Purpura: Difference between revisions
Kylie Smith (talk | contribs) No edit summary |
Kim Jackson (talk | contribs) No edit summary |
||
| (34 intermediate revisions by 4 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> '''Original Editor '''- [[User:Elaine Lonnemann |Elaine Lonnemann ]] '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> | |||
'''Original | |||
== Definition/Description<br> == | |||
== Definition/Description == | |||
[[Image:ITP-1.jpg|border|alt=|right]] | |||
Idiopathic thrombocytopenic purpura (ITP), also known as primary immune thrombocytopenic purpura and autoimmune thrombocytopenic purpura, is defined as isolated thrombocytopenia with normal bone marrow and in the absence of other causes of thrombocytopenia. ITP has two distinct clinical syndromes, with typical manifestation of an acute condition in children (spontaneous resolution within 2 months) and a chronic condition in adults (lasting longer than 6 months)<ref name="Medscape">Medscape [Internet]. WebMD LLC; 1994. Idiopathic Thrombocytopenic Purpura; 2016 July 22. [cited 2017 Mar 27]; [about 8 screens]. Available from: http://emedicine.medscape.com/article/779545-overview#a6</ref | Purpura is a hemorrhagic condition that occurs when not enough normal platelets are available to plug damaged vessels or prevent leakage from even minor injury to normal capillaries. Purpura is characterized by movement of blood into the surrounding tissue (extravasation), under the [[skin]], and through mucous membranes, producing spontaneous ecchymoses (bruises) and petechiae (small, red patches) on the skin<ref name="Patho Book">Goodman CC, Fuller KS. Pathology: Implications for the Physical Therapist. 4th ed. St. Louis: Elsevier Saunders; 2015.</ref>. Purpura measure between 4 and 10 mm (millimeters) in diameter. When purpura spots are less than 4 mm in diameter, they are called petechiae. Purpura spots larger than 1 cm (centimeter) are called ecchymoses<ref name="Medline">MedlinePlus medical encyclopedia [Internet]. Atlanta (GA): A.D.A.M., Inc.; c2017. Purpura; [updated 2015 April 14]; [1screen] Available from: https://medlineplus.gov/ency/article/003232.htm</ref>. There are many different types of purpura. Their classification depends on the appearance or cause of the condition. | ||
[[Image:Idiopathic-Thrombocytopenic-Purpura.gif|border|right|350x250px]]Idiopathic thrombocytopenic purpura (ITP), also known as primary immune thrombocytopenic purpura and [[Autoimmune Disorders|autoimmune]] thrombocytopenic purpura, is defined as isolated thrombocytopenia with normal [[Bone Marrow|bone marrow]] and in the absence of other causes of thrombocytopenia. ITP has two distinct clinical syndromes, with typical manifestation of an acute condition in children (spontaneous resolution within 2 months) and a chronic condition in adults (lasting longer than 6 months)<ref name="Medscape">Medscape [Internet]. WebMD LLC; 1994. Idiopathic Thrombocytopenic Purpura; 2016 July 22. [cited 2017 Mar 27]; [about 8 screens]. Available from: http://emedicine.medscape.com/article/779545-overview#a6</ref> | |||
== Prevalence == | == Prevalence == | ||
Frequency | |||
*The incidence of ITP in adults is approximately 66 cases per 1,000,000 per year | *The incidence of ITP in adults is approximately 66 cases per 1,000,000 per year | ||
*An average estimate of the incidence in children is 50 cases per 1,000,000 per year<ref name="Medscape" />. | *An average estimate of the incidence in children is 50 cases per 1,000,000 per year<ref name="Medscape" />. | ||
<u> | <u>Ag</u>e | ||
*Peak prevalence occurs in adults aged 20-50 years. | *Peak prevalence occurs in adults aged 20-50 years. | ||
*Peak prevalence occurs in children aged 2-4 years. | *Peak prevalence occurs in children aged 2-4 years. | ||
*Approximately 40% of all patients are younger than 10 years<ref name="Medscape" />. | *Approximately 40% of all patients are younger than 10 years<ref name="Medscape" />. <br> | ||
