Paediatric Conditions of the Foot
This article or area is currently under construction and may only be partially complete. Please come back soon to see the finished work! (22/11/2023)
Top Contributors - Stacy Schiurring, Jess Bell and Kim Jackson
Introduction[edit | edit source]
Optional reading: for an in-depth review of foot structure and functional anatomy, please read this article.
Metatarsus Adductus (Metatarsus Varus)[edit | edit source]
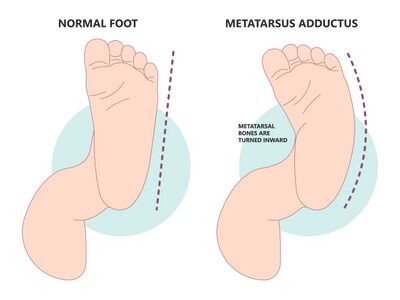
"Metatarsus adductus primarily involves medial deviation of the forefoot on the hindfoot." - Pediatric Orthopedic Society of North America (POSAN)[1]
Secondary characteristics include:
- prominence of the 5th metatarsal base [1]
- neutral[2] to slightly valgus hindfoot [1]
- slightly supinated forefoot [1]
- a possible widening of the space between the 1st and 2nd toes [1]
- many patients also have internal tibial torsion [1]
- no ankle range of motion (ROM) restrictions [2]
Metatarsus Adductus can be divided into two types:
- Flexible: Presents with adduction of the 5 metatarsal bones at the tarsometatarsal joint.
- Rigid: Presents with medial subluxation of the tarsometatarsal joints. There is valgus of the hindfoot and the navicular is later to the head of the talus.
Incidence: 1/1,000 live births [1][2]
Aetiology:
- In utero compression
- Embryologic or congenital abnormalities [2]
Assessment[edit | edit source]
- Bleck’s Heel bisector line is a simple measure that assesses the flexibility and severity of metatarsus adductus. It is a manual assessment and no types of equipment is needed. This method has been used for over four decades, with some modifications. Recent research has shown that this method can be unclear and has the potential for measurement errors when measuring the heel bisector line (HBL).[3] Procedure:
- The shape of the weight-bearing foot is obtained. Traditionally a mould of the weight-bearing foot is made, modifications include the use of footprints or photos the weight-bearing foot.[3] Another option includes placing the child in prone with knees flexed to 90°, and the plantar surface of the foot parallel to the ceiling.[2]
- Next, the procedure is completed by determining the longitudinal axis of the ellipse with a straight edge, independent of the forefoot.[3]
- Classification of metatarsus adductus according to Bleck’s classification involves observation of where the HBL crosses the metatarsal heads.[3]Add image from video?
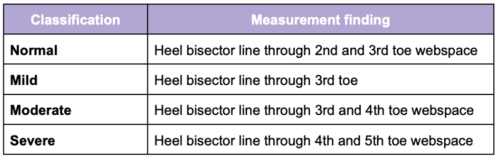 Bleck's classification of metatarsus adductus[2]
Bleck's classification of metatarsus adductus[2]
- Transmalleolar Axis Bisector (TMAB) is an newly proposed alternative assessment technique for measuring the severity of metatarsus adductus. [3] Procedure:[3]
- The child in prone with knees flexed to 90° and the plantar surface of the foot parallel to the ceiling. Weight-bearing of the foot is approximated by maintaining the ankle in a plantigrade position.
- Using a pair of vernier calipers, a line is drawn across the heel connecting the most medial point of the medial malleolus to the most lateral point of the lateral malleolus. The midpoint of this line is marked.
- A goniometer is then placed on the foot, with the axis on the marked midpoint, the stationary arm aligned on the drawn line. The moveable arm is placed at 90° to the stationary arm. The moveable arm delineates the TMAB.
- Classification of metatarsus adductus is based off the location of where the TMAB cross the metatarsal heads. There are currently no classification norms using this method as research is ongoing. Researchers recommend recording outcomes as TMAB at the second interdigital web space, third digit, third interdigital web space, etc. Create an image?
