Neck Pain: Clinical Practice Guidelines
Original Editors - Chad Adams, Jacob Melnick, & Tyler Shultz
Lead Editors Tyler Shultz, Kim Jackson, Cindy John-Chu, Angeliki Chorti, Alexandra Malzer, Eric Robertson, Dorian Mars, Admin, Jacob Melnick, Evan Thomas, Zachary Cooper, WikiSysop, Albert Alabaster, Scott Buxton, Simisola Ajeyalemi, Agoro Bukola Zainab, Rachael Lowe, Tony Lowe, Nupur Smit Shah and Chad Adams
Discussion & Background[edit | edit source]
The purpose of these clinical guidelines it to describe the new evidence based physical therapy practices including pathoanatomical features, examination, diagnosis/classification, intervention and treatment recommendations for musculoskeletal disorders related to neck pain. In 2017 The Orthopaedic Section of the American Physical Therapy Association (APTA) revised the previous clinical practice guidelines of neck pain from 2008 and produced a new summary of recommendations and guidelines from current peer-reviewed literature (Blanpied et al.,2017).
Neck pain lacks a common clinical definition (Moffett et al,.2006). The most common type is non-specific neck pain defined as ‘’pain with a postural or mechanical basis, often called cervical spondylosis’’ (Binder et al., 2008). The 7 most common types of neck pain are: Muscle pain, muscle spasm, headache, facet joint pain, nerve pain, referred pain and bone pain each with their own causation, diagnosis and treatment (Harvard health publishing., 2018). Neck pain is becoming increasingly common throughout the world (Hoy et al 2010) with around two thirds of people experiencing neck pain at one moment in their life. The prevalence of neck pain varies largely between studies with a ‘’mean point prevalence of 7.6% and mean lifetime prevalence of 48.5%’’(Binder et al,.2007). Most studies indicate a higher incidence of neck pain among women (Hoy et al,.2011), if you suffer from anxiety or depression (Elbinoune et al,.2016) and if you are an office worker with poor position of the screen and keyboard (Hush et al.,2009).
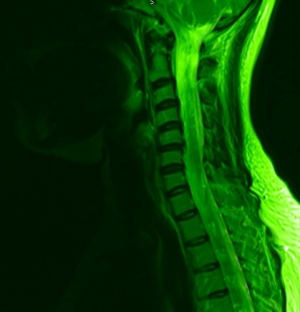
ANATOMY:
Bones and joints- The neck consists of 7 bones C1-C7. The most common neck pain caused by problems to the bone is osteoarthritis with wear in cartilage between the joints causing the bones to rub together producing pain and stiffness (Abu-Naser et al,.2016). The bones are linked together by facet joints these are small joints between your vertebrae.
Muscles, tendons and ligaments- The large muscles of the neck such as the sternocleidomastoid and the trapezius enable gross motor movements in the neck (Veritas Health,.2021). The most common pain produced by these structures is a neck strain which affects the cervical muscles and tendons or a sprain which affects the ligaments overstretching/tearing these structures.
Nerves- Cervical spine nerves provide functional control and sensation to different parts of the body based on the spinal level at which they sit. When a nerve is damaged/trapped sensation such as tingling is often felt in the upper extremities aiding identification of the damaged nerve.