== Characteristics/Clinical Presentation == | == Characteristics/Clinical Presentation == | ||
[[Image:Itp1.jpg|right|250x250px|alt=|frameless]] | |||
Physical signs and symptoms include: | Physical signs and symptoms include: | ||
*Easy or excessive bruising (purpura) | *Easy or excessive bruising (purpura) | ||
*Superficial bleeding into the skin that appears as a rash of pinpoint-sized reddish-purple spots (petechiae), usually on the lower legs | *Superficial bleeding into the skin that appears as a rash of pinpoint-sized reddish-purple spots (petechiae), usually on the lower legs | ||
*Bleeding from the gums or nose | *Bleeding from the gums or nose | ||
*Blood in urine or stools | *Blood in urine or stools | ||
*Unusually heavy menstrual flow <ref name="Mayo Clinic">Mayo Clinic [Internet]. Mayo Foundation for Medical Education and Research (MFMER); 1998. Idiopathic thrombocytopenic purpura (ITP) [Internet]. 2016 April 23. [cited 2017Mar27]. [about 8 screens]. Available from: http://www.mayoclinic.org/diseases-conditions/idiopathic-thrombocytopenic-purpura/home/ovc-20201208</ref> | *Unusually heavy menstrual flow <ref name="Mayo Clinic">Mayo Clinic [Internet]. Mayo Foundation for Medical Education and Research (MFMER); 1998. Idiopathic thrombocytopenic purpura (ITP) [Internet]. 2016 April 23. [cited 2017Mar27]. [about 8 screens]. Available from: http://www.mayoclinic.org/diseases-conditions/idiopathic-thrombocytopenic-purpura/home/ovc-20201208</ref> | ||
*Non-blanchable lesions <ref name="Leung">Leung AKC, Chan KW. Evaluating the Child with Purpura [Internet]. American Family Physician; 2001 Aug 01 [cited 2017 Mar 27]; 64(3): 419-428. Available from: http://www.aafp.org/afp/2001/0801/p419.html#afp20010801p419-b9</ref> | *Non-blanchable lesions <ref name="Leung">Leung AKC, Chan KW. Evaluating the Child with Purpura [Internet]. American Family Physician; 2001 Aug 01 [cited 2017 Mar 27]; 64(3): 419-428. Available from: http://www.aafp.org/afp/2001/0801/p419.html#afp20010801p419-b9</ref> | ||
Idiopathic thrombocytopenic purpura can occur in anyone at almost any age, but these factors increase the risk: <ref name="Mayo Clinic" /> | Idiopathic thrombocytopenic purpura can occur in anyone at almost any age, but these factors increase the risk: <ref name="Mayo Clinic" /> | ||
*'''Your sex.''' Women are two to three times more likely to develop ITP than men are. | *'''Your sex.''' Women are two to three times more likely to develop ITP than men are. | ||
*'''Recent viral infection.''' Many children with ITP develop the disorder after a viral illness, such as mumps, measles, influenza or a respiratory infection. | *'''Recent viral infection.''' Many children with ITP develop the disorder after a viral illness, such as mumps, measles, influenza or a respiratory infection.<br> | ||
== Associated Co-morbidities == | == Associated Co-morbidities == | ||
ITP is associated with a considerable number of medical conditions including hematological diseases, dermatological conditions, oral conditions, viral infections (such as Hepatitis C, HIV, measles, and mumps), gastrointestinal, bleeding, and autoimmune disorders. One possible cause of associated signs and symptoms could be due to an adverse drug reaction. However, further research is needed to identify the cause and extent of the association between these conditions and ITP <ref name="Feudjo">Feudjo-Tepie MA, Le Roux G, Beach KJ, Bennett D, and Robinson NJ. Comorbidities of Idiopathic Thrombocytopenic Purpura: A Population-Based Study. Advances in Hematology [Internet]. 2009 [cited 2017 March 27]; 2009. Available from: https://www.hindawi.com/journals/ah/2009/963506/ DOI:10.1155/2009/963506</ref><ref name="Neunert">Neunert C, Lim W, Cohen A, Solberg L, Crowther M. The American Society of Hematology 2011 evidence-based practice guideline for immune thrombocytopenia. BLOOD [Internet]. 