Prosthetics for Individuals with Hip Disarticulation and Hemipelvectomy Amputations
Original Editor - Tarina van der Stockt
Top Contributors - Martina Lukin, Wanda van Niekerk, Kim Jackson, Tarina van der Stockt and Simisola Ajeyalemi
Introduction[edit | edit source]
Hip disarticulation (HD) and Hemipelvectomy (HP) are the most proximal amputations of the lower extremity. Although the two amputation levels are similar in appearance they feature important anatomical differences; Whilst a HD is performed directly through the hip joint, a HP includes removal of the entire hip joint along with a section of the pelvis on the same side[1].
Both HD and HP are very extensive amputations, most commonly performed due to malignant tumours[1]. Less frequently, they also performed following severe trauma, vascular disease (vascular insufficiency), femoral osteomyelitis and other factors [1]. Both levels are not common and account for less than 1% of all amputations [2][3].
Because of the extent of HD and HP amputations, they can significantly impact functional mobility and independence. Coupled with an increased likelihood of chronic pain and skin complications[2], individuals with these proximal amputation levels tend to experience the most difficulty in activities such as walking, rising and sitting down and climbing stairs[1][4].
Despite the challenges associated with rehabilitation, prosthetic fitting for HD and HP amputees should not be discouraged[5]. Modern advancements in prosthetic design have seen the development of lighter and more functional lower limb components, including some specifically designed for HD and HP prostheses. Socket designs have also evolved to incorporate more modern interface materials such as silicone, that conform more closely to the individual's anatomy thus providing improved fit and comfort for the prosthetic user. HD and HP Prostheses, particularly those incorporating modern designs and components, can help restore functional mobility to a higher level as well as benefit a more diverse demographic of amputees[5].
Requirements for successful prosthetic fitting[edit | edit source]
- Active pelvic lordosis
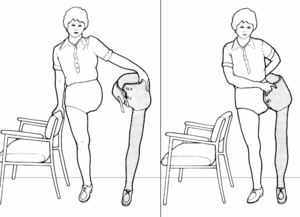
Due to the type of amputation, there is no residual limb left and thus no lever to control the prosthesis during gait. As a result, the main mechanism used by the prosthetic user to initiate knee flexion during gait is pelvic lordosis. To ensure successful prosthetic fitting, the prosthetic user must be able to achieve good lordotic range of motion through active use of the lower back and abdominal musculature[3].
- Single leg balance
Ability to balance on the sound leg is essential for the prosthetic user to be able to donn and doff the prosthesis independently[3]. An overall good sense of balance may also allow the user to ambulate without using additional gait aids such as crutches.
- Ability to contain abdominal soft tissue
The HD socket must fit firmly and encompass all of the soft tissue in the abdominal region to enable more effective transfer of forces during gait, increase stability and capture lordosis more effectively[3]. Although not a strict requirement, individuals with lower body weight tend to have more successful prosthetic outcomes at this level[3].
Prosthetic Design and Components for Hip Disarticulation and Hemipelvectomy[edit | edit source]
Despite the physical differences between HP and HD amputation levels, the prosthetic components and prosthetic design for the two levels is the same[8].
The current standard is based on the Canadian hip disarticulation prosthesis, a design originally pioneered in the 1950s by McLaurin[9][3][4]. This type of prosthesis features a prosthetic hip joint mounted anteriorly on the socket, and below the level of the anatomical hip joint. This joint positioning is in contrast to older HP prosthesis designs which mounted the hip joint laterally and in line with the anatomical location.
A major challenge of prostheses at this level is to ensure adequate safety and stability for the user while still enabling functionality (i.e. knee and hip flexion during swing and stance phase). Thus the key advantage of the Canadian hip disarticulation prosthesis design is that the overall stability can be influenced by the prosthetic alignment[3], or the relationship between the position of the hip, knee and foot components. Placing the hip joint anteriorly on the socket brings the centre of gravity further anteriorly and allows it to fall in front of the knee joint, thus providing passive stability at both the hip and knee joints during standing[4].
PIC
Other factors affecting stability include the type of components used and how they function in combination with each other. A thorough physical assessment of the individual is essential as it can help can guide the selection of components, with careful consideration to the their personal requirements and activity level.
Another method to help aid stability is to shorten the overall length of the prosthesis by approximately 1cm compared to the contralateral limb. This allows for additional toe clearance during the swing phase of gait, although depending on the components used, this compensation may not always be necessary [8][4].
Socket[edit | edit source]
A total embracing socket is made by making a plaster cast of the individual’s pelvis allowing the socket to enclose the iliac crest(s)[12]. The socket can be made from different types of materials. The socket for a hindquarter amputation will also contain the abdominal and pelvic contents. There are 2 main ways of casting for the socket, using forming blocks or total contact casting
Weight bearing within the socket is transferred to the ischial tuberosity and buttocks of the sound limb for hindquarter amputation, and the ischium and buttock of the amputated side for a hip disarticulation amputation.
Suspension[edit | edit source]
Total tissue contact is the method used for suspension with the upper edges of the socket grasping/locking over the iliac crests. A shoulder strap can add additional suspension[12].
Prosthetic Components[edit | edit source]
Feet[edit | edit source]
Different feet can be used and should be chosen based upon their weight and stability it will add to the knee joint. Dynamic response feet are commonly used. Read more about Prosthetic Feet using this link.
