McKenzie Method
Original Editor - Jessie Tourwe as part of the Vrije Universiteit Brussel's Evidence-based Practice project
Top Contributors - Admin, Matt Huey, Kim Jackson, Denys Nahornyi, Jessie Tourwe, Lucinda hampton, Oluwatosin Osasona, Venus Pagare, George Prudden, Linde Van Droogenbroeck, WikiSysop, Rucha Gadgil, Amanda Ager, Evan Thomas, Ilona Malkauskaite, Samuel Adedigba, Manisha Shrestha, 127.0.0.1, Samuel Winter, Scott Buxton and Carina Therese Magtibay
Description/Definition[edit | edit source]
The McKenzie method or mechanical diagnosis and therapy (MDT) is a system of diagnosis and treatment for spinal and extremity musculoskeletal disorders.
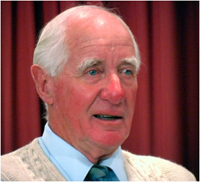
MDT was introduced in 1981 by Robin McKenzie (1931–2013), a physical therapist from New Zealand [1][2][3][4].
A feature of the method is emphasizing patient empowerment and self-treatment. MDT categories patients complaints not on anatomical basis, but subgroups them by the clinical presentation of patients [5]. The reliability of MDT classifications have been confirmed by several studies [6][7][8].
Watch him in action in the video below
MDT is commonly utilized to treat symptoms in the spine with patients often experiencing symptoms in the extremities that originated from the spine. The goal is to centralize the symptoms back to the spine. The phenomenon of Centralization is the symptoms movement from the distal segments of body to the proximal. Advent of centralization is a good signal and speaks of a directional preference. And in contrast, Peripheralization - the movement of pain from the spine to the extremities, indicates a worsening [10].
MDT exists of 4 steps:
- Assessment: The clinician takes a history of symptoms along with what activities either aggravate or relieve the symptoms. Next, a movement assessment is performed to determine if the patient has any movement loss, along with what the symptoms do with the movement. Then the clinician has the patient perform specific repeated or sustained movements to determine the effect on the symptoms.
- Classification: Based on assessment the symptomatic response during the repeated or sustained movement testing, a classification is given. Most patient's symptoms are classified into: derangement syndrome, dysfunction syndrome, postural syndrome or other. The choice of exercises in MDT is based upon the direction that causes the symptoms to decrease, centralize, or abolish.
- Treatment: Treatment consists of first finding a repeated or sustained movement that reduces and/or abolishes the symptoms. Next, the goal is to maintain this improvement for several days. Finally, the patient performs recovery of function, which is having the patient do once pain provoking movements to determine if they are now pain-free.
- Prevention: The prevention step consists of educating and encouraging the patient to exercise regularly and self-care.[1][2][11][12]
The exercise that is given typically will be in one direction based upon the symptomatic response. The exercise may be a repeated movement or a sustained position, it could also require reaching end range or sometimes mid-range, just depending on what happens with the symptoms. A single direction of repeated movements or sustained postures leads to sequential and lasting abolition of all distal referred symptoms and subsequent abolition of any remaining spinal pain[12].
Studies have shown that while this method may not be superior to other rehabilitation interventions for pain and disability reduction in patients with acute lower back pain, there is moderate to high-quality evidence supporting the superiority of MDT over other methods in reducing both in patients with chronic lower back pain. A recent study that evaluated the effectiveness of MDT compared to manual therapy in the management of patients with chronic low back pain concluded that MDT is a successful treatment to decrease pain in the short term and enhance function in the long term[13]. One study showing significantly improved cervical posture of people with a forward head posture[14].
Classification[edit | edit source]
Patients are classified into four groups according to the mechanical and symptomatic response to repeated movements and/or sustained positions. Classifications are not always given at the initial evaluation, but in some cases, it may be 3-5 visits before a classification is confirmed.
The video below (4 minutes) gives some salient points to consider when using this approach.
