Morel-Lavallée lesion: Difference between revisions
No edit summary |
(PP page links added and categories added) |
||
| Line 19: | Line 19: | ||
== Pathophysiology == | == Pathophysiology == | ||
[[File:Morel-lavallee-illustrations.jpg|thumb|450x450px|Case courtesy of Dr Matt Skalski, <a href="https://radiopaedia.org/?lang=us">Radiopaedia.org</a>. From the case <a href="https://radiopaedia.org/cases/22762?lang=us">rID: 22762</a>]] | [[File:Morel-lavallee-illustrations.jpg|thumb|450x450px|Case courtesy of Dr Matt Skalski, <a href="https://radiopaedia.org/?lang=us">Radiopaedia.org</a>. From the case <a href="https://radiopaedia.org/cases/22762?lang=us">rID: 22762</a>]] | ||
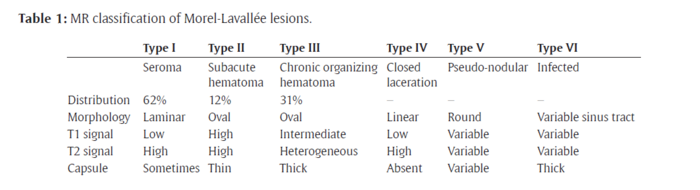
MLL occurs due to shearing forces which separate the skin and subcutaneous tissue from the deep fascia, causing a potential space<ref name=":0" /><ref name=":1" /><ref name=":3" /><ref name=":4" /><ref name=":6" /><ref name=":8">Weiss NA, Johnson JJ, Anderson SB. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4427222/pdf/wjem-16-438.pdf Morel-lavallee lesion initially diagnosed as quadriceps contusion: ultrasound, MRI, and importance of early intervention]. Western Journal of Emergency Medicine. 2015 May;16(3):438.</ref><ref name=":9">Cruz N, Jiménez R. [https://reader.elsevier.com/reader/sd/pii/S2210261221002340?token=C80C41D90F7CEE3ACB97BCC5E93E1B4C35747C6360CCC9420F281E1AAAB782FC4FE027E1EABB65CE512F7BAB5AF7354A&originRegion=eu-west-1&originCreation=20221125082018 Morel-Lavallée lesion diagnosed 25 years after blunt trauma]. International Journal of Surgery Case Reports. 2021 Apr 1;81:105733.</ref>. Damage to the lymphatic and blood vessels leads to an accumulation of blood and lymph<ref name=":0" /><ref name=":2" /><ref name=":3" /><ref name=":6" /><ref name=":8" /> and necrotic fat<ref name=":0" /><ref name=":2" /><ref name=":6" /><ref name=":11">Cochran GK, Hanna KH. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5207285/pdf/10.1177_1558944716646776.pdf Morel-Lavallee lesion in the upper extremity.] Hand. 2017 Jan;12(1):NP10-3.</ref> in the potential space, causing a haematoma or seroma<ref name=":8" />. Blood will start to be reabsorbed over time leaving a serosanguinous fluid surrounded by a haemosiderin layer<ref name=":1" />. Inflammation is then induced by the haemosiderin layer leading to a fibrous capsule<ref name=":1" /><ref name=":9" />. This fibrous capsule prevents more fluid reabsorption, initiating a chronic MLL<ref name=":2" />. | MLL occurs due to shearing forces which separate the skin and subcutaneous tissue from the deep fascia, causing a potential space<ref name=":0" /><ref name=":1" /><ref name=":3" /><ref name=":4" /><ref name=":6" /><ref name=":8">Weiss NA, Johnson JJ, Anderson SB. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4427222/pdf/wjem-16-438.pdf Morel-lavallee lesion initially diagnosed as quadriceps contusion: ultrasound, MRI, and importance of early intervention]. Western Journal of Emergency Medicine. 2015 May;16(3):438.</ref><ref name=":9">Cruz N, Jiménez R. [https://reader.elsevier.com/reader/sd/pii/S2210261221002340?token=C80C41D90F7CEE3ACB97BCC5E93E1B4C35747C6360CCC9420F281E1AAAB782FC4FE027E1EABB65CE512F7BAB5AF7354A&originRegion=eu-west-1&originCreation=20221125082018 Morel-Lavallée lesion diagnosed 25 years after blunt trauma]. International Journal of Surgery Case Reports. 