Pelvic Floor Muscle Function and Strength: Difference between revisions
(adding of contents, videos and editing grammar) |
(Reworked content, took out statements that were straight from articles. Added in new literature and recent evidence.) |
||
| Line 5: | Line 5: | ||
</div> | </div> | ||
== | == Introduction == | ||
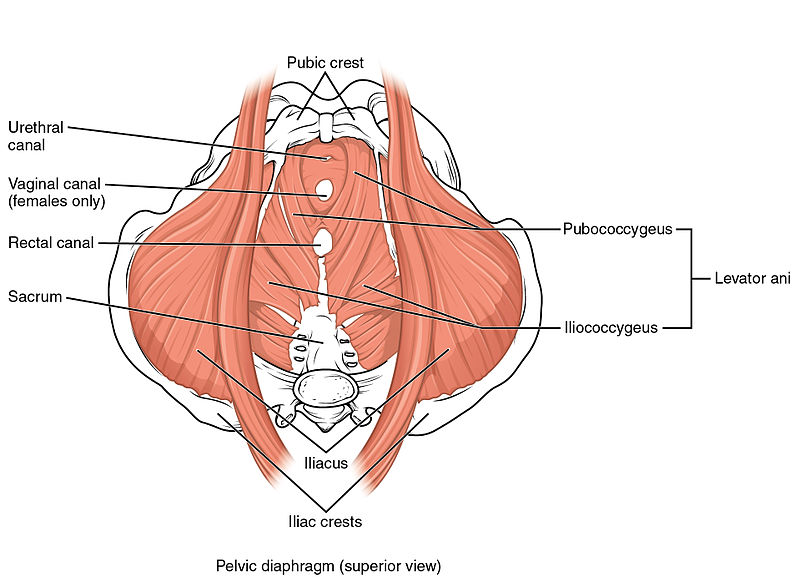
[[Pelvic Floor|Pelvic floor | The [[Pelvic Floor Anatomy|Pelvic floor muscles]] (PFM) are found in base of the pelvis. There are superficial muscles as well as the deep levator ani muscles . Changes in their function and strength can contribute to Pelvic Floor Dysfunction (PP article), such as urinary or faecal incontinence, pelvic organ prolapse, pelvic pain. | ||
== Pelvic Floor Muscle Function == | |||
= | The Pelvic floor muscles provide several important functions such as pelvic organ support, bladder and bowel control and sexual function. The ability to contract the pelvic floor correctly can be difficult. A proper pelvic floor contraction encorporates both a squeeze and a lift without contraction of other muscles such as the adductors and gluts.<ref name="Bo">Bo K, Sherburn M. Evaluation of female pelvic-floor muscle function and strength. Phys Ther 2005;85:269-282.</ref> | ||
== Pelvic Floor Muscle Strength == | |||
The pelvic floor muscles provides so many functionsand as such they need to have the ability to maintain a sustained resting tone as well as quick contractions for continence and sexual function as well as the ability to relax to allow for urination and defeactation. | |||
Evaluating the strength of the pelvic floor muscles is not as simple as a single maximum voluntary contraction. Factors such as power, endurance, speed of contraction and ability to relax all need to be evaluated. | |||
[[File:Pelvic Floor Muscles.jpg|center|thumb|800x800px|pelvic floor muscles ]] | |||
== Importance of proper evaluation of pelvic floor muscle and function == | |||
Correct contraction of the pelvic floor cannot be observed externally. In people with pelvic floor dysfunction they often struggle to contract the pelvic floor correctly and a thorough examination will allow for an indivdualised treatment programme. It also allows for | |||
== | == Assessment methods == | ||
There are various methods that can be used to evaluate the pelvic floor muscles. There is no absolute gold standard for pelvic floor muscle assessment at the moment. Examination of each patient needs to be indivdualised to what they are comfortable with. | |||
Examination needs to look at the ability of the pelvic floor to contact correctly (squeeze and lift) as well as the strength and endurance of the actual contraction.<ref name="Bo" /> | |||
[[Image:Pelvic Floor Muscles.jpg|right|400px]] | |||
=== | === External Observation === | ||
External visual observation of the perineum may be utilized to visualize what happens when asked to contract the pelvic floor. It is usually the initial step is assessing pelvic floor muscle function. | |||
It is not appropriate to use observation as the only assessment method as the inward movement of the skin may be created by contraction of the [[Pelvic Floor Anatomy|superficial perineal muscles]] and there may be no contraction of the levator ani muscles.<ref name="Bo" /> | |||
=== | === Internal Vaginal Digital Palpation === | ||
Internal digital examination of the vagina is a helpful examination tool. It is performed by inserting a finger (or fingers) into the vaginal cavity. | |||
Pelvic Floor muscle contraction can be felt and the therapist is looking for both a squeeze and lift. | |||
When doing an internal vaginal palpation various aspects of pelvic floor muscle strength need to be examined. | |||
Laycock<ref>Laycock J, Jerwood D. Pelvic floor muscle assessment: the PERFECT scheme. Physiotherapy. 2001 Dec 1;87(12):631-42.</ref> developed the PERFECT Scheme which is a method of examination of the pelvic floor muscles that looks at | |||
* Power - Modified Oxford Scale) | |||
* Endurance - How long can they hold a maximal voluntary contraction, up to 10sec | |||
