Outlet Syndrome
- Median SNCS to rule out other ailments
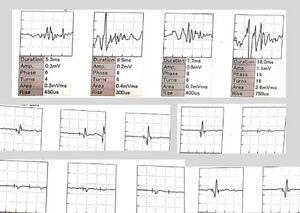
- Electromyography (EMG) studies - In case of a suspected axonal degeneration, EMG studies play a vital role in understanding nature, severity and timings of the lesion. It helps in understanding prognosis of the lesion by knowing the level and extent of nerve regeneration. It also plays important role in ruling out other differential diagnosis other than Ulnar nerve injuries. Following muscles should be sampled :
- Ulnar supplied muscles like FDP for ring and little finger, ADM, FDI
- Median supplied hand muscle like Abductor Pollices Brevis (APB) - This is done to rule out more proximal lesion like cervical radiculopathy or generalized brachial plexopathy.
- At least one muscle with C7 myotome to rule out Cervical lesion. If this is found affected, Ulnar nerve is ruled out and more proximal lesion is established which will need further testing.
- Lower Cervical Paraspinal Muscles this is done if tested muscles other than Ulnar nerve muscles are found affected and the diagnosis favors Cervical radiculopathy or Anterior Horn Cell lesion
Interpretation of Electrodiagnostic testing[edit | edit source]
Entrapment syndrome are mostly chronic compression injuries, many a times as a result of some offending factor. Histopathology of a nerve in chronic compression presents with breakdown in the blood–nerve barrier, which over time can cause subperineural edema. This can cause initially segmental demyelination which may progress to diffuse demyelination, and finally axonal loss[9].
In the initial stage, there is dynamic ischemia which means symptoms are position-dependent. Here in certain positions, there will be a decrease in perfusion of Ulnar nerve and it resolves when the position is changed. Electrodiagnostic findings will be normal in such cases. This is because fastest-conducting nerve fibers remain unaffected at this juncture[9].
A more severe form of compression or advanced stage will cause prolonged ischemia leading to demyelination of Ulnar nerve at the affected segment. Nerve conduction velocity will be slowed in such cases.[9]
- MNCV studies of Ulnar nerve will show prolonged distal motor latency (latency of the nerve at wrist) with reduced or normal nerve conduction velocity if the compression / entrapment is at Guyon's canal.
- If the affection is at the elbow, distal motor latency will be normal. MNCV studies will show normal conduction velocity wrist to below elbow. But there will be reduced nerve conduction velocity of Ulnar nerve across elbow i.e. below elbow to above elbow.
- Normal SNCS of Dorsal Ulnar Cutaneous nerve (DUC) favors entrapment at wrist. In the lesion at cubital tunnel, DUC SNCS may show reduced Sensory Nerve Action Potential (SNAP) amplitude compared to other side or in many instances, SNAP will not be elicited.
Long standing or severe compression will ultimately lead to axonal degeneration of Ulnar nerve[9]
- Amplitude in a Compound Motor Axonal Potential (CMAP) or SNAP represents the number of physiologically intact axons of the nerve being tested. In cases where axonal degeneration has set in, there will be a reduction in CMAP amplitude. A reduction of amplitude by 50% compared to the normal side is considered significant[7].
- Patient may present with Conduction block where apart from demyelination, there will be a reduction in CMAP amplitude by 20% or more in the affected region and proximal to the area of affection[7]. CMAP amplitude will be normal distal to the level of lesion.
- Incases where axonal loss is suspected, needle EMG will prove to be conclusive. Presence of Fibrillation Potentials and Positive Sharp waves in Ulnar supplied muscles suggest acute axonal degeneration. On Voluntary activity, presence of long duration polyphasic motor unit action potentials (MUAP) suggest signs of regeneration and more chronic nature of injury. If these signs are present in FCU and FDP along with hand muscles, the lesion is at elbow. If needle EMG of FPD is normal and hand muscles present with EMG findings of axonal degeneration or regeneration, the lesion is at elbow.