Intervention[edit | edit source]
- Mild cases: typically resolves without intervention[2]
- Moderate cases: [2]
- Stretching exercises
- Corrective shoe ware
- straight last
- reverse last
- Severe cases:[2]
- Manipulation
- Serial casting followed by corrective shoe ware
- Surgery should not considered before ages of four to allow for spontaneous resolution
Pes Planus (pes planovalgus or flat foot)[edit | edit source]
Pes Planus is "defined by the loss of the medial longitudinal arch of the foot where it contacts or nearly contacts the ground."[4]It can occur with or without further deformities of the foot and ankle.[5]
Pes planus can be divided into two types:
- Flexible: where the longitudinal arches of the foot are present on heel elevation (tiptoe standing) and non-bearing but disappear with full weight bearing on the foot.[6]
- Rigid: where the longitudinal arches of the foot are absent in both heel elevation (tiptoe standing) and weight bearing. This is normally associated with underlying pathology[8] such as vertical talus or tarsal coalition.[5]
Incidence: 7 to 22% of the general population[2]
Aetiology:
- Congenital: most infants have flat feet due to ligamentous laxity and developing neuromuscular control. Only a small percentage of children fail to develop normal arches. Children with Down Syndrome, Marfan Syndrome, or Ehlers-Danos Syndrome can be prone to congenital ligamentous laxity.[4]
- Aquired: most commonly associated with posterior tibial tendon dysfunction
Factors that can contribute to an increased flat foot:
- Little time spent barefoot resulting in weak foot intrinsic muscles and poor foot arch development[2]
- Childhood obesity[2][4]
Assessment[edit | edit source]
- Significant malalignment with or without associated pain:
- Presence of an accessory navicular bone
- Lack of mobility:
- Need to rule out tarsal coalition with rigid or limited subtalar motion
- A full-body postural assessment can also be useful to rule out issue further up the kinetic chain
- Neuro screen[2]
Intervention[edit | edit source]
"... we don't need to correct if they don't have pain, if there's no problem with their gait, or their ability to participate in activities of interest. " -Krista Eskay, PT[2]
Rehabilitation Interventions:
- Pain management
- Stretching/increasing ankle flexibility
- Strengthening foot intrinsics and ankle muscles
- Proprioceptive training
- Family education and reassurance
Providing additional support:
- Shoes with an arch support. This will not correct the deformity but will provide additional stability and can result in improved mobility and gait.
- Orthotics
When to refer:
- to an orthopedist:
- if the longitudinal arch of the foot are absent on heel elevation, or is asymmetrical
- significant pain affecting activities of daily living or mobility
- to a neurologist:
- abnormal neuro screen
- if under five years of age, pain in their knees, hips and feet
- to a physical medicine specialist:
- if under five years of age, pain in their knees, hips and feet
Pes Cavus[edit | edit source]
Clubfoot (Talipes Equinovarus)[edit | edit source]
Clubfoot "is one of the most common congenital malformations and is characterized across varying degrees and severity of predictable contractures manifesting with four main components: (1) midfoot cavus, (2) forefoot adductus, (3) heel/hindfoot varus and (4) hindfoot equinus."[9]
- occurs twice as often in male as in female babies[9]
- can be unilateral or bilateral[2]
- involved foot can be smaller and shorter in size[2]
- clubfoot will have an empty heel pad[2]
- transverse plantar crease present[2]
Incidence: 1/1,000 live births[2][10]
Aetiology:
- Idiopathic: approximately 80% of cases
- Other cases tend to be associated with disorders such as Spina Bifida, Cerebral Palsy and Arthrogryposis[11]
Assessment[edit | edit source]
When assessing the foot, there are several distinctive deformities associated with clubfoot:[9][12]
- midfoot cavus
- forefoot adductus
- hindfoot varus
- hindfoot equinus.