2021 Apr 1;81:105733.</ref>. Damage to the lymphatic and blood vessels leads to an accumulation of blood and lymph<ref name=":0" /><ref name=":2" /><ref name=":3" /><ref name=":6" /><ref name=":8" /> and necrotic fat<ref name=":0" /><ref name=":2" /><ref name=":6" /><ref name=":11">Cochran GK, Hanna KH. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5207285/pdf/10.1177_1558944716646776.pdf Morel-Lavallee lesion in the upper extremity.] Hand. 2017 Jan;12(1):NP10-3.</ref> in the potential space, causing a haematoma or seroma<ref name=":8" />. Blood will start to be reabsorbed over time leaving a serosanguinous fluid surrounded by a haemosiderin layer<ref name=":1" />. [[Inflammation Acute and Chronic|Inflammation]] is then induced by the haemosiderin layer leading to a fibrous capsule<ref name=":1" /><ref name=":9" />. This fibrous capsule prevents more fluid reabsorption, initiating a chronic MLL<ref name=":2" />. | ||
MLL are often associated with pelvic or acetabular fractures but can also occur without a fracture<ref name=":7" />. | MLL are often associated with pelvic or acetabular fractures but can also occur without a fracture<ref name=":7" />. | ||
| Line 28: | Line 28: | ||
== Clinical Presentation == | == Clinical Presentation == | ||
[[File:Morel-lavallee sites.jpg|thumb|400x400px|Case courtesy of Dr Matt Skalski, <a href="https://radiopaedia.org/?lang=us">Radiopaedia.org</a>. From the case <a href="https://radiopaedia.org/cases/22762?lang=us">rID: 22762</a>]] | [[File:Morel-lavallee sites.jpg|thumb|400x400px|Case courtesy of Dr Matt Skalski, <a href="https://radiopaedia.org/?lang=us">Radiopaedia.org</a>. From the case <a href="https://radiopaedia.org/cases/22762?lang=us">rID: 22762</a>]] | ||
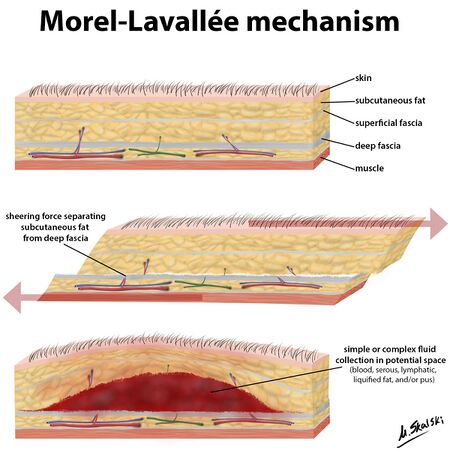
MLL occurs most commonly over the greater trochanter (>60% of cases)<ref name=":0" /><ref name=":2" /> <ref name=":4" /><ref name=":5" /><ref name=":6" /><ref name=":9" />, proximal femur<ref name=":0" /><ref name=":1" /><ref name=":4" />, buttock<ref name=":1" /><ref name=":2" /><ref name=":4" />, knee<ref name=":2" /><ref name=":4" /><ref name=":5" /><ref name=":9" /> and in rare cases, the lumbar region<ref name=":1" /><ref name=":2" /><ref name=":5" /><ref name=":9" />. It can also occur at the scapula<ref name=":1" /><ref name=":5" />. Delayed presentation (months or years) can occur in up to ⅓ of patients<ref name=":0" /><ref name=":6" />. The most common signs and symptoms include: | MLL occurs most commonly over the greater trochanter (>60% of cases)<ref name=":0" /><ref name=":2" /> <ref name=":4" /><ref name=":5" /><ref name=":6" /><ref name=":9" />, proximal [[femur]]<ref name=":0" /><ref name=":1" /><ref name=":4" />, buttock<ref name=":1" /><ref name=":2" /><ref name=":4" />, [[knee]]<ref name=":2" /><ref name=":4" /><ref name=":5" /><ref name=":9" /> and in rare cases, the [[Lumbar Anatomy|lumbar]] region<ref name=":1" /><ref name=":2" /><ref name=":5" /><ref name=":9" />. It can also occur at the scapula<ref name=":1" /><ref name=":5" />. Delayed presentation (months or years) can occur in up to ⅓ of patients<ref name=":0" /><ref name=":6" />. The most common signs and symptoms include: | ||