* Repetitions - How many maximal voluntary contractions they hold with a rest between them, up to 10 (eg 10 repetitiions of a 10 second hold) | |||
* Fast- The number of 1 second MVC they can perform in a row (up to 10) | |||
* Every Contraction Timed - reminder to time every contraction | |||
An internal vaginal examination has good intra-rater reliability but only fair intrarater reliability <ref name=":0" />. This means that follow up internal examinations by the same practitioner can provide useful information in clinical practice. | |||
1- | The advantage of an internal vaginal examination is that anatomical changes, symmetry of contraction, muscle tone as well as any painful areas can be examined as well as the muscle strength <ref name=":0" /><ref name=":1">Sherburn M, Murphy CA, Carroll S, Allen TJ, Galea MP. Investigation of transabdominal real-time ultrasound to visualise the muscles of the pelvic floor. Australian Journal of Physiotherapy. 2005 Jan 1;51(3):167-70.</ref> | ||
2- | === Ultrasound <ref name=":2">Thompson JA, O’Sullivan PB, Briffa K, Neumann P. Assessment of pelvic floor movement using transabdominal and transperineal ultrasound. International Urogynecology Journal. 2005 Aug 1;16(4):285-92.</ref><ref name=":1" /> === | ||
Real time trans-abdominal and trans-perineal ultrasound can both be used to assess pelvic floor contraction. Both have shown to be reliable in assessing movement of pelvic structures during contraction<ref name=":2" />. | |||
Trans abdominal ultrasound is a non-invasive, valid and reliable tool that can be used to assess pelvic floor muscle contraction<ref name=":1" />. By placing the ultrasound probe in the correct supra-pubically the examiner can evaluate both the squeeze and lift component of the contraction<ref name=":1" />. | |||
Real-time ultrasound is helpful as it provides a good visual feedback tool for patients to use as a means of correctly contracting their pelvic floor muscles. Transabdominal ultrasound is also non-invasive so can be used in patients who are not comfortable with an internal examination or where an internal examination is contra-indicated eg children.{{#ev:youtube|https://youtu.be/nrt7SqoUSZ4}}<ref>Using Real Time Ultrasound Imaging to assess Pelvic floor function. Lifecare pilates. Available from:https://youtu.be/nrt7SqoUSZ4 </ref> | |||
=== MRI === | |||
MRI can be used to evaluate for pelvic floor dysfunction as well as the ability of the pelvic floor to lift while contracting. Clinically it is very expensive and is not used widely for PFM assessment. | |||
=== EMG === | |||
Surface Electromyography can be used to evaluate the pelvic floor muscle, | |||
PFM activation recorded using transperineal sEMG is only weakly correlated with PFM strength. Results from perineal sEMG should not be interpreted in the context of reporting PFM strength.<ref name=":0">Navarro Brazález B, Torres Lacomba M, de la Villa P, Sanchez Sanchez B, Prieto Gómez V, Asúnsolo del Barco Á, McLean L. The evaluation of pelvic floor muscle strength in women with pelvic floor dysfunction: A reliability and correlation study. Neurourology and urodynamics. 2018 Jan;37(1):269-77. available from : https://www.ncbi.nlm.nih.gov/pubmed/28455942</ref> | |||
=== Manometers and Dynamometers === | === Manometers and Dynamometers === | ||
Manometry and dynamometry are | Manometry and dynamometry are reliable tools that can measure a pelvic floor muscle contraction and may be superior to digital palpation as an objective measure of strenth.<ref name=":0" /> | ||
== | == Conclusion == | ||
There are a variety of ways to assess PFM function and strength. Real-time ultrasound and internal digital palpation are probably the most widely used in clinical practice as they are the most cost-effective and efficient means of examination. Manometry and Dynamoetry may however, provide a more accurate measurement of strength. | |||
When assessing PFM function and strength it is important to correlate multiple examination findings to ensure accurate evaluation. | |||