Summary of Electrodiagnostic differentiating findings[edit | edit source]
| Ulnar Nerve Compression
Wrist |
Ulnar Nerve compression
Elbow |
MEDIAL CORD of Brachial Plexus Injury | LOWER TRUNK of Brachial Plexus Injury | Radiculopathy affecting ROOTS
(C8-T1) | |
| Nerve Conduction Studies | |||||
| ULNAR DIGIT 5 SNAP | Affected | Affected | Affected | Affected | |
| DORSAL ULNAR CUTANEOUS SNAP | Affected | Affected | Affected | ||
| MEDIAL ANTEBRACHIAL CUTANEOUS SNAP | Affected | Affected | |||
| LOW ULNAR CMAP amplitude | Yes | Yes | Yes | Yes | Not always |
| CONDUCTION BLOCK ACROSS ELBOW | Yes | ||||
| EMG Abnormalities | |||||
| FDI | Present | Present | Present | Present | Present |
| ADQ | Present | Present | Present | Present | Present |
| FDP (4,5th) | Present | Present | Present | Present | |
| FCU | Present | Present | Present | Present | |
| APB | Present | Present | Present | ||
| Extensor Indices | Present | Present | |||
| CERVICAL PARASPINAL MUSCLES | Present | ||||
Anomalous innervations among the nerves are very common especially between Median and Ulnar nerves. Martin Gruber Anastomosis is an anomalous innervation of Median nerve to Ulnar supplied hand muscles and this anastomosis takes place in the forearm. It is estimated that approximately 17 % population have this. Riche Cannieu Anastomosis is an anomalous innervation of Ulnar nerve to Median supplied hand muscles. In presence of such anomalous innervation, more care and attention are needed while performing and interpreting electrodiagnostic tests[6].
Resources[edit | edit source]
References[edit | edit source]
- ↑ 1.0 1.1 1.2 Davis DD, Kane SM. Ulnar Nerve Entrapment.2020
- ↑ https://commons.wikimedia.org/wiki/Category:Ulnar_nerves#/media/File:Branches_of_the_ulnar_nerve_in_hand.jpg
- ↑ 3.0 3.1 Vij N, Traube B, Bisht R, Singleton I, Cornett EM, Kaye AD, Imani F, Erdi AM, Varrassi G, Viswanath O, Urits I. An update on treatment modalities for ulnar nerve entrapment: a literature review. Anesthesiology and Pain Medicine. 2020 Dec;10(6).
- ↑ Contreras MG, Warner MA, Charboneau WJ, Cahill DR. Anatomy of the ulnar nerve at the elbow: potential relationship of acute ulnar neuropathy to gender differences. Clinical Anatomy: The Official Journal of the American Association of Clinical Anatomists and the British Association of Clinical Anatomists. 1998;11(6):372-8.
- ↑ https://commons.wikimedia.org/wiki/File:The_ulnar_nerve_is_shown._The_most_common_entrapment_neuropathies_of_the_ulnar_nerve_are_the_cubital_tunnel_syndrome_at_the_elbow,_and_the_ulnar_tunnel_syndrome_at_the_wrist.webp
- ↑ 6.0 6.1 Kern RZ. The electrodiagnosis of ulnar nerve entrapment at the elbow. Canadian journal of neurological sciences. 2003 Nov;30(4):314-9.
- ↑ 7.0 7.1 7.2 7.3 Preston DC, Shapiro BE. Electromyography and neuromuscular disorders e-book: clinical-electrophysiologic correlations (Expert Consult-Online). Elsevier Health Sciences; 2012 Dec 1.
- ↑ https://plusqueen.tistory.com/8
- ↑ 9.0 9.1 9.2 9.3 Dy CJ, Mackinnon SE. Ulnar neuropathy: evaluation and management. Current reviews in musculoskeletal medicine. 2016 Jun;9:178-84.