Diagnosis & Classification Recommendations[edit | edit source]
Diagnosis and Classification of Patients with neck pain (Grade: B)
Clinical findings such as motion limitations in the cervical and upper thoracic regions, headaches, referred pain, and special test results can be useful in classifying a patient into one of the following International Statistical Classification of Diseases, and Related Health Problems (ICD) categories: cervicalgia, pain in thoracic spine, headaches, cervico-cranial syndrome, sprain and strain of the cervical spine, spondylosis with radiculopathy, and cervical disc disorder with radiculopathy. Patents can also be placed in a related impairment based category of the International Classification of Functioning, Disability, and Health (ICF). The groups of the ICF include: neck pain with mobility impairments, neck pain with headaches, neck pain with movement coordination impairments, and neck pain with radiating pain. Physical examination measures that are useful in the classification of the ICD and ICF models are listed below:
I. ICD- Cervicalgia / ICF- pain with mobility impairments
a. Cervical Active Range of Motion
b. Cervical and Thoracic segmental mobility
II. ICD- Headaches or cervico-cranial syndrome / ICF- Neck Pain with Headaches
a. Cervical Active Range of Motion
b. Cervical segmental Mobility
c. Cranial Cervical Flexion Test
III. ICD- Sprain and Strain of cervical spine / ICF- Neck Pain with Movement Coordination impairments
a. Cranial Cervical Flexion Test
b. Deep Neck Flexor Endurance
IV. ICD- Spondylosis with radiculopathy or cervical disc disorder with radiculopathy / ICF- Neck Pain with Radiating Pain
a. Upper Limb Tension Test (ULLT)
b. Spurling’s Test
c. Distraction Test
Differential Diagnosis of patients with neck pain (Grade: B)
If a patient’s impairments fall outside of the ranges of the classification system or the interventions do not fail to improve the symptoms the clinician should consider serious pathological conditions or psychosocial factors as being a possible explanations to the patient’s pain.
Examination Recommendations[edit | edit source]
The use of Outcome Measures (Grade: A)
Validated self-report questionnaires should be used with patients complaining of neck pain. The Neck Disability Index and the Patient Specific Functional Scale are two examples of these questionnaires. The main reason for this recommendation is that these tools establish a baseline status for pain, function, and disability that can be used later in intervention selection and goal tracking.
The consideration of certain risk factors that can predispose a patient to chronic neck pain (Grade: B)
Some risk factors have been shown to predispose a patient for chronic neck pain and should be considered by a clinician during the initial examination. These risk factors include:
- Age > 40 yrs.
- Coexisting LBP (Low Back Pain)
- History of neck pain
- Frequent cycling
- Loss of strength in hands
- Worrisome attitude
- Poor quality of life
- Decreased vitality
The consideration of pathoanatomical features (Grade: F)
Although the cause of neck pain may often be related to degenerative changes or pathology the tissue causing the pain is most often unknown. Therefore, a clinician must examine for muscle, connective tissue, and nervous tissue dysfunction during their examination and evaluation.
Intervention & Treatment Recommendations[edit | edit source]
Cervical Manipulation/Mobilizations alongside coordination, strengthening, & endurance exercises (Grade: A)
Manipulation and mobilization techniques including thrust and not thrust motions have been shown to reduce symptoms in patient with neck pain and headaches. Exercises that improve the coordination, strength and endurance of cervical musculature have also been shown improvements in this patient group. Although each of these techniques are beneficial, the patients that receive a combination of the two treatments show the most reduction in symptoms.
Patient Education and Reassurance are important throughout treatment. (Grade: A)
Especially following a traumatic event, patients should be encouraged to return to pre-accident function levels as quickly as safely possible. They should also be reassured that neck pain patients normally have a good prognosis and regaining normal function is highly likely.
The use of upper quarter and nerve mobilization procedures and the use of traction can be useful in the treatment of patients with neck pain. (Grade: B)
These interventions have been shown beneficial and are even more effective when paired with manual therapy and exercise.
Use of Thoracic Mobilization/Manipulation (Grade: C)
The use of thrust manipulations and mobilizations can reduce symptoms in patients with neck and neck related arm pain.
Use of Stretching and centralization techniques (Grade: C)
Stretching involved musculature can be beneficial for patients with neck pain. Movements that promote centralization of pain have also shown results in reducing symptoms in patients with neck pain
Activity Limitations (Grade: F)
The patient should be limited to functional activity that does not cause an increase in symptoms throughout the treatment period. This helps the clinician to assess changes in the patients level of function during an episode of care.
References[edit | edit source]