2011 April 21 [cited 2017 March 27]; 117(16): 4190-4207. Available from: http://www.bloodjournal.org/content/bloodjournal/117/16/4190.full.pdf</ref | ITP is associated with a considerable number of medical conditions including hematological diseases, dermatological conditions, oral conditions, viral infections (such as Hepatitis C, HIV, measles, and mumps), gastrointestinal, bleeding, and autoimmune disorders. One possible cause of associated signs and symptoms could be due to an adverse drug reaction. However, further research is needed to identify the cause and extent of the association between these conditions and ITP <ref name="Feudjo">Feudjo-Tepie MA, Le Roux G, Beach KJ, Bennett D, and Robinson NJ. Comorbidities of Idiopathic Thrombocytopenic Purpura: A Population-Based Study. Advances in Hematology [Internet]. 2009 [cited 2017 March 27]; 2009. Available from: https://www.hindawi.com/journals/ah/2009/963506/ DOI:10.1155/2009/963506</ref><ref name="Neunert">Neunert C, Lim W, Cohen A, Solberg L, Crowther M. The American Society of Hematology 2011 evidence-based practice guideline for immune thrombocytopenia. BLOOD [Internet]. 2011 April 21 [cited 2017 March 27]; 117(16): 4190-4207. Available from: http://www.bloodjournal.org/content/bloodjournal/117/16/4190.full.pdf</ref> | ||
== Medications == | == Medications == | ||
A detailed description of The American Society of Hematology 2011 evidence-based practice guideline for immune thrombocytopenia can be viewed here<ref name="Neunert" />: | A detailed description of The American Society of Hematology 2011 evidence-based practice guideline for immune thrombocytopenia can be viewed here<ref name="Neunert" />: | ||
http://www.bloodjournal.org/content/117/16/4190?sso-checked=true | http://www.bloodjournal.org/content/117/16/4190?sso-checked=true | ||
The primary focus of a pharmaceutical approach to the treatment of ITP is to raise the individual’s platelet count. They may also be asked to stop taking medications that impair platelet function, such as aspirin, blood thinners, and ibuprofen <ref name="Healthline">Healthline [Internet]. Healthline Media; 2005. Purpura; 2016 June 30. [cited 2017 Mar 27]; [about 6 screens]. Available from: http://www.healthline.com/health/purpura?s_con_rec=false&r=0#Overview1</ref>. | The primary focus of a pharmaceutical approach to the treatment of ITP is to raise the individual’s platelet count. They may also be asked to stop taking medications that impair platelet function, such as aspirin, blood thinners, and ibuprofen <ref name="Healthline">Healthline [Internet]. Healthline Media; 2005. Purpura; 2016 June 30. [cited 2017 Mar 27]; [about 6 screens]. Available from: http://www.healthline.com/health/purpura?s_con_rec=false&r=0#Overview1</ref>. | ||
Corticosteroids: The doctor may start with a corticosteroid medication, which can help increase the platelet count by decreasing the activity of the immune system. It usually takes about two to six weeks for their platelet count to return to a safe level. When it does, the doctor will discontinue the drug<ref name="Healthline" />.<br>Intravenous immunoglobulin: If your purpura is causing severe bleeding, your doctor may give you an intravenous medication called intravenous immunoglobulin (IVIG). They may also give you IVIG if you need to increase your platelet count rapidly before surgery. This treatment is usually effective in increasing your platelet count, but the effect is usually only in the short term. It can cause side effects such as headache, nausea, and fever <ref name="Healthline" />.<br>Other drug therapies: The latest drugs used to treat purpura are romiplostim (Nplate) and eltrombopag (Promacta). These medications cause bone marrow to produce more platelets, which reduces the risk of bruising and bleeding. Potential side effects include: | |||
*headaches | *headaches | ||
*dizziness | *dizziness | ||
| Line 70: | Line 58: | ||
*increased risk of blood clots | *increased risk of blood clots | ||