* Compressible, fluctuant swollen area<ref name=":0" /><ref name=":1" /><ref name=":4" /><ref name=":6" /><ref name=":7" />. The fluctuant swelling is an essential clinical characteristic<ref name=":7" />. | * Compressible, fluctuant swollen area<ref name=":0" /><ref name=":1" /><ref name=":4" /><ref name=":6" /><ref name=":7" />. The fluctuant swelling is an essential clinical characteristic<ref name=":7" />. | ||
| Line 41: | Line 41: | ||
The necrotic tissue associated with the MLL is particularly susceptible to infection<ref name=":2" /> and if infection occurs, it can lead to | The necrotic tissue associated with the MLL is particularly susceptible to infection<ref name=":2" /> and if infection occurs, it can lead to | ||
* Cellulitis<ref name=":2" /> | * [[Cellulitis]]<ref name=":2" /> | ||
* Abscess<ref name=":2" /> | * Abscess<ref name=":2" /> | ||
* Osteomyelitis<ref name=":2" /> | * [[Osteomyelitis]]<ref name=":2" /> | ||
* Necrosis of underlying tissues due to pressure<ref name=":7" /> | * Necrosis of underlying tissues due to pressure<ref name=":7" /> | ||
== Classification == | == Classification == | ||
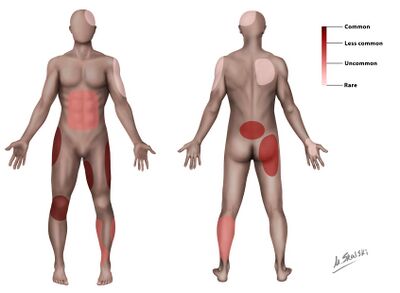
Mellado and Bencardino proposed a MRI classification and identified 6 types of MLL based on the lesion chronicity, appearance on MRI and tissue composition <ref name=":1" /><ref name=":10" /><ref name=":6" /><ref name=":7" />. The 6 types include the following: | Mellado and Bencardino proposed a [[MRI Scans|MRI]] classification and identified 6 types of MLL based on the lesion chronicity, appearance on MRI and tissue composition <ref name=":1" /><ref name=":10" /><ref name=":6" /><ref name=":7" />. The 6 types include the following: | ||
[[File:MRI classification morel lavallee.png|center|thumb|700x700px|De Coninck, T, Vanhoenacker, F and Verstraete, K. Imaging Features of Morel-Lavallée Lesions. Journal of the Belgian Society of Radiology. 2017; 101(S2): 15, pp. 1–8. DOI: <nowiki>https://doi.org/10.5334/jbr-btr.1401</nowiki>]] | [[File:MRI classification morel lavallee.png|center|thumb|700x700px|De Coninck, T, Vanhoenacker, F and Verstraete, K. Imaging Features of Morel-Lavallée Lesions. Journal of the Belgian Society of Radiology. 2017; 101(S2): 15, pp. 1–8. DOI: <nowiki>https://doi.org/10.5334/jbr-btr.1401</nowiki>]] | ||
| Line 60: | Line 60: | ||
Diagnosis of MLL should be based on the patient’s history, the physical examination and imaging<ref name=":9" />. | Diagnosis of MLL should be based on the patient’s history, the physical examination and imaging<ref name=":9" />. | ||
Ultrasound, MRI and CT scan can be used to diagnose MLL<ref name=":10" /><ref name=":6" /><ref name=":7" />. On ultrasound, the fluid mass is located anterior to the muscle but posterior to the hypodermis<ref name=":7" />. MRIs are particularly important in the diagnosis of MLL <ref name=":10" /><ref name=":7" /><ref name=":9" /> and help with differential diagnosis<ref name=":9" />. | [[Ultrasound Scans|Ultrasound]], [[MRI Scans|MRI]] and [[CT Scans|CT]] scan can be used to diagnose MLL<ref name=":10" /><ref name=":6" /><ref name=":7" />. On ultrasound, the fluid mass is located anterior to the muscle but posterior to the hypodermis<ref name=":7" />. MRIs are particularly important in the diagnosis of MLL <ref name=":10" /><ref name=":7" /><ref name=":9" /> and help with differential diagnosis<ref name=":9" />. | ||