Each syndrome demands a different management approach.
Below you will find the four categories of MDT classification with their descriptions.[16][17]
Derangement Syndrome[edit | edit source]
- This is the more common and known syndrome
- Inconsistency and change is the major characteristic of this syndrome
- Symptoms may be local, referred, radicular or a combination, the symptoms could also move from side to side or proximal to distal.
- Symptoms can be constant or intermittent and could vary through the day
- The onset can be sudden, with no known cause, or gradual over time
- The symptoms can be influenced by postures or normal daily activities
- Directional Preference is a hallmark of derangement syndrome, which a specific repeated movement or sustained position causes a relevant improvement in symptoms.
- Treatments involve specific movements that cause the pain to decrease, centralize and/or abolish.[12]
Dysfunction Syndrome[edit | edit source]
- Refers to pain which is a result of mechanical deformation of structurally impaired tissues like scar tissue or adhered or adaptively shortened tissue.
- The symptoms must be present for 8-12 weeks, this time allowed the tissues to deform
- The pain is always intermittent and arises at the end range of a restricted movement.
- The treatment includes: repeated movements in the direction of the dysfunction or in the direction that reproduces the pain. The aim is to remodel that tissue, which limits the movement, through exercises so that it becomes pain-free over time[12].
Postural Syndrome[edit | edit source]
- Refers to pain which occurs due to a mechanical deformation of normal soft tissue from prolonged end range loading of periarticular structures.
- The pain arises during static positioning of the spine: for example sustained slouched sitting.
- The pain disappears when the patient is moved out of the static position.
- There is no pain with performing movement or activity.
- The treatment includes: patient education, correction of the posture by improving posture by restoring lumbar lordosis, avoiding provocative postures and avoid prolonged tensile stress on normal structure[12]
Other or non-mechanical Syndrome[edit | edit source]
There are patients who do not fit within one of the three mechanical syndromes but who demonstrate symptoms and signs of other pathologies.[12] Confirming a classification can take 3-5 visits to ensure all planes and forces are exhausted.
- Spinal stenosis
- Hip disorders
- Sacroiliac disorders
- Low back pain in pregnancy
- Chronic pain syndrome
- Mechanically inconclusive
- Mechanically unresponsive radiculopathy
- Structurally compromised
- Post-surgical problems
- Trauma/Recovering trauma
Just because a patient is classified into the "Other" category, does not mean they may not change over time. Time is often a factor in the determination of treatment.
This classification shows strong inter-rater reliability amongst physiotherapist trained in MDT.[16][17]
Management[edit | edit source]
Unlike other exercises for treating low back pain meant for muscle strengthening, stability and restoring range of motion, MDT exercises are meant to directly diminish or even eliminate the patients symptoms. [12] This effect is accomplished by providing a corrective mechanical directional movement. Patients who have a directional preference have been shown to have improvements in lumbar pain.[18] MDT educates patients regarding movement and position strategies can reduce pain. A cautious progression of repeated forces and loads is used in this method.[19] The exercises may be uncomfortable at first, but after some repetitions the symptoms will decrease.
Exercise Force Progression[edit | edit source]
The use of force progression may be needed to obtain the desired outcomes. The use of each progression is dependent on how the patient's symptoms respond.
- Static: Mid Range -> Static End Range
- Dynamic: Mid Range -> End Range-> Self Overpressure
- Clinician Generated: Patient to End Range -> Overpressure -> Therapist mobilisation -> Manipulation
Exercise Prescription[edit | edit source]
The prescription of exercises is dependent upon the patient's response with the clinician. The following is an example of a prescription given to a patient based upon favorable response during the treatment session.
- 10 reps of the motion every 2 hours
- Take motion to end range
- Postural awareness
- Follow-up in next 24-48 hours to assess progress
At the follow up session, the clinician will assess the patient's baseline symptoms and response to the given exercise/activity. If the patient returns and is significantly better, often no change is given to their prescribed activities. If the patient returns the same, then force progressions or alternatives may be explored. If the patient returns worse, reassess the patient.