*acute respiratory distress syndrome | *acute respiratory distress syndrome | ||
Biologic therapy, such as the drug rituximad (Rituxan), can help decrease the immune system response. It’s mostly used to treat patients with severe thrombocyotopenic purpura and patients for whom corticosteroid treatment isn’t effective. Side effects may include: | Biologic therapy, such as the drug rituximad (Rituxan), can help decrease the immune system response. It’s mostly used to treat patients with severe thrombocyotopenic purpura and patients for whom corticosteroid treatment isn’t effective. Side effects may include: | ||
| Line 78: | Line 63: | ||
*sore throat | *sore throat | ||
*rash | *rash | ||
*fever <ref name="Healthline" / | *fever <ref name="Healthline" /> | ||
== Diagnostic Tests/Lab Tests/Lab Values == | == Diagnostic Tests/Lab Tests/Lab Values == | ||
| Line 94: | Line 79: | ||
In people with ITP, an unknown cause leads antibodies produced by the immune system to attach themselves to the platelets, marking the platelets for destruction. The spleen, which helps the body fight infection, recognizes the antibodies and removes the platelets from your system. The result of this case of mistaken identity is a lower number of circulating platelets than is normal.<br> | In people with ITP, an unknown cause leads antibodies produced by the immune system to attach themselves to the platelets, marking the platelets for destruction. The spleen, which helps the body fight infection, recognizes the antibodies and removes the platelets from your system. The result of this case of mistaken identity is a lower number of circulating platelets than is normal.<br> | ||
A normal platelet count is generally between 150,000 and 450,000 platelets per microliter of circulating blood. People with ITP often have platelet counts below 20,000. Because platelets help the blood clot, as their number decreases, your risk of bleeding increases. The greatest risk is when your platelet count falls very low — below 10,000 platelets per microliter. At this point, internal bleeding may occur even without any injury<ref name="Mayo Clinic" />. Older patients have more severe and rare bleeding manifestations, such as GI bleeding and possibly intracranial hemorrhage secondary to co-morbidities such as hypertension<ref name="Kayal">Kayal L, Jayachandran S, Singh K. Idiopathic thrombocytopenic purpura. Contemp Clin Dent [serial online] 2014 [cited 2017 Mar 27];5:410-4. Available from: http://www.contempclindent.org/text.asp?2014/5/3/410/137976</ref>.<br><br> | A normal platelet count is generally between 150,000 and 450,000 platelets per microliter of circulating blood. People with ITP often have platelet counts below 20,000. Because platelets help the blood clot, as their number decreases, your risk of bleeding increases. The greatest risk is when your platelet count falls very low — below 10,000 platelets per microliter. At this point, internal bleeding may occur even without any injury<ref name="Mayo Clinic" />. Older patients have more severe and rare bleeding manifestations, such as GI bleeding and possibly intracranial hemorrhage secondary to co-morbidities such as hypertension<ref name="Kayal">Kayal L, Jayachandran S, Singh K. Idiopathic thrombocytopenic purpura. Contemp Clin Dent [serial online] 2014 [cited 2017 Mar 27];5:410-4. Available from: http://www.contempclindent.org/text.asp?2014/5/3/410/137976</ref>.[[Image:Abd296dd0943bdd3a5eff3780c5634c5.jpg|center|600x300px]]<br>Image Available from: www.nplate.com<br> | ||
== Systemic Involvement == | == Systemic Involvement == | ||
ITP directly affects the dermatologic and hematologic systems. It does not directly have any other systemic involvement. However, the section above titled "Associated Co-morbidities" includes some of the co-morbidities associated with ITP that may have systemic involvement including the gastrointestinal or endocrine systems. | |||