MLLs are often missed (up to one third of cases)<ref name=":9" /> and untreated lesions can lead to complications such as infection<ref name=":3" /><ref name=":7" /> and chronic lesions<ref name=":9" />. Early diagnosis is very important to prevent infection and development of the capsule (chronic lesion)<ref name=":11" />. | MLLs are often missed (up to one third of cases)<ref name=":9" /> and untreated lesions can lead to complications such as infection<ref name=":3" /><ref name=":7" /> and chronic lesions<ref name=":9" />. Early diagnosis is very important to prevent infection and development of the capsule (chronic lesion)<ref name=":11" />. | ||
| Line 69: | Line 69: | ||
* Seroma<ref name=":9" /> | * Seroma<ref name=":9" /> | ||
* Soft tissue malignancy <ref name=":3" /><ref name=":4" /><ref name=":10" /><ref name=":9" /> | * Soft tissue malignancy <ref name=":3" /><ref name=":4" /><ref name=":10" /><ref name=":9" /> | ||
* Bursitis<ref name=":4" /><ref name=":10" /><ref name=":9" /> | * [[Bursitis]]<ref name=":4" /><ref name=":10" /><ref name=":9" /> | ||
* Abscess<ref name=":4" /> | * Abscess<ref name=":4" /> | ||
== Physiotherapy management == | == Physiotherapy management == | ||
Although physiotherapy cannot directly treat the MLL, it can help improve functional activities and reduce pain<ref name=":7" />. There is no specific physiotherapy protocol, as the physiotherapy management will depend on what the patient requires e.g. range-of-motion improvement, gait re-education or strengthening. Physiotherapy management depends on the severity of the lesion, the medical/surgical management and the amount of bed rest the patient had. A case study (2022) of a patient with a thigh MLL, found that physiotherapy significantly improved joint range-of-motion, strength, cardiovascular/pulmonary function and functional independence<ref name=":7" />. Another study (2021) found that physiotherapy was essential to get the best functional outcomes after surgery or conservative management<ref>Agrawal U, Tiwari V. [https://europepmc.org/article/NBK/nbk574532https://europepmc.org/article/NBK/nbk574532 Morel Lavallee Lesion].</ref>. | Although physiotherapy cannot directly treat the MLL, it can help improve functional activities and reduce pain<ref name=":7" />. There is no specific physiotherapy protocol, as the physiotherapy management will depend on what the patient requires e.g. range-of-motion improvement, [[gait]] re-education or [[Strength Training|strengthening]]. Physiotherapy management depends on the severity of the lesion, the medical/surgical management and the amount of bed rest the patient had. A case study (2022) of a patient with a thigh MLL, found that physiotherapy significantly improved joint range-of-motion, strength, cardiovascular/pulmonary function and functional independence<ref name=":7" />. Another study (2021) found that physiotherapy was essential to get the best functional outcomes after surgery or conservative management<ref>Agrawal U, Tiwari V. [https://europepmc.org/article/NBK/nbk574532https://europepmc.org/article/NBK/nbk574532 Morel Lavallee Lesion].</ref>. | ||
== Medical management == | == Medical management == | ||
| Line 93: | Line 93: | ||
<references /> | <references /> | ||
[[Category:Conditions]] | |||
[[Category:Pain]] | |||