These deformities can present with a range of orthopaedic deformity and degree of stiffness.[9] Several scoring systems exist[2] and can be used to help in the assessment and classifying the degree of deformity present. According to the literature, there is no gold standard grading method for assessing or monitoring the degree of deformity associated with clubfoot.[12]
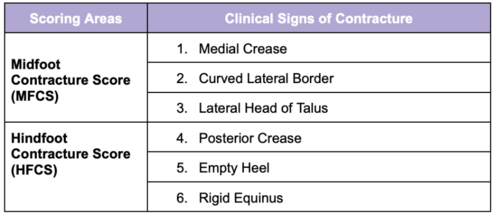
- Pirani Scoring System is based on 6 well-described Clinical Signs of Contracture characterising a severe clubfoot. This scoring system quantifies the degree of clubfoot deformity in Pirani classification uses for the deformity component of the clubfoot 0, ½, and 1 point to evaluate the degree and severity of the deformity. In particular, the hind and medial part of the foot are evaluated separately. In each of these parts, we evaluated three parameters: the hind foot contracture score (HCFS), dorsal crease, empty heel, and rigid equinus; and the mid-foot contracture score (MFCS), medial creasy, lateral edge convexity, and talus head position. The maximum number of points corresponding to the deformity is six. The assessment is performed with the examiner in sitting. The infant is on the mother’s lap. A feeding, relaxed infant allows a more precise examination. The measurements are made while the examiner is gently correcting the foot with minimal effort, and no discomfort.[13]The six areas assessed include three signs from the midfoot and three signs from the hindfoot. The six areas as scored as described below, then the scores are summed to a Total Score, which ranges from 0-6. The higher the score, the more severe the presentation.
- If the sign is severely abnormal it scores 1
- If it is partially abnormal it scores 0.5
- If it is normal it scores 0 For more information on using this scoring system please read this article. For a clinical example, please see this article.
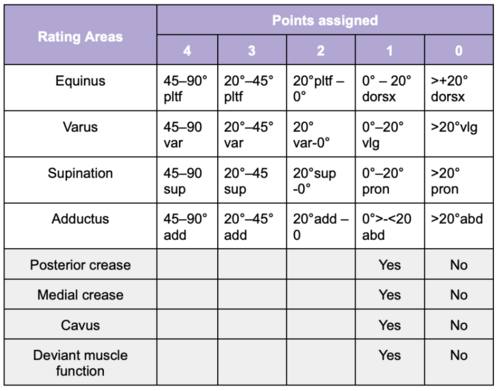
- Dimeglio Classification Scoring System is based on 8 rated areas characterising clubfoot. It focuses on assessing the mobility of the clubfoot deformity.[14] Total score ranges between 0-20. The higher the score, the more severe the presentation.
- very severe: 16–20
- severe 11–15
- moderate 6–10
- postural 0–5
Interventions[edit | edit source]
The purposes of clubfoot therapy are to achieve and maintain clubfoot correction, so that the patients have functional, painless, plantigrade feet with good mobility (Ponseti, & Campos, 2009). [12]
- The standard is the Ponseti method. It's been around for a long time since the 1940s. It's this really comprehensive technique for treating congenital clubfoot abnormalities. The thing is, is it's a long process and if you don't follow through with the whole process, risk of recurrence is higher.
So really what we want to think about doing is taking and applying forces to the foot that start within the first few weeks of life. And if we apply forces gradually over time, a lot of club feet can be corrected without major reconstructive surgery, but still might be associated with some minor reconstructive surgery. So this has become the most widely practised technique and method for initial treatment of infants with clubfoot. So we're going to go through the Ponseti method a little bit so that you have a good understanding of the different components.
So there's two phases, the treatment phase and the maintenance phase. The maintenance phase is the one that's really tough because a lot of families, because of just the amount of effort that it requires, aren't able to consistently keep up with it, and this is done to prevent recurrence. So a lot of times this is when we'll see they have a good correction. But they're unable to maintain it. So the treatment phase is when the deformity is actually physically corrected. Maintenance phase is a time when there's braces that are utilised to prevent recurrence. So it's really important to pay attention to details because you really want to make sure that you get all of these corrections appropriate as you go along.