Examples of Common MDT Exercises[edit | edit source]
These are common exercises or movements used in the treatment for patients with lumbar pain symptoms. The selection of a movement is determined based upon the assessment and patient's symptomatic response. The selection of exercises or movements is based upon how the symptoms respond during and after the exercise/movement.
Lying Prone[edit | edit source]
This exercise is simple but can be effective for acute or pain sensitive patients. The patient lays on their stomach with the head to one side or the other. This position can create a lordosis of the lumbar spine. The patient maintains this position for at least 3 minutes to determine what the symptoms are doing. Often in severe cases, this position may be enough to elicit a decrease in symptoms to allow the patient to progress to sustained or repeated movements.
Extension in Lying[edit | edit source]
The patient lies on their stomach with the hands near the shoulders (as if they are ready to perform a push-up). Next, the patient presses their shoulders up toward the ceiling, while maintaining the hips and legs on the table. The goal is to reach full end range of extension then return to the table, however, this motion may be limited due to increased pain or obstruction. If this is the case, then the patient returns to the table. Typically, 10 repetitions are performed at a steady, rhythmical pace. Each time trying to push further to end range while listening to the symptoms. If the symptoms are decreasing, centralizing, or being abolished, then the exercise is repeated as many times as needed. This procedure is the most important and effective in the treatment of derangement as well as extension dysfunction [3].
Prone Extension Modifications:
- Therapist applies PA pressure whilst patient extends
- Therapist mobilises the spine whilst patient extends
- With hips off center , start with hips away from painful side, repeate press-ups 10-15 times
- As above, but with lateral overpressure through ribs and iliac rest
Extension in Standing[edit | edit source]
This exercise is similar to extension in lying, but performed in standing. This may be performed if extension in lying increases symptoms or the patient cannot tolerate laying on their stomach. The patient stands up straight with their feet apart, to remain a stable position. The hands are placed on the lumbar region, in the area of the spina iliaca posterior superior. His hands fixate the pelvis while the patient leans backwards. The patient has to lean backwards as far as possible. This exercise has to be repeated 10 times. If balance is an issue or the patient needs a more extension, lean against a sturdy surface such as a cabinet or heavy desk. It can have similar effects on derangement and dysfunction as extension in lying depending on the symptomatic response.
Evidence supporting MDT[edit | edit source]
Classification Reliability
MDT Recommended as a Treatment Approach
- Classification of patients with low back-related leg pain: a systematic review
- Effectiveness of the McKenzie Method of Mechanical Diagnosis and Therapy for Treating Low Back Pain: Literature Review With Meta-analysis
- Treatment Effect Sizes of Mechanical Diagnosis and Therapy for Pain and Disability in Patients With Low Back Pain: A Systematic Review
Prediction of Outcomes
- Centralization and directional preference: An updated systematic review with synthesis of previous evidence
- Association between directional preference and centralization in patients with low back pain
Treatment Efficacy
- The McKenzie method compared with manipulation when used adjunctive to information and advice in low back pain patients presenting with centralization or peripheralization: a randomized controlled trial
- Does it matter which exercise? A randomized control trial of exercise for low back pain
Presentations[edit | edit source]
Watch these videos below (around 40 minutes each) to get a better appreciation of the approach,
References[edit | edit source]
- ↑ 1.0 1.1 McKenzie Instytute International. What is the McKenzie Method? Available from: https://mckenzieinstitute.org/patients/what-is-the-mckenzie-method/ (accessed 24 September 2020)
- ↑ 2.0 2.1 Machado LAC, Souza MS, Ferreira PH, Ferreira ML. The McKenzie Method for Low Back Pain: A Systematic Review of the Literature With a Meta-Analysis Approach. Spine 2006;31(9):254–262.