Knees[edit | edit source]
Read more about Prosthetic Knees using this link, these are the pros and cons for different prosthetic knees with a hip disarticulation amputation.
- Single-axis knees: For individuals with a single slow speed of walking this type of knee is a favourable choice because of its lightweight and friction control.
- Stance control knees: Not used
- Polycentric knees: Used for active individuals who are able to tolerate the increased weight. With a person with a hip disarticulation with no prosthetic hip, this knee will allow some knee flexion that will shorten the leg to help with the swing.
- Hydraulic knees are not often used because of the increased weight but it may be chosen to initiate hip flexion during the swing phase of gait.
- Microprocessor knees: Even just applying a microprocessor knee as part of the prosthesis can reduce energy expenditure during gait[13].
Hip Components/Joints[3][12][edit | edit source]
Hip Limiter
This is a mechanism attached on the front of the socket that allows movement of the hip in swing phase. The limiter controls movement that can be adjusted to increase or decrease step length as the individual becomes more active. A locking mechanism can be attached if required by the individual.
Endoskeletal designs: Double anterior and posterior free motion hinges that allow for hip extension by means of rubber bands, and a manual hip lock. It is relatively lightweight. Sitting is difficult due to the distal components.
Energy Storing Interjoint segment
The individual can release energy from the hip joint by changing the amount of pelvic thrust during toe off. This will also help to control the knee extension. Foot rise is controlled and will lead to prosthesis shortening for toe clearance during swing. With this system, the prosthesis does not have to be shortened to provide for toe clearance and will prevent gait deviations like vaulting to occur.
Four-bar joint/polycentric
This hip joint allows for an easier and smoother walking pattern because by shortening the length of the prosthesis it helps to clear the foot during the swing phase. It is attached on the front of the socket and is therefore not in the way when sitting.
Helix 3D Prosthetic Hip is an example of a more recent polycentric hip joint. This hip leads to a more natural gait by allowing for toe clearance and smooth steps. It is paired with specific microprocessor knees.
In a study where robotics were applied to the prosthetic hip joint, it resulted in more symmetry during gait[13]
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 Yari P, Dijkstra PU, Geertzen JH. Functional outcome of hip disarticulation and hemipelvectomy: a cross-sectional national descriptive study in the Netherlands. Clinical Rehabilitation. 2008 Dec;22(12):1127-33
- ↑ 2.0 2.1 Huffman A, Schneeberger S, Goodyear E, West JM, O'Brien AL, Scharschmidt TJ, Mayerson JL, Schulz SA, Moore AM. Evaluating hip disarticulation outcomes in a 51-patient series. Journal of Orthopaedics. 2022 May 1;31:117-20.
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 3.6 3.7 Stark G. Overview of hip disarticulation prostheses. JPO: Journal of Prosthetics and Orthotics. 2001 Jun 1;13(2):50-3.
- ↑ 4.0 4.1 4.2 4.3 Gholizadeh H, Baddour N, Botros M, Brannen K, Golshan F, Lemaire ED. Hip disarticulation and hemipelvectomy prostheses: A review of the literature. Prosthetics and Orthotics International. 2021 Oct 1;45(5):434-9
- ↑ 5.0 5.1 Kralovec ME, Houdek MT, Andrews KL, Shives TC, Rose PS, Sim FH. Prosthetic rehabilitation after hip disarticulation or hemipelvectomy. American Journal of Physical Medicine & Rehabilitation. 2015 Dec 1;94(12):1035-40
- ↑ Chandler Balkman. Hip disarticulation prosthetic gait demonstration 2022. Available from: https://www.youtube.com/watch?v=bSq-tirpTIM [last accessed 9/7/2022]
- ↑ prostheticsinmotion. Hip Disarticulation Amputee Excels with the Otto Bock Helix Hip Joint. Available from: https://www.youtube.com/watch?v=U77D-J46cnU [last accessed 9/7/2022]
- ↑ 8.0 8.1 Van der Waarde T, Michael J. Hip Disarticulation and Transpelvic Amputation: Prosthetic Management. Atlas of Limb Prosthetics: Surgical, Prosthetic, and Rehabilitation Principles. 2002.
- ↑ Solomonidis SE, Loughran AJ, Taylor J, Paul JP. Biomechanics of the hip disarticulation prosthesis. Prosthetics and Orthotics International. 1977 Apr;1(1):13-8.
- ↑ Cale Konetchy. Ottobock Hip Casting Video. Available from: https://youtu.be/rRRXhef_0iM
- ↑ Martin Bionics. Bikini of Hip Sockets Hammock Casting Stand Explained. Available from: https://youtu.be/rFIs9BOU2bU
- ↑ 12.0 12.1 12.2 Engstrom B, Van de Ven C, editors. Therapy for amputees. Elsevier Health Sciences; 1999
- ↑ 13.0 13.1 Ueyama Y, Kubo T, Shibata M. Robotic hip-disarticulation prosthesis: evaluation of prosthetic gaits in a non-amputee individual. Advanced Robotics. 2020 Jan 2:1-8.
- ↑ Chandler Balkman. Helix Hip. Available from: https://youtu.be/668uiI0arN0
- ↑ crystald563. Crystal's prosthesis for hip disarticulation. Available from: https://www.youtube.com/watch?v=9G1rvk_Dt50
- ↑ POACFL. NPS Prosthesis for Hip Disarticulate / Hemipelvectomy Amputees. Crystal's prosthesis for hip disarticulation. Available from: https://youtu.be/soAB8qHl890