== Medical Management | == Medical Management == | ||
Treatments include medications and sometimes a splenectomy to remove the spleen. | Treatments include medications and sometimes a splenectomy to remove the spleen. | ||
| Line 106: | Line 91: | ||
See above section titled "Medications". | See above section titled "Medications". | ||
<u>Splenectomy</u> | <u>Splenectomy:</u> If medications aren’t effective in treating your purpura, your doctor may recommend a splenectomy. Removing the spleen is a fast way of increasing your platelet count. This is because the spleen is the main body part responsible for eliminating platelets. | ||
{{#ev:youtube|w82Tivwc1dE}}<ref>Platelet Disorder Support Association. What are the Challenges of Treating and Managing ITP? [web streaming video].Youtube, 2008 December 17 [cited 2017 March 27]. Available from: https://www.youtube.com/watch?v=w82Tivwc1dE </ref> | |||
== Physical Therapy Management | == Physical Therapy Management == | ||
Physical therapists are not able to treat or diagnose idiopathic thrombocytopenic purpura, but are able to recognize differences in skin pigmentation and can refer the patient to a suitable specialist. | Physical therapists are not able to treat or diagnose idiopathic thrombocytopenic purpura, but are able to recognize differences in skin pigmentation and can refer the patient to a suitable specialist. | ||
If you are cleared through a physician to treat associated impairments such as general weakness, | If you are cleared through a physician to treat associated impairments such as general weakness, it is recommended that low-impact activities be performed over high-impact activities. Patients can have increased risk of injury, bruising, and bleeding<ref name="Healthline" />. | ||
== Differential Diagnosis == | == Differential Diagnosis == | ||
| Line 120: | Line 105: | ||
Other differential diagnoses for ITP include disorders such as: | Other differential diagnoses for ITP include disorders such as: | ||
* | *Autoimmune disorders: SLE, antiphospholipid antibody syndrome | ||
* | *Infections: HIV, HCV, EBV | ||
* | *Neoplastic: CLL, lymphoma, large granular lymphocytic leukemia, | ||
* | *MDS Drug effect: Heparin, quinidine, sulfa, gold | ||
* | *Hypersplenism | ||
* | *Isolated thrombocytopenia of pregnancy | ||
* | *Congenital (Wiskott-Aldrich, Bernard-Soulier, Fanconi’s anemia, etc) | ||
* | *Rare: Pure megakaryocyte aplasia <ref name="UCSF">University of California San Francisco Department of Medicine [Internet]. San Francisco: The Regents of the University of California; 2017. Idiopathic Thrombocytopenic Purpura; 2003 December [2017 March 27]; [2 pages]. Available from: https://medicine.ucsf.edu/education/resed/Chiefs_cover_sheets/itp_update.pdf</ref> | ||
== Case Reports/ Case Studies == | == Case Reports/ Case Studies == | ||
{{#ev:youtube|qm6-rU_Hunk}}<ref>Mayo Clinic. Jude’s Story: A Toddlers Battle with ITP [web streaming video]. Youtube, 2014 September 24 [cited 2017 March 27]. Available from: https://www.youtube.com/watch?v=qm6-rU_Hunk </ref> | |||
== References == | == References == | ||
Latest revision as of 16:49, 14 October 2021
Definition/Description
[edit | edit source]
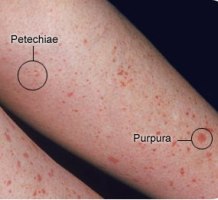
Purpura is a hemorrhagic condition that occurs when not enough normal platelets are available to plug damaged vessels or prevent leakage from even minor injury to normal capillaries. Purpura is characterized by movement of blood into the surrounding tissue (extravasation), under the skin, and through mucous membranes, producing spontaneous ecchymoses (bruises) and petechiae (small, red patches) on the skin[1]. Purpura measure between 4 and 10 mm (millimeters) in diameter. When purpura spots are less than 4 mm in diameter, they are called petechiae. Purpura spots larger than 1 cm (centimeter) are called ecchymoses[2]. There are many different types of purpura. Their classification depends on the appearance or cause of the condition.
