Pelvic Floor Muscle Function and Strength: Difference between revisions
No edit summary |
No edit summary |
||
| Line 69: | Line 69: | ||
=== Vaginal weights or cones === | === Vaginal weights or cones === | ||
Vagina cones can be used for both the measurement process and the training process. | Vagina cones can be used for both the measurement process and the training process. | ||
{{#ev:youtube|https://youtu.be/horceqF3TIg }} | |||
=== Measurement of lift === | === Measurement of lift === | ||
Revision as of 18:01, 18 February 2019
Original Editor - Kirsten Ryan
Top Contributors - Redisha Jakibanjar, Laura Ritchie, Mandy Roscher, Admin, Nicole Hills, Alicia Fernandes, Kirsten Ryan, Temitope Olowoyeye, WikiSysop, Kim Jackson, Claire Knott and Scott Buxton
Definition[edit | edit source]
Pelvic floor muscle function can be defined as the proper squeeze or contraction of the pelvic muscle.
Pelvic floor muscle strength can be defined as maximum voluntary contraction a person attempts to recruit as many fibers in a muscle as possible.[1]
Importance of proper evaluation of pelvic floor muscle and function[edit | edit source]
· Pelvic muscles are deep and are very difficult to contract isolately despite of the instructions given.
· Pelvic floor evaluation post and pretreatment help to know the efficacy of the treatment
Assessment methods[edit | edit source]
Methods for evaluating PFM function and strength can be categorized as:
1. Methods to measure the ability to contract (clinical observation, vaginal palpation, ultrasound, MRI, electromyography [EMG]).
2. Measures to quantify strength (manual muscle test by vaginal palpation, manometry, dynamometry, cones).
External Observation[edit | edit source]
External visual observation of the perineum may be utilized to visualize what the patient does when asked to contract the pelvic floor and is usually the initial step is assessing pelvic floor muscle function. Caution against using observation as the only assessment as the inward movement of the skin may be created by contraction of the superficial perineal muscles and have no influence on urethral closure mechanism. In women who are obese, a correct lift can be difficult to observe externally.
Vaginal palpation[edit | edit source]
Vaginal palpation is first described by Kegel to evaluate the pelvic floor muscle function and classified the contraction qualitatively as correct or not correct. For measuring PFM strength, he developed the “perineometer,” a pressure manometer, which measured the ability of the PFM to develop vaginal squeeze pressure. Nowadays, more than 25 different vaginal palpation methods have been developed. There has been no systematic research to determine the best method of vaginal palpation to assess the ability to contract.
Ultrasound and MRI[edit | edit source]
Recently, real time diagnostic ultrasound and MRI have been used to evaluate PFM function during contraction.
EMG[edit | edit source]
Electromyography is used to evaluate the pelvic floor muscle especially through the surface electrode.
PFM activation recorded using transperineal sEMG is only weakly correlated with PFM strength. Results from perineal sEMG should not be interpreted in the context of reporting PFM strength.[2]
| [3] |
Digital Palpation[edit | edit source]
Digital palpation of the vagina PFM is the standard when assessing the ability to contract the PFM by most physical therapists. The quality of contraction and upward movement can be assessed digitally.[1]
Manual muscle testing[edit | edit source]
Laycock developed the modified Oxford Grading System to measure PFM strength using vaginal palpation of the PFM. This is a 6-point scale:
0-no contraction,
1-flicker,
2-weak,
3-moderate,
4-good (with lift), and
5-strong.
This measurement scale is commonly used by physical therapists because it can be incorporated with vaginal palpation in the clinical assessment.
Manometers and Dynamometers[edit | edit source]
Manometry and dynamometry are more reliable tools than vaginal palpation for the assessment of PFM strength in women with pelvic floor disorders, especially when different raters are involved.[2]
Vaginal weights or cones[edit | edit source]
Vagina cones can be used for both the measurement process and the training process.
Measurement of lift[edit | edit source]
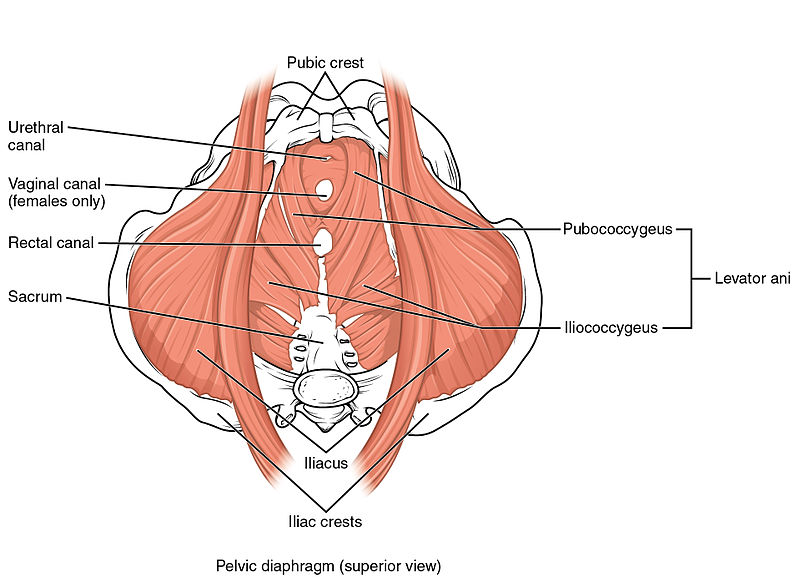
MRI and ultrasound can detect the actual lift inside the pelvis.
Presentations[edit | edit source]
 |
Pelvic Physiotherapy - to Kegel or Not?
This presentation was created by Carolyn Vandyken, a physiotherapist who specializes in the treatment of male and female pelvic dysfunction. She also provides education and mentorship to physiotherapists who are similarly interested in treating these dysfunctions. In the presentation, Carolyn reviews pelvic anatomy, the history of Kegel exercises and what the evidence tells us about when Kegels are and aren't appropriate for our patients. |
References[edit | edit source]
- ↑ 1.0 1.1 Bo K, Sherburn M. Evaluation of female pelvic-floor muscle function and strength. Phys Ther 2005;85:269-282.
- ↑ 2.0 2.1 Navarro Brazález B, Torres Lacomba M, de la Villa P, Sanchez Sanchez B, Prieto Gómez V, Asúnsolo del Barco Á, McLean L. The evaluation of pelvic floor muscle strength in women with pelvic floor dysfunction: A reliability and correlation study. Neurourology and urodynamics. 2018 Jan;37(1):269-77. available from : https://www.ncbi.nlm.nih.gov/pubmed/28455942
- ↑ Tom Ockler, PT. Trigger point assessment and treatment for Pelvic Floor triggers M 3 Seminar. Available from: http://www.youtube.com/watch?v=cWJwGvFDGLg [last accessed 30/04/14]