Oxford Shoulder Score: Difference between revisions
No edit summary |
(rephrased the page as it had a plagiarism problem) |
||
| Line 2: | Line 2: | ||
== Objective == | == Objective == | ||
[[File:Shoulder Pain.png|thumb|Shoulder Pain]] | [[File:Shoulder Pain.png|thumb|Shoulder Pain]] | ||
A | A questionnaire of [[shoulder]] pain and function. it was devised in 1996 (Dawson, Fitzpatrick, & Carr, 1996) for assessing the outcomes of shoulder [[Surgery and General Anaesthetic|surgery]] and later was used for degenerative conditions (excluding conditions of [[Shoulder Instability|shoulder instability]]<ref name=":0">Younis F, Sultan J, Dix S, Hughes PJ. [https://link.springer.com/referenceworkentry/10.1007/978-94-007-0753-5_2048 The range of the Oxford Shoulder Score in the asymptomatic population: a marker for post-operative improvement.] The Annals of The Royal College of Surgeons of England. 2011 Nov;93(8):629-33.</ref>. | ||
== Intended Population == | == Intended Population == | ||
| Line 9: | Line 9: | ||
== Method of Use == | == Method of Use == | ||
[[File:The oxford shoulder score.png|thumb|520x520px|alt=|The oxford shoulder score]] | [[File:The oxford shoulder score.png|thumb|520x520px|alt=|The oxford shoulder score]] | ||
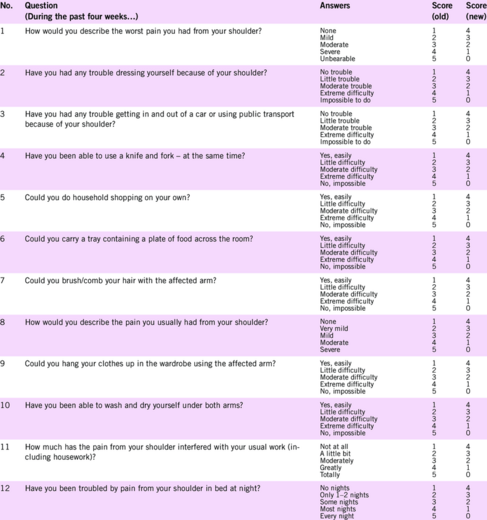
It contains 12 items, each with 5 | It contains 12 items, each with 5 answers. starting with 1 (best/fewest symptoms) to 5 (worst/most severe) which is awarded to correspond to the patient's symptoms. The total gives a minimum score of 12 and a maximum of 60. A higher score implies a greater degree of disability. | ||
In 2009 the scoring method for the OSS was modified so that each of the 12 items is scored from 4 (best/fewest symptoms) to 0 (worst/most severe) <ref>Younis F, Sultan J, Dix S, Hughes PJ. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3566690/#:~:text=The%20Oxford%20Shoulder%20Score%20(OSS,the%20range%20in%20asymptomatic%20individuals. The range of the Oxford Shoulder Score in the asymptomatic population: a marker for post-operative improvement.] The Annals of The Royal College of Surgeons of England. 2011 Nov;93(8):629-33.</ref>. | In 2009 the scoring method for the OSS was modified so that each of the 12 items is scored from 4 (best/fewest symptoms) to 0 (worst/most severe) <ref>Younis F, Sultan J, Dix S, Hughes PJ. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3566690/#:~:text=The%20Oxford%20Shoulder%20Score%20(OSS,the%20range%20in%20asymptomatic%20individuals. The range of the Oxford Shoulder Score in the asymptomatic population: a marker for post-operative improvement.] The Annals of The Royal College of Surgeons of England. 2011 Nov;93(8):629-33.</ref>. | ||
== Reference == | == Reference == | ||
The total score | The total score ranges from 48 to 0, after the modification of the score in 2009, a lower score indicates a greater degree of disability. | ||
=== Reliability === | === Reliability === | ||
the score was found to have a great interrater reliability and test-retest reliability<ref name=":0" />. | |||
=== Validity === | === Validity === | ||
Evidence of | Evidence suggested the validity of OSS to measure the degree of disability and detect the possible outcomes of shoulder surgery <ref name=":0" />. | ||
=== Responsiveness === | === Responsiveness === | ||
it was stated that the sensitivity of the OSS can detect the smallest of changes that might happen in response to treatment interventions.<ref name=":0" /> | |||
== Links == | == Links == | ||
Oxford Shoulder Score http://www.orthopaedicscore.com/scorepages/oxford_shoulder_score.html | Oxford Shoulder Score http://www.orthopaedicscore.com/scorepages/oxford_shoulder_score.html | ||
Latest revision as of 13:25, 30 September 2022
Objective[edit | edit source]
A questionnaire of shoulder pain and function. it was devised in 1996 (Dawson, Fitzpatrick, & Carr, 1996) for assessing the outcomes of shoulder surgery and later was used for degenerative conditions (excluding conditions of shoulder instability[1].
Intended Population[edit | edit source]
The OSS was designed to assess the outcome of all shoulder surgeries with the exception of instability surgery.
Method of Use[edit | edit source]
It contains 12 items, each with 5 answers. starting with 1 (best/fewest symptoms) to 5 (worst/most severe) which is awarded to correspond to the patient's symptoms. The total gives a minimum score of 12 and a maximum of 60. A higher score implies a greater degree of disability.
In 2009 the scoring method for the OSS was modified so that each of the 12 items is scored from 4 (best/fewest symptoms) to 0 (worst/most severe) [2].
Reference[edit | edit source]
The total score ranges from 48 to 0, after the modification of the score in 2009, a lower score indicates a greater degree of disability.
Reliability[edit | edit source]
the score was found to have a great interrater reliability and test-retest reliability[1].
Validity[edit | edit source]
Evidence suggested the validity of OSS to measure the degree of disability and detect the possible outcomes of shoulder surgery [1].
Responsiveness[edit | edit source]
it was stated that the sensitivity of the OSS can detect the smallest of changes that might happen in response to treatment interventions.[1]
Links[edit | edit source]
Oxford Shoulder Score http://www.orthopaedicscore.com/scorepages/oxford_shoulder_score.html
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 Younis F, Sultan J, Dix S, Hughes PJ. The range of the Oxford Shoulder Score in the asymptomatic population: a marker for post-operative improvement. The Annals of The Royal College of Surgeons of England. 2011 Nov;93(8):629-33.
- ↑ Younis F, Sultan J, Dix S, Hughes PJ. The range of the Oxford Shoulder Score in the asymptomatic population: a marker for post-operative improvement. The Annals of The Royal College of Surgeons of England. 2011 Nov;93(8):629-33.