Idiopathic thrombocytopenic purpura (ITP), also known as primary immune thrombocytopenic purpura and autoimmune thrombocytopenic purpura, is defined as isolated thrombocytopenia with normal bone marrow and in the absence of other causes of thrombocytopenia. ITP has two distinct clinical syndromes, with typical manifestation of an acute condition in children (spontaneous resolution within 2 months) and a chronic condition in adults (lasting longer than 6 months)[3]
Prevalence[edit | edit source]
Frequency
- The incidence of ITP in adults is approximately 66 cases per 1,000,000 per year
- An average estimate of the incidence in children is 50 cases per 1,000,000 per year[3].
Age
- Peak prevalence occurs in adults aged 20-50 years.
- Peak prevalence occurs in children aged 2-4 years.
- Approximately 40% of all patients are younger than 10 years[3].
Characteristics/Clinical Presentation[edit | edit source]
Physical signs and symptoms include:
- Easy or excessive bruising (purpura)
- Superficial bleeding into the skin that appears as a rash of pinpoint-sized reddish-purple spots (petechiae), usually on the lower legs
- Bleeding from the gums or nose
- Blood in urine or stools
- Unusually heavy menstrual flow [4]
- Non-blanchable lesions [5]
Idiopathic thrombocytopenic purpura can occur in anyone at almost any age, but these factors increase the risk: [4]
- Your sex. Women are two to three times more likely to develop ITP than men are.
- Recent viral infection. Many children with ITP develop the disorder after a viral illness, such as mumps, measles, influenza or a respiratory infection.
Associated Co-morbidities[edit | edit source]
ITP is associated with a considerable number of medical conditions including hematological diseases, dermatological conditions, oral conditions, viral infections (such as Hepatitis C, HIV, measles, and mumps), gastrointestinal, bleeding, and autoimmune disorders. One possible cause of associated signs and symptoms could be due to an adverse drug reaction. However, further research is needed to identify the cause and extent of the association between these conditions and ITP [6][7]
Medications[edit | edit source]
A detailed description of The American Society of Hematology 2011 evidence-based practice guideline for immune thrombocytopenia can be viewed here[7]:
http://www.bloodjournal.org/content/117/16/4190?sso-checked=true
The primary focus of a pharmaceutical approach to the treatment of ITP is to raise the individual’s platelet count. They may also be asked to stop taking medications that impair platelet function, such as aspirin, blood thinners, and ibuprofen [8].
Corticosteroids: The doctor may start with a corticosteroid medication, which can help increase the platelet count by decreasing the activity of the immune system. It usually takes about two to six weeks for their platelet count to return to a safe level. When it does, the doctor will discontinue the drug[8].
Intravenous immunoglobulin: If your purpura is causing severe bleeding, your doctor may give you an intravenous medication called intravenous immunoglobulin (IVIG). They may also give you IVIG if you need to increase your platelet count rapidly before surgery. This treatment is usually effective in increasing your platelet count, but the effect is usually only in the short term. It can cause side effects such as headache, nausea, and fever [8].
Other drug therapies: The latest drugs used to treat purpura are romiplostim (Nplate) and eltrombopag (Promacta). These medications cause bone marrow to produce more platelets, which reduces the risk of bruising and bleeding. Potential side effects include:
- headaches
- dizziness
- nausea
- joint or muscle pain
- vomiting
- increased risk of blood clots
- acute respiratory distress syndrome
Biologic therapy, such as the drug rituximad (Rituxan), can help decrease the immune system response. It’s mostly used to treat patients with severe thrombocyotopenic purpura and patients for whom corticosteroid treatment isn’t effective. Side effects may include:
- low blood pressure
- sore throat
- rash
- fever [8]
Diagnostic Tests/Lab Tests/Lab Values[edit | edit source]
Frequently, the diagnosis can be established on the basis of a careful history and physical examination, and a few key laboratory tests. Indicated tests include a complete blood cell count with platelet count, a peripheral blood smear, and prothrombin and activated partial thromboplastin times [5]
- A complete blood count. This test checks the number of red blood cells, white blood cells, and platelets in your blood. In ITP, the red and white blood cell counts are normal, but the platelet count is low.
