Obturator Nerve
Original Editor - Jin Yoo
Top Contributors - Jin Yoo, Lucinda hampton, Leana Louw, Mariam Hashem and Kim Jackson
Description [1][edit | edit source]
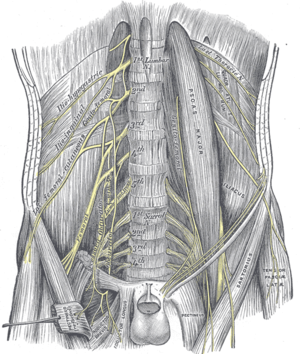
The obturator nerve arises from the lumbar plexus on the posterior abdominal wall and descends within the psoas muscle, emerging from the medial margin of the muscle to enter the pelvis. The nerve path continues by following along the lateral wall of the pelvis, passing through the obturator canal, to enter the medial compartment of the thigh. From here the nerve divides into the anterior and posterior branch which are separated by the adductor brevis muscle.
- The posterior branch travels underneath the adductor muscle along the anterior surface of the adductor magnus muscle, innervating the obturator externus, adductor brevis, as well as part of the adductor magnus muscle that is attached to the linea aspera.
- On the anterior surface of the adductor brevis muscle the anterior branch travels underneath the pectineus and adductor longus muscles to innervate the adductor longus, gracilis, and adductor brevis muscles. This branch also often contribute to the pectineus muscle. The cutaneous branches innervate the skin on the medial thigh.
Root[edit | edit source]
L2 - L4
Branches[edit | edit source]
Posterior Branch
Anterior Branch
Cutaneous Branch
Function [3][edit | edit source]
Motor[edit | edit source]
- Obturator Externus
- Adductor Longus
- Adductor Brevis
- 1/2 Adductor Magnus (the adductor portion)
- Gracilis
- Pectineus (occasional twig)
Sensory[edit | edit source]
- Hip joint
- Knee joint
- Medial skin over adductors (contributes together with saphenous and medial femoral cutaneous nerve)
Clinical Relevance [4][edit | edit source]
Injury to the nerve is rare as it lies deep within the pelvis and medial thigh. It can be damaged through direct injury to the nerve or to surrounding muscle tissue. Mild damage to the obturator nerve can be treated with physical therapy. More severe cases may require surgery.
Injury may be caused by:
- Nerve being stretched during surgery
- Entrapment within the obturator canal
- Compression during pregnancy
- Car or household accident
- Abdominal surgery[5]
- Athletes may present with pain that may be brought on by exercise, often sports involving a lot or running and twisting. They may have been predisposed to this injury by previous pelvic trauma or surgery.[6]
In mild damage physiotherapy treatment is employed. More severe cases may require surgery with follow up rehab physiotherapy.[5] Axonal growth is at about 1mm per day.[7]
Symptoms of Obturator Neuropathy:[edit | edit source]
- sensory alteration in medial thigh
- pain & paresthesias may extend from hip to knee along the medial aspect of the thigh
- extension or lateral leg movement can increase pain
- may have trouble walking or experience leg weakness due to problems adducting the ipsilateral hip
Signs of Obturator Neuropathy:[edit | edit source]
- weak hip adductors on affected side
- wasting of medial thigh
- abnormal abduction of hip during ambulation resulting in a circumducting, wide-based gait
- area of sensory loss or alteration in the mid and lower third of the medial thigh which sometimes may extend below the knee
- ipsilateral loss of the hip adductor tendon reflex (test against asymptomatic leg as is not always present in healthy population)
Assessment [4][edit | edit source]
- Needle EMG to confirm acute/chronic denervation of hip adductors excluding other lower extremity muscles such as iliopsoas or quadriceps
- CT, MRI, or ultrasound imaging when intra-pelvic mass lesions are suspected of entrapping the nerve
Treatment[edit | edit source]
| Tipton JS, 2008 [8] |
|
| Sorenson EJ. Chen JJ. Daube JR. 2002 [9] |
|
| Bradshaw C. McCrory P. Bell S. Brukner P. 1997 [10] |
|
References[edit | edit source]
- ↑ Drake, Richard, et al. Gray's Anatomy for Students. 3rd Edition. Philadelphia: Churchill Livingstone/Elsevier. 2015.
- ↑ Dr. Nabil Ebraheim. Obturator Nerve Anatomy - Everything You Need To Know - Dr. Nabil Ebraheim. Available from: https://www.youtube.com/watch?v=Z-txhI4uqqM [last accessed 22/02/2019]
- ↑ Whitaker RH. Borley NR. Instant Anatomy. Oxford: Blackwell Science Ltd.. 2000.
- ↑ 4.0 4.1 Busis NA. Femoral and obturator neuropathies. Neurologic Clinics 1999; 17: 633-53.
- ↑ 5.0 5.1 Healthline. Obturator nerve. Available from: https://www.healthline.com/human-body-maps/obturator-nerve#1 (last accessed 19.3.2019)
- ↑ Tipton JS. Obturator neuropathy. Current reviews in musculoskeletal medicine. 2008 Dec 1;1(3-4):234-7. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2682412/ (last accessed 19.3.2019)
- ↑ PM&R knowledge. PERIPHERAL NEUROLOGICAL RECOVERY AND REGENERATION. Available from: https://now.aapmr.org/peripheral-neurological-recovery-and-regeneration/ (last accessed 19.3.2019)
- ↑ Tipton JS. Obturator neuropathy. Current Reviews in Musculoskeletal Medicine 2008; 1: 234-7.
- ↑ Sorenson EJ. Chen JJ. Daube JR. Obturator neuropathy: causes and outcome. Muscle & Nerve 2002; 25: 605-7.
- ↑ Bradshaw C. McCrory P. Bell S. Brukner P. Obturator neuropathy: a cause of chronic groin pain in athletes. American Journal of Sports Medicine 1997; 25: 402-8.
- ↑ Brian Ableson. Flossing the Obturator Nerve - Amazing Results. Available from: https://www.youtube.com/watch?v=VEbVmzcIiv8 [last accessed 22/02/2019]