Meningomyelocele: Difference between revisions
No edit summary |
No edit summary |
||
| Line 11: | Line 11: | ||
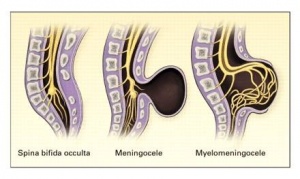
Spina Bifida Occulta: It can occur without neurologic defects. | Spina Bifida Occulta: It can occur without neurologic defects. | ||
Meningocele: A cystic swelling of the dura and arachnoid | Meningocele: A cystic swelling of the dura and arachnoid protrudes through the spina bifida defect in the vertebral arch. | ||
Meningomyelocele: when cord tissue extends into the meningocele. | Meningomyelocele: when cord tissue extends into the meningocele. | ||
| Line 24: | Line 24: | ||
== Pathophysiology == | == Pathophysiology == | ||
MMC is associated with abnormal development of the cranial neural tube, which results in several characteristic CNS anomalies. The [[Arnold Chiari Malformation|Chiari type II malformation]] is characterized by cerebellar hypoplasia and varying degrees of caudal displacement of the lower brainstem into the upper cervical canal through the foramen magnum. This deformity impedes the flow and absorption of cerebrospinal fluid (CSF) and causes hydrocephalus, which occurs in more than 90% of infants with MMC. | MMC is associated with abnormal development of the cranial neural tube, which results in several characteristic CNS anomalies. The [[Arnold Chiari Malformation|Chiari type II malformation]] is characterized by cerebellar hypoplasia and varying degrees of caudal displacement of the lower brainstem into the upper cervical canal through the foramen magnum. This deformity impedes the flow and absorption of cerebrospinal fluid (CSF) and causes hydrocephalus, which occurs in more than 90% of infants with MMC. Non-neurologic associations include spine malformations, hydronephrosis, cardiac defects, and gastrointestinal anomalies.<ref name=":1" /> | ||
== Epidemiology == | == Epidemiology == | ||
The incidence of spina-bifada worldwide 18.6 per 10,000.<ref>Hassan AE, Du YL, Lee SY, Wang A, Farmer DL. [https://www.mdpi.com/2221-3759/10/2/22 Spina Bifida: A Review of the Genetics, Pathophysiology and Emerging Cellular Therapies]. Journal of Developmental Biology. 2022 Jun 6;10(2):22.</ref> The United States of America has steadily decreased their rate by 25% to 1 per 1,500 births.<ref>Oumer M, Taye M, Aragie H, Tazebew A. [https://www.hindawi.com/journals/scientifica/2020/4273510/ Prevalence of spina bifida among newborns in Africa: a systematic review and Meta-analysis.] Scientifica. 2020 Oct 6;2020:1-2.</ref> There are variations in incidence between some racial populations. <ref name=":2">5. Shin M, Besser L, Siffel C, Kucik J, Shaw G, Lu C et al. [https://www.researchgate.net/publication/45167199_Prevalence_of_Spina_Bifida_Among_Children_and_Adolescents_in_10_Regions_in_the_United_States Prevalence of Spina Bifida Among Children and Adolescents in 10 Regions in the United States]. PEDIATRICS. 2010;126(2):274-279.</ref> African-American cases are often a third of those found for white Americans, while those for Hispanic-Americans are two to three times greater<ref name=":1" />. | |||
== Aetiology == | == Aetiology == | ||
The risk of an adult with MMC having a child with a neural tube defect is 5% <ref name=":3">6. Canfield M, Ramadhani T, Shaw G, Carmichael S, Waller D, Mosley B et al. Anencephaly and spina bifida among Hispanics: maternal, sociodemographic, and acculturation factors in the National Birth Defects Prevention Study. Birth Defects Research Part A: Clinical and Molecular Teratology. 2009;85(7):637-646.</ref>. Several risk factors have been linked to neural tube defect, including | The risk of an adult with MMC having a child with a neural tube defect is 5% <ref name=":3">6. Canfield M, Ramadhani T, Shaw G, Carmichael S, Waller D, Mosley B et al. Anencephaly and spina bifida among Hispanics: maternal, sociodemographic, and acculturation factors in the National Birth Defects Prevention Study. Birth Defects Research Part A: Clinical and Molecular Teratology. 2009;85(7):637-646.</ref>. Several risk factors have been linked to neural tube defect, including:<ref>Copp AJ, Adzick NS, Chitty LS, Fletcher JM, Holmbeck GN, Shaw GM. Spina bifida. Nat Rev Dis Primers. 2015 Apr 30;1:15007.</ref> | ||
* Chromosomal and genetic conditions: parents or siblings with neural tube defect | * Chromosomal and genetic conditions: | ||
** parents or siblings with neural tube defect | |||
*** trisomies 13 and 18 | |||
*** HARD syndrome ([[Hydrocephalus]], agyria and retinal dysplasia) etc. | |||
* Maternal environmental factors and exposure: | |||
** alcohol use | |||
** caffeine intake | |||
** smoking, air pollution | |||
** disinfectant byproducts in drinking water | |||
** exposure to organic solvents, pesticides, nitrate-related compounds, polycyclic aromatic hydrocarbons, fumonisins, EM field | |||
** maternal fever or hyperthermia ( especially in the first trimester) from febrile illness or external sources like sauna, hot tub<ref name=":1" /> | |||
* Maternal medical conditions: | |||
** Women with low RBC cell folate levels during early pregnancy have up to a 6 times greater risk of having a child with a neural tube defect | |||
** elevated glycemic index, and gestational diabetes mellitus | |||
** infections | |||
** obesity | |||
** stress | |||
** maternal diarrhoea.<ref name=":3" /> | |||
* Maternal nutritional deficiencies: | |||
** folate | |||
** methionine | |||
** zinc | |||
** vitamin C | |||
** vitamin B12 | |||
** choline. | |||
* Maternal medications: | |||
** Intrauterine exposure to antiepileptic drugs, particularly valproate and carbamazepine | |||
** drugs used to induce ovulation | |||
** various folic acid antagonists | |||
== Diagnostic Procedures == | == Diagnostic Procedures == | ||
| Line 42: | Line 66: | ||