[[Category:Musculoskeletal/Orthopaedics]] | |||
[[Category:Sports Medicine]] | |||
[[Category:Sports Injuries]] | |||
[[Category:Hip]] | |||
[[Category:Knee]] | |||
[[Category:Pelvis]] | |||
Revision as of 12:44, 25 November 2022
This article or area is currently under construction and may only be partially complete. Please come back soon to see the finished work! (25/11/2022)
Definition[edit | edit source]
A Morel-Lavallée lesion (MLL) was first described in 1853[1] [2]. It is a closed soft-tissue degloving injury[1][3][4][5][6] that usually occurs after blunt trauma[1][2][3][5]. In recent literature, it can also be referred to as Morel-Lavallée seroma or effusion, post-traumatic soft tissue cysts or post-traumatic extravasations[2].
Epidemiology and aetiology[edit | edit source]
These injuries are uncommon[2] and there is no consensus on the ratio of men to women. One source reported a 2:1 ratio[2] while another reported a 1:1 ratio[7].
These injuries occur due to blunt trauma after:
MLL can also be iatrogenic e.g. after abdominal liposuction or mammoplasty[1][2][6]
Pathophysiology[edit | edit source]
MLL occurs due to shearing forces which separate the skin and subcutaneous tissue from the deep fascia, causing a potential space[1][2][4][5][8][10][11]. Damage to the lymphatic and blood vessels leads to an accumulation of blood and lymph[1][3][4][8][10] and necrotic fat[1][3][8][12] in the potential space, causing a haematoma or seroma[10]. Blood will start to be reabsorbed over time leaving a serosanguinous fluid surrounded by a haemosiderin layer[2]. Inflammation is then induced by the haemosiderin layer leading to a fibrous capsule[2][11]. This fibrous capsule prevents more fluid reabsorption, initiating a chronic MLL[3].
MLL are often associated with pelvic or acetabular fractures but can also occur without a fracture[9].
Secondary risk factors for an MLL include female gender and BMI of over 25[1].
Clinical Presentation[edit | edit source]
MLL occurs most commonly over the greater trochanter (>60% of cases)[1][3] [5][6][8][11], proximal femur[1][2][5], buttock[2][3][5], knee[3][5][6][11] and in rare cases, the lumbar region[2][3][6][11]. It can also occur at the scapula[2][6]. Delayed presentation (months or years) can occur in up to ⅓ of patients[1][8]. The most common signs and symptoms include:
- Compressible, fluctuant swollen area[1][2][5][8][9]. The fluctuant swelling is an essential clinical characteristic[9].
- Pain[1][2][4][8]
- Stiffness[5][9]
- Cutaneous anaesthesia or hypothesia may be present[1][2][4][8]
- Ecchymosis may be present[9]
- Abrasions may be present[9]
- Secondary dermal changes e.g. discolouration, frank necrosis, drying/cracking[1][9]
Complications[edit | edit source]
The necrotic tissue associated with the MLL is particularly susceptible to infection[3] and if infection occurs, it can lead to
- Cellulitis[3]
- Abscess[3]
- Osteomyelitis[3]
- Necrosis of underlying tissues due to pressure[9]
Classification[edit | edit source]
Mellado and Bencardino proposed a MRI classification and identified 6 types of MLL based on the lesion chronicity, appearance on MRI and tissue composition [2][7][8][9]. The 6 types include the following:
Type I to III are the most common types with Type I being acute, type II, sub-acute and III, chronic[8].