- A blood smear. For this test, some of your blood is put on a slide. A microscope is used to look at your platelets and other blood cells.
- Bone marrow exam. This test may be used to help identify the cause of a low platelet count, though the American Society of Hematology doesn't recommend this test for children with ITP [4][9]
Etiology/Causes[edit | edit source]
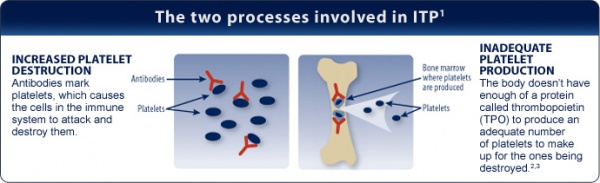
Thrombocytopenia can be caused by decreased production or increased destruction of platelets. Historically, ITP was believed to be caused by increased platelet destruction at a rate that exceeded production by a compensating bone marrow. However, new knowledge has questioned this model, providing evidence that platelet production is also decreased in many patients with ITP[7].
In people with ITP, an unknown cause leads antibodies produced by the immune system to attach themselves to the platelets, marking the platelets for destruction. The spleen, which helps the body fight infection, recognizes the antibodies and removes the platelets from your system. The result of this case of mistaken identity is a lower number of circulating platelets than is normal.
A normal platelet count is generally between 150,000 and 450,000 platelets per microliter of circulating blood. People with ITP often have platelet counts below 20,000. Because platelets help the blood clot, as their number decreases, your risk of bleeding increases. The greatest risk is when your platelet count falls very low — below 10,000 platelets per microliter. At this point, internal bleeding may occur even without any injury[4]. Older patients have more severe and rare bleeding manifestations, such as GI bleeding and possibly intracranial hemorrhage secondary to co-morbidities such as hypertension[10].
Image Available from: www.nplate.com
Systemic Involvement[edit | edit source]
ITP directly affects the dermatologic and hematologic systems. It does not directly have any other systemic involvement. However, the section above titled "Associated Co-morbidities" includes some of the co-morbidities associated with ITP that may have systemic involvement including the gastrointestinal or endocrine systems.
Medical Management[edit | edit source]
Treatments include medications and sometimes a splenectomy to remove the spleen.
See above section titled "Medications".
Splenectomy: If medications aren’t effective in treating your purpura, your doctor may recommend a splenectomy. Removing the spleen is a fast way of increasing your platelet count. This is because the spleen is the main body part responsible for eliminating platelets.
Physical Therapy Management[edit | edit source]
Physical therapists are not able to treat or diagnose idiopathic thrombocytopenic purpura, but are able to recognize differences in skin pigmentation and can refer the patient to a suitable specialist.
If you are cleared through a physician to treat associated impairments such as general weakness, it is recommended that low-impact activities be performed over high-impact activities. Patients can have increased risk of injury, bruising, and bleeding[8].
Differential Diagnosis[edit | edit source]
Other differential diagnoses for ITP include disorders such as:
- Autoimmune disorders: SLE, antiphospholipid antibody syndrome
- Infections: HIV, HCV, EBV
- Neoplastic: CLL, lymphoma, large granular lymphocytic leukemia,
- MDS Drug effect: Heparin, quinidine, sulfa, gold
- Hypersplenism
- Isolated thrombocytopenia of pregnancy
- Congenital (Wiskott-Aldrich, Bernard-Soulier, Fanconi’s anemia, etc)
- Rare: Pure megakaryocyte aplasia [12]
Case Reports/ Case Studies[edit | edit source]
References[edit | edit source]
see adding references tutorial.