=== Presentations === | === Presentations === | ||
Revision as of 14:49, 20 February 2019
Original Editor - Kirsten Ryan
Top Contributors - Redisha Jakibanjar, Laura Ritchie, Admin, Mandy Roscher, Kirsten Ryan, Nicole Hills, Alicia Fernandes, Temitope Olowoyeye, WikiSysop, Kim Jackson, Scott Buxton and Claire Knott
Introduction[edit | edit source]
The Pelvic floor muscles (PFM) are found in base of the pelvis. There are superficial muscles as well as the deep levator ani muscles . Changes in their function and strength can contribute to Pelvic Floor Dysfunction (PP article), such as urinary or faecal incontinence, pelvic organ prolapse, pelvic pain.
Pelvic Floor Muscle Function[edit | edit source]
The Pelvic floor muscles provide several important functions such as pelvic organ support, bladder and bowel control and sexual function. The ability to contract the pelvic floor correctly can be difficult. A proper pelvic floor contraction encorporates both a squeeze and a lift without contraction of other muscles such as the adductors and gluts.[1]
Pelvic Floor Muscle Strength[edit | edit source]
The pelvic floor muscles provides so many functionsand as such they need to have the ability to maintain a sustained resting tone as well as quick contractions for continence and sexual function as well as the ability to relax to allow for urination and defeactation.
Evaluating the strength of the pelvic floor muscles is not as simple as a single maximum voluntary contraction. Factors such as power, endurance, speed of contraction and ability to relax all need to be evaluated.
Importance of proper evaluation of pelvic floor muscle and function[edit | edit source]
Correct contraction of the pelvic floor cannot be observed externally. In people with pelvic floor dysfunction they often struggle to contract the pelvic floor correctly and a thorough examination will allow for an indivdualised treatment programme. It also allows for
Assessment methods[edit | edit source]
There are various methods that can be used to evaluate the pelvic floor muscles. There is no absolute gold standard for pelvic floor muscle assessment at the moment. Examination of each patient needs to be indivdualised to what they are comfortable with.
Examination needs to look at the ability of the pelvic floor to contact correctly (squeeze and lift) as well as the strength and endurance of the actual contraction.[1]
External Observation[edit | edit source]
External visual observation of the perineum may be utilized to visualize what happens when asked to contract the pelvic floor. It is usually the initial step is assessing pelvic floor muscle function.
It is not appropriate to use observation as the only assessment method as the inward movement of the skin may be created by contraction of the superficial perineal muscles and there may be no contraction of the levator ani muscles.[1]
Internal Vaginal Digital Palpation[edit | edit source]
Internal digital examination of the vagina is a helpful examination tool. It is performed by inserting a finger (or fingers) into the vaginal cavity.
Pelvic Floor muscle contraction can be felt and the therapist is looking for both a squeeze and lift.
When doing an internal vaginal palpation various aspects of pelvic floor muscle strength need to be examined.
Laycock[2] developed the PERFECT Scheme which is a method of examination of the pelvic floor muscles that looks at
- Power - Modified Oxford Scale)
- Endurance - How long can they hold a maximal voluntary contraction, up to 10sec
- Repetitions - How many maximal voluntary contractions they hold with a rest between them, up to 10 (eg 10 repetitiions of a 10 second hold)
- Fast- The number of 1 second MVC they can perform in a row (up to 10)
- Every Contraction Timed - reminder to time every contraction
An internal vaginal examination has good intra-rater reliability but only fair intrarater reliability [3]. This means that follow up internal examinations by the same practitioner can provide useful information in clinical practice.