So treatment, you want to begin this as early as possible. We're talking within the first week of life. Typically what happens is first, you have manipulations and casting that are done on a weekly basis. So you have a serial casting that is done, so you get a cast. A week later, the cast gets taken off and changed, and the foot gets put in a new position. So this cast is meant to hold the foot in a corrected position and allow it to reshape gradually over time. Typically you're going to need about five to six casts to fully correct the alignment of the foot and the ankle. And when that final cast goes on, the majority of infants will then still require a minor surgery compared to what it would take to surgically correct everything. And this is to gain adequate length of their Achilles tendon. It's called a percutaneous Achilles lengthening.
So in that maintenance phase, the final cast is going to remain in place for three weeks, and then the foot is going to be placed into a removable orthotic device. The orthotic needs to be worn for 23 hours per day for three months, and then during the nighttime for several years after that. So you can see why the carryover of this with families is potentially difficult. But failure to carry over and use this properly and correctly in its entirety, can result in recurrence of the clubfoot deformity. So good results have been demonstrated when people are able to maintain this protocol and they can have foot function like a typical foot.
So all of the casts are long leg casts that are applied, and they're applied from the toes all the way up to the groin, and they are going to address a lot of different corrections that are needed. So the first cast, or really address that pronation and plantarflexion of the first ray and the forefoot adduction. So, after the first cast, the foot is much straighter and that cavus position of the foot are often no longer present. The second cast is going to focus more on straightening the foot and aligning the forefoot with the heel. So for this we really want to make sure that we still keep them in plantarflexion. We're not worried about getting that dorsiflexion range of motion yet, because we're still working on the foot position. So before casting, you'll have someone that's going to manipulate the foot, determine the amount of correction that they can maintain, hold that position, they'll apply this plaster cast, and really focusing again on that forefoot abduction. So moving it out of that adducted position. The heel is often not directly manipulated. So even though that heel is really pulled inwards a lot of the time, what often happens is there's a gradual correction of the hindfoot and the midfoot. As that forefoot is corrected.
Further casting goes from four to five casts beyond that, and for this, we're really looking at, again, continuing to correct the foot position, the forefoot position. Allow that hindfoot varus to realign. And then once the hindfoot is realigned, that's when you can start to work on the dorsiflexion. If after all of the casting, their dorsiflexion is still less than 15 degrees past neutral. That's when they'll do that percutaneous Achilles tenotomy. So that percutaneous tendon release is really when that achilles tendon is still too short and the child can't fully dorsiflex through a full range of motion.
So it happens in most children. I think up to 70% of them will still require this. And this is to allow that full ankle range of motion. But it's relatively a small procedure compared to the malalignment that we see originally from a clubfoot. And then a final cast is put on. Goals of this cast are 15 degrees of dorsiflexion and 70 degrees of foot abduction. This is typically on for three weeks and more are really rarely needed unless it's some really severe cases of clubfoot. So the results are really good. So you can see here stage one up through those mid stages of casting until you get that nice neutral foot alignment and then you get that dorsiflexion. And this is kind of what their casts look like as they went through their casting.
So the maintenance and recurrence prevention is really the tough part. So after you get that final cast cut off, they're often placed in this foot abduction orthosis. And this is really to maintain foot in proper position with the forefeet really set apart and pointed upwards. And this is unfortunately used with a brace that has shoes mounted to a bar and it needs to be worn 23 hours a day for the first three months of life, and after that, sleeping for several years, around age of three or four. So you can see that when you do this perfectly, the recurrence is close to zero, but doing this perfectly is really, really hard. So when it's not worn, according to the guidelines, there is a much higher risk of recurrence.