The diagnosis in a newborn is usually obvious because of the visible bulge in the back which consists of protruding membrane-covered sac containing meninges, cerebrospinal fluid (CSF) and nerve tissue seen through a vertebral column defect. The clinical features of meningomyelocele depend on the: | The diagnosis in a newborn is usually obvious because of the visible bulge in the back which consists of protruding membrane-covered sac containing meninges, cerebrospinal fluid (CSF) and nerve tissue seen through a vertebral column defect. The clinical features of meningomyelocele depend on the: | ||
* | * level of involvement | ||
* | * presence of hydrocephalus | ||
* | * associated brain abnormalities | ||
In addition, the measurement of maternal serum α-fetoprotein (MSAFP) levels is a common screening test. If the level is elevated, indicating that any portion of the fetus is not covered by skin, this screening test is then followed by detailed ultrasonography. Ultrasound scans will diagnose 92% of neural tube defects. Mothers with elevated MSAFP levels and a normal-appearing ultrasound scan may be evaluated by amniocentesis for the presence of elevated acetylcholinesterase levels in the amniotic fluid.<ref name=":1" /><br> | In addition, the measurement of maternal serum α-fetoprotein (MSAFP) levels is a common screening test. If the level is elevated, indicating that any portion of the fetus is not covered by skin, this screening test is then followed by detailed ultrasonography. Ultrasound scans will diagnose 92% of neural tube defects. Mothers with elevated MSAFP levels and a normal-appearing ultrasound scan may be evaluated by amniocentesis for the presence of elevated acetylcholinesterase levels in the amniotic fluid.<ref name=":1" /><br> | ||
== Management / Interventions == | |||
== Management / Interventions | |||
Generally, surgery follows within the first few days of life to close the spinal cord defect.<ref name=":1" /> It is also important to prevent infection and additional trauma to the exposed tissues. Additional surgeries may be required to manage other problems in the feet, hips, or spine. Individuals with hydrocephalus will also require subsequent surgeries due to the shunt needing to be replaced. Due to the bowel and bladder problems that are often caused by the neural tube defect, catheterization may be necessary. | Generally, surgery follows within the first few days of life to close the spinal cord defect.<ref name=":1" /> It is also important to prevent infection and additional trauma to the exposed tissues. Additional surgeries may be required to manage other problems in the feet, hips, or spine. Individuals with hydrocephalus will also require subsequent surgeries due to the shunt needing to be replaced. Due to the bowel and bladder problems that are often caused by the neural tube defect, catheterization may be necessary. | ||
The Management of Myelomeningocele Study (MOMS).<ref>7. McLone D, Knepper P. The Cause of Chiari II Malformation: A Unified Theory. Pediatric Neurosurgery. 1989;15(1):1-12.</ref>The MOMS trial is an NIH-sponsored multicenter clinical trial that began in 2002 to evaluate what was the best treatment for myelomeningocele — fetal surgery or surgical repair after birth. | The Management of Myelomeningocele Study (MOMS).<ref>7. McLone D, Knepper P. The Cause of Chiari II Malformation: A Unified Theory. Pediatric Neurosurgery. 1989;15(1):1-12.</ref>The MOMS trial is an NIH-sponsored multicenter clinical trial that began in 2002 to evaluate what was the best treatment for myelomeningocele — fetal surgery or surgical repair after birth. The clinical trial results showed prenatal surgery significantly reduced the need to divert, or shunt, fluid away from the brain; improved mental development and motor function; and increased the likelihood that a child will walk unassisted. The MOMS trial has proved that some of the factors causing problems like Chiari II malformation and hydrocephalus are in fact those that develop during the second half of pregnancy. Closing the fetus’s back early may allow some nerve function to be restored in pregnancy, and actually, reverse the development of this serious condition. | ||
The clinical trial results showed prenatal surgery significantly reduced the need to divert, or shunt, fluid away from the brain; improved mental development and motor function; and increased the likelihood that a child will walk unassisted. The MOMS trial has proved that some of the factors causing problems like Chiari II malformation and hydrocephalus are in fact those that develop during the second half of pregnancy. Closing the fetus’s back early may allow some nerve function to be restored in pregnancy, and actually, reverse the development of this serious condition. | |||
== Physiotherapy Management == | == Physiotherapy Management == | ||
A multidisciplinary approach towards managing patients with MMC is essential for successful outcomes. The patient should be assessed as soon after birth as possible. At different stages, the focus of physiotherapy will change with the changing needs of the patient. Regular review is essential to meet up with patient needs. Parents and caregivers should be involved in patient care. | A multidisciplinary approach towards managing patients with MMC is essential for successful outcomes. The patient should be assessed as soon after birth as possible. At different stages, the focus of physiotherapy will change with the changing needs of the patient. Regular review is essential to meet up with patient needs. Parents and caregivers should be involved in patient care. | ||
* CLINICAL PRESENTATION - | * CLINICAL PRESENTATION - <ref name=":1" />Possible signs include: | ||
** Flaccid or spastic paralysis of the lower limbs | |||
** Urinary and or faecal incontinence | |||
** Hydrocephalus | |