- ↑ Goodman CC, Fuller KS. Pathology: Implications for the Physical Therapist. 4th ed. St. Louis: Elsevier Saunders; 2015.
- ↑ MedlinePlus medical encyclopedia [Internet]. Atlanta (GA): A.D.A.M., Inc.; c2017. Purpura; [updated 2015 April 14]; [1screen] Available from: https://medlineplus.gov/ency/article/003232.htm
- ↑ 3.0 3.1 3.2 Medscape [Internet]. WebMD LLC; 1994. Idiopathic Thrombocytopenic Purpura; 2016 July 22. [cited 2017 Mar 27]; [about 8 screens]. Available from: http://emedicine.medscape.com/article/779545-overview#a6
- ↑ 4.0 4.1 4.2 4.3 Mayo Clinic [Internet]. Mayo Foundation for Medical Education and Research (MFMER); 1998. Idiopathic thrombocytopenic purpura (ITP) [Internet]. 2016 April 23. [cited 2017Mar27]. [about 8 screens]. Available from: http://www.mayoclinic.org/diseases-conditions/idiopathic-thrombocytopenic-purpura/home/ovc-20201208
- ↑ 5.0 5.1 Leung AKC, Chan KW. Evaluating the Child with Purpura [Internet]. American Family Physician; 2001 Aug 01 [cited 2017 Mar 27]; 64(3): 419-428. Available from: http://www.aafp.org/afp/2001/0801/p419.html#afp20010801p419-b9
- ↑ Feudjo-Tepie MA, Le Roux G, Beach KJ, Bennett D, and Robinson NJ. Comorbidities of Idiopathic Thrombocytopenic Purpura: A Population-Based Study. Advances in Hematology [Internet]. 2009 [cited 2017 March 27]; 2009. Available from: https://www.hindawi.com/journals/ah/2009/963506/ DOI:10.1155/2009/963506
- ↑ 7.0 7.1 7.2 Neunert C, Lim W, Cohen A, Solberg L, Crowther M. The American Society of Hematology 2011 evidence-based practice guideline for immune thrombocytopenia. BLOOD [Internet]. 2011 April 21 [cited 2017 March 27]; 117(16): 4190-4207. Available from: http://www.bloodjournal.org/content/bloodjournal/117/16/4190.full.pdf
- ↑ 8.0 8.1 8.2 8.3 8.4 Healthline [Internet]. Healthline Media; 2005. Purpura; 2016 June 30. [cited 2017 Mar 27]; [about 6 screens]. Available from: http://www.healthline.com/health/purpura?s_con_rec=false&r=0#Overview1
- ↑ NHLBI [Internet]. National Institutes of Health; How is Immune Thrombocytopenia Diagnosed?; 2012 March 14. [cited 2017 March 27]; [1 screen]. Available from: https://www.nhlbi.nih.gov/health/health-topics/topics/itp/diagnosis
- ↑ Kayal L, Jayachandran S, Singh K. Idiopathic thrombocytopenic purpura. Contemp Clin Dent [serial online] 2014 [cited 2017 Mar 27];5:410-4. Available from: http://www.contempclindent.org/text.asp?2014/5/3/410/137976
- ↑ Platelet Disorder Support Association. What are the Challenges of Treating and Managing ITP? [web streaming video].Youtube, 2008 December 17 [cited 2017 March 27]. Available from: https://www.youtube.com/watch?v=w82Tivwc1dE
- ↑ University of California San Francisco Department of Medicine [Internet]. San Francisco: The Regents of the University of California; 2017. Idiopathic Thrombocytopenic Purpura; 2003 December [2017 March 27]; [2 pages]. Available from: https://medicine.ucsf.edu/education/resed/Chiefs_cover_sheets/itp_update.pdf
- ↑ Mayo Clinic. Jude’s Story: A Toddlers Battle with ITP [web streaming video]. Youtube, 2014 September 24 [cited 2017 March 27]. Available from: https://www.youtube.com/watch?v=qm6-rU_Hunk