A more basic acute vs chronic classification was proposed by Shen et al (2013)[2]. The lesion is considered chronic once a capsule is present[2].
Diagnosis and Imaging[edit | edit source]
Diagnosis of MLL should be based on the patient’s history, the physical examination and imaging[11].
Ultrasound, MRI and CT scan can be used to diagnose MLL[7][8][9]. On ultrasound, the fluid mass is located anterior to the muscle but posterior to the hypodermis[9]. MRIs are particularly important in the diagnosis of MLL [7][9][11] and help with differential diagnosis[11].
MLLs are often missed (up to one third of cases)[11] and untreated lesions can lead to complications such as infection[4][9] and chronic lesions[11]. Early diagnosis is very important to prevent infection and development of the capsule (chronic lesion)[12].
Differential diagnosis[edit | edit source]
- Haematoma[4][5][7][11]
- Seroma[11]
- Soft tissue malignancy [4][5][7][11]
- Bursitis[5][7][11]
- Abscess[5]
Physiotherapy management[edit | edit source]
Although physiotherapy cannot directly treat the MLL, it can help improve functional activities and reduce pain[9]. There is no specific physiotherapy protocol, as the physiotherapy management will depend on what the patient requires e.g. range-of-motion improvement, gait re-education or strengthening. Physiotherapy management depends on the severity of the lesion, the medical/surgical management and the amount of bed rest the patient had. A case study (2022) of a patient with a thigh MLL, found that physiotherapy significantly improved joint range-of-motion, strength, cardiovascular/pulmonary function and functional independence[9]. Another study (2021) found that physiotherapy was essential to get the best functional outcomes after surgery or conservative management[13].
Medical management[edit | edit source]
Compression bandaging can be done in acute and chronic cases [2][7][9][11], with or without sclerotherapy[11][12]. Effective bandaging however not always possible in certain areas e.g. greater trochanter[2].
Existing evidence suggests that surgical treatment results is shorter healing time compared to compression bandaging alone[2]. While some MLL can resolve spontaneously[4], others have symptoms that can persist for decades and affect quality of life in untreated cases[11].
Surgical management[edit | edit source]
Surgical management is indicated if conservative management fails[11][14]; where an untreated chronic lesion has developed a fibrous capsule due to ongoing inflammation[11]; where the diagnosis is unclear[14] or where there is secondary infection[14]. Surgical treatment options include:
- Aspiration[2][4][7][9]
- Sclerotherapy alone in lesions with a volume of up to 400ml[2]. Sclerodesis with Doxycycline is most common[2][14] but other agents such as erythromycin, vancomycin and tetracycline are also used[2]. The majority of these sclerodesis agents cause fibrosis as they induce cell destruction[2].
- Percutaneous drainage with or without sclerotherapy (acute or chronic)[7][12][14]
- Drainage and debridement[9][14]. Open debridement is done when there is an open fracture[7].
- Open capsule excision in chronic and large, recurrent cases[2][11]
References[edit | edit source]
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 1.13 1.14 1.15 1.16 1.17 Diviti S, Gupta N, Hooda K, Sharma K, Lo L. Morel-Lavallee lesions-review of pathophysiology, clinical findings, imaging findings and management. Journal of clinical and diagnostic research: JCDR. 2017 Apr;11(4):TE01.
- ↑ 2.00 2.01 2.02 2.03 2.04 2.05 2.06 2.07 2.08 2.09 2.10 2.11 2.12 2.13 2.14 2.15 2.16 2.17 2.18 2.19 2.20 2.21 2.22 2.23 2.24 2.25 2.26 2.27 2.28 2.29 Singh R, Rymer B, Youssef B, Lim J. The Morel-Lavallée lesion and its management: a review of the literature. Journal of orthopaedics. 2018 Dec 1;15(4):917-21.