- ↑ 3.0 3.1 McKenzie R., The lumbar spine: Mechanical diagnosis and therapy. Wellington: Spinal publications New-Zealand, 1981.
- ↑ Physiotherapy NewZealand Physios mourn passing of legend - Robin McKenzie Available from: https://100yearsofphysio.org.nz/document-library/obituaries/physios-mourn-passing-of-legend-robin-mckenzie/#.Xc45LDIza-U (last accessed 15.11.2019)
- ↑ Werneke M, Hart D. Categorizing patients with occupational low back pain by use of the Quebec Task Force Classification system versus pain pattern classification procedures: discriminant and predictive validity. Physical Therapy. 2004;84(3):43–54.
- ↑ Takasaki H, Okuyama K, Rosedale R. Inter-examiner classification reliability of Mechanical Diagnosis and Therapy for extremity problems - Systematic review. Musculoskelet Sci Pract 2017;27:78-84.
- ↑ Tagliaferri SD, Angelova M, Zhao X, Owen PJ, Miller CT, Wilkin T, Belavy DL. Artificial intelligence to improve back pain outcomes and lessons learnt from clinical classification approaches: three systematic reviews. NPJ Digit Med 2020;3:93.
- ↑ Clare HA, Adams R, Maher CG. Reliability of detection of lumbar lateral shift. Journal of Manipulative and Physiological Therapeutics 2003;26(8),476–480.
- ↑ The original McKenzie Robin McKenzie on Close Up Available from: https://www.youtube.com/watch?v=8BXDe5fcp7I (last accessed 15.11.2019)
- ↑ Davies C L, Blackwood C M, The centralization phenomen: it`s role in the assessement and management of low back pain, BCMJ. 2004;46:348-352.
- ↑ Garcia AN, Gondo FL, Costa RA, Cyrillo FN, Silva TM, Costa LC, Costa LO. Effectiveness of the back school and McKenzie techniques in patients with chronic non-specific low back pain: a protocol of a randomized controlled trial, BMC Musculoskeletal Disorders 2011;12:179
- ↑ 12.0 12.1 12.2 12.3 12.4 12.5 12.6 May S, Donelson R. Evidence-informed management of chronic low back pain with the McKenzie method.Spine J. 2008;8(1):134-41.
- ↑ Namnaqani FI, Mashabi AS, Yaseen KM, Alshehri MA. The effectiveness of McKenzie method compared to manual therapy for treating chronic low back pain: a systematic review. J Musculoskelet Neuronal Interact. 2019;19(4):492-9.
- ↑ Mann SJ, Singh P. McKenzie Back Exercises. InStatPearls [Internet] 2019 Apr 1. StatPearls Publishing. Available from: https://www.ncbi.nlm.nih.gov/books/NBK539720/ (last accessed 15.11.2019)
- ↑ The McKenzie Institute USA What Physical Therapy Clinicians Need to Know About The McKenzie Method Available from: https://www.youtube.com/watch?v=j2lOZBNkWZ8 (last accessed 15.11.2019)
- ↑ 16.0 16.1 Hefford C. McKenzie classification of mechanical spinal pain: Profile of syndromes and directions of preference. Manual therapy 2008 Feb; 13 (1): 75-81.
- ↑ 17.0 17.1 Clare HA, Adams R et al. Reliability of McKenzie classification of patients with cervical or lumbar pain. Journal of manipulative and physiological therapeutics 2005 Feb; 28(2): 122-127.
- ↑ Long A, Donelson R, Fung T. Does it matter which exercise? A randomized control trial of exercise for low back pain. Spine (Phila Pa 1976). 2004 Dec 1;29(23):2593-602. doi: 10.1097/01.brs.0000146464.23007.2a. PMID: 15564907.
- ↑ Liebenson C. Rehabilitation of the spine: a practitioner’s manual, second edition. Lipincott Williams & Wilkins, Philadelphia (2007).