The advantage of an internal vaginal examination is that anatomical changes, symmetry of contraction, muscle tone as well as any painful areas can be examined as well as the muscle strength [3][4]
Ultrasound [5][4][edit | edit source]
Real time trans-abdominal and trans-perineal ultrasound can both be used to assess pelvic floor contraction. Both have shown to be reliable in assessing movement of pelvic structures during contraction[5].
Trans abdominal ultrasound is a non-invasive, valid and reliable tool that can be used to assess pelvic floor muscle contraction[4]. By placing the ultrasound probe in the correct supra-pubically the examiner can evaluate both the squeeze and lift component of the contraction[4].
Real-time ultrasound is helpful as it provides a good visual feedback tool for patients to use as a means of correctly contracting their pelvic floor muscles. Transabdominal ultrasound is also non-invasive so can be used in patients who are not comfortable with an internal examination or where an internal examination is contra-indicated eg children.
MRI[edit | edit source]
MRI can be used to evaluate for pelvic floor dysfunction as well as the ability of the pelvic floor to lift while contracting. Clinically it is very expensive and is not used widely for PFM assessment.
EMG[edit | edit source]
Surface Electromyography can be used to evaluate the pelvic floor muscle,
PFM activation recorded using transperineal sEMG is only weakly correlated with PFM strength. Results from perineal sEMG should not be interpreted in the context of reporting PFM strength.[3]
Manometers and Dynamometers[edit | edit source]
Manometry and dynamometry are reliable tools that can measure a pelvic floor muscle contraction and may be superior to digital palpation as an objective measure of strenth.[3]
Conclusion[edit | edit source]
There are a variety of ways to assess PFM function and strength. Real-time ultrasound and internal digital palpation are probably the most widely used in clinical practice as they are the most cost-effective and efficient means of examination. Manometry and Dynamoetry may however, provide a more accurate measurement of strength.
When assessing PFM function and strength it is important to correlate multiple examination findings to ensure accurate evaluation.
Presentations[edit | edit source]
 |
Pelvic Physiotherapy - to Kegel or Not?
This presentation was created by Carolyn Vandyken, a physiotherapist who specializes in the treatment of male and female pelvic dysfunction. She also provides education and mentorship to physiotherapists who are similarly interested in treating these dysfunctions. In the presentation, Carolyn reviews pelvic anatomy, the history of Kegel exercises and what the evidence tells us about when Kegels are and aren't appropriate for our patients. |
References[edit | edit source]
- ↑ 1.0 1.1 1.2 Bo K, Sherburn M. Evaluation of female pelvic-floor muscle function and strength. Phys Ther 2005;85:269-282.
- ↑ Laycock J, Jerwood D. Pelvic floor muscle assessment: the PERFECT scheme. Physiotherapy. 2001 Dec 1;87(12):631-42.
- ↑ 3.0 3.1 3.2 3.3 Navarro Brazález B, Torres Lacomba M, de la Villa P, Sanchez Sanchez B, Prieto Gómez V, Asúnsolo del Barco Á, McLean L. The evaluation of pelvic floor muscle strength in women with pelvic floor dysfunction: A reliability and correlation study. Neurourology and urodynamics. 2018 Jan;37(1):269-77. available from : https://www.ncbi.nlm.nih.gov/pubmed/28455942
- ↑ 4.0 4.1 4.2 4.3 Sherburn M, Murphy CA, Carroll S, Allen TJ, Galea MP. Investigation of transabdominal real-time ultrasound to visualise the muscles of the pelvic floor. Australian Journal of Physiotherapy. 2005 Jan 1;51(3):167-70.
- ↑ 5.0 5.1 Thompson JA, O’Sullivan PB, Briffa K, Neumann P. Assessment of pelvic floor movement using transabdominal and transperineal ultrasound. International Urogynecology Journal. 2005 Aug 1;16(4):285-92.
- ↑ Using Real Time Ultrasound Imaging to assess Pelvic floor function. Lifecare pilates. Available from:https://youtu.be/nrt7SqoUSZ4