Because the risk of recurrence can persist for several years after the casting is complete. What you want to do is as soon as you start to notice that there is a recurrence, go back, have more long leg plaster casts applied at two week intervals. So again, we're going back to the serial application of casting and that's really going to help to correct the foot deformity and any ankle tightness that has developed since then. An Achilles tendon lengthening could potentially be necessary if you aren't able to fully correct and regain that ankle range of motion. And then even more in depth as a tendon transfer where they'll take the tibialis anterior tendon and transfer it to be able to give the Achilles more length. And this can be done in older children to help maintain the correction if their ankle starts to get tight again.
Resources[edit | edit source]
video of HBL?
- bulleted list
- x
or
- numbered list
- x
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 Pediatric Orthopaedic Society of North America (POSNA). Metatarsus Adductus. Available from: https://posna.org/physician-education/study-guide/metatarsus-adductus (accessed 29 October 2023).
- ↑ 2.00 2.01 2.02 2.03 2.04 2.05 2.06 2.07 2.08 2.09 2.10 2.11 2.12 2.13 2.14 2.15 2.16 2.17 2.18 2.19 Eskay, K. Paediatric Physiotherapy Programme. Paediatric Conditions of the Foot. Physioplus. 2023.
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 Alonge VO. Proposing Transmalleolar Axis Bisector (TMAB) as a Geometrically Accurate Alternative to the Heel Bisector Line for the Clinical Assessment of Metatarsus Adductus. Int J Foot Ankle. 2020;4:041.
- ↑ 4.0 4.1 4.2 4.3 National Institute of Health, National Library of Medicine. StatPearls | Pes Planus. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430802/#:~:text=Pes%20planus%20commonly%20referred%20to,fascia%20between%20the%20forefoot%20and (accessed 14 November 2023).
- ↑ 5.0 5.1 KAYMAZ B. Pediatric Pes Planus (flatfoot). Family Practice and Palliative Care. 2022 Oct 19;7(4):118-23.
- ↑ Kothari A, Bhuva S, Stebbins J, Zavatsky AB, Theologis T. An investigation into the aetiology of flexible flat feet: the role of subtalar joint morphology. A The Bone & Joint Journal. 2016 Apr;98(4):564-8
- ↑ Squibb M, Sheerin K, Francis P. Measurement of the Developing Foot in Shod and Barefoot Paediatric Populations: A Narrative Review. Children. 2022 May 19;9(5):750.
- ↑ Halabchi F, Mazaheri R, Mirshahi M, Abbasian L. Pediatric flexible flatfoot; clinical aspects and algorithmic approach. Iranian journal of pediatrics. 2013 Jun;23(3):247.
- ↑ 9.0 9.1 9.2 9.3 9.4 9.5 Barrie A, Varacallo M. Clubfoot. InStatPearls [Internet] 2022 Sep 4. StatPearls Publishing.
- ↑ Dibello D, Di Carlo V, Colin G, Barbi E, Galimberti A. What a paediatrician should know about congenital clubfoot. Italian Journal of Pediatrics. 2020 Dec;46(1):1-6.
- ↑ Bridgens J, Kiely N. Current management of clubfoot (congenital talipes equinovarus). BmJ. 2010 Feb 2;340(6):c355.
- ↑ 12.0 12.1 12.2 Martanto TW, Dominica H, Irianto KA, Bayusentono S, Utomo DN. The pirani score evaluation on patients with clubfoot treated with the ponsety method in public hospital. EurAsian Journal of BioSciences. 2020;14(2):3419-22.
- ↑ Africa Clubfoot Training Project. Chapter 4 Africa Clubfoot Training Basic & Advanced Clubfoot Treatment Provider Courses - Participant Manual. University of Oxford: Africa Clubfoot Training Project, 2017.
- ↑ Andriesse H, Roos EM, Hägglund G, Jarnlo GB. Validity and responsiveness of the Clubfoot Assessment Protocol (CAP). A methodological study. BMC Musculoskeletal Disorders. 2006 Dec;7(1):1-9.