- ↑ 3.00 3.01 3.02 3.03 3.04 3.05 3.06 3.07 3.08 3.09 3.10 3.11 3.12 Zairi F, Wang Z, Shedid D, Boubez G, Sunna T. Lumbar Morel-Lavallée lesion: case report and review of the literature. Orthopaedics & Traumatology: Surgery & Research. 2016 Jun 1;102(4):525-7.
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 4.6 4.7 4.8 4.9 LaTulip S, Rao RR, Sielaff A, Theyyunni N, Burkhardt J. Ultrasound utility in the diagnosis of a Morel-Lavallée lesion. Case Reports in Emergency Medicine. 2017 Feb 1;2017.
- ↑ 5.00 5.01 5.02 5.03 5.04 5.05 5.06 5.07 5.08 5.09 5.10 5.11 5.12 Depaoli R, Canepari E, Bortolotto C, Ferrozzi G. Morel-Lavallée lesion of the knee in a soccer player. Journal of ultrasound. 2015 Mar;18(1):87-9.
- ↑ 6.0 6.1 6.2 6.3 6.4 6.5 6.6 6.7 6.8 Mettu R, Surath HV, Chayam HR, Surath A. Chronic Morel-Lavallée lesion: a novel minimally invasive method of treatment. Wounds. 2016 Nov 1;28(11):404-7.
- ↑ 7.00 7.01 7.02 7.03 7.04 7.05 7.06 7.07 7.08 7.09 7.10 Christian D, Leland HA, Osias W, Eberlin S, Howell L. Delayed presentation of a chronic Morel-Lavallee lesion. Journal of Radiology Case Reports. 2016 Jul;10(7):30.
- ↑ 8.00 8.01 8.02 8.03 8.04 8.05 8.06 8.07 8.08 8.09 8.10 8.11 De Coninck T, Vanhoenacker F, Verstraete K. Imaging features of Morel-Lavallée lesions. Journal of the Belgian Society of Radiology. 2017;101(Suppl 2).
- ↑ 9.00 9.01 9.02 9.03 9.04 9.05 9.06 9.07 9.08 9.09 9.10 9.11 9.12 9.13 9.14 9.15 9.16 9.17 9.18 9.19 9.20 Badjate DM, Jain D, Phansopkar P, Wadhokar OC. A Physical Therapy Rehabilitative Approach in Improving Activities of Daily Living in a Patient With Morel-Lavallée Syndrome: A Case Report. Cureus. 2022 Sep 24;14(9).
- ↑ 10.0 10.1 10.2 Weiss NA, Johnson JJ, Anderson SB. Morel-lavallee lesion initially diagnosed as quadriceps contusion: ultrasound, MRI, and importance of early intervention. Western Journal of Emergency Medicine. 2015 May;16(3):438.
- ↑ 11.00 11.01 11.02 11.03 11.04 11.05 11.06 11.07 11.08 11.09 11.10 11.11 11.12 11.13 11.14 11.15 11.16 11.17 11.18 11.19 Cruz N, Jiménez R. Morel-Lavallée lesion diagnosed 25 years after blunt trauma. International Journal of Surgery Case Reports. 2021 Apr 1;81:105733.
- ↑ 12.0 12.1 12.2 12.3 Cochran GK, Hanna KH. Morel-Lavallee lesion in the upper extremity. Hand. 2017 Jan;12(1):NP10-3.
- ↑ Agrawal U, Tiwari V. Morel Lavallee Lesion.
- ↑ 14.0 14.1 14.2 14.3 14.4 14.5 Dawre S, Lamba S, Gupta S, Gupta AK. The Morel-Lavallee lesion: a review and a proposed algorithmic approach. European Journal of Plastic Surgery. 2012 Jul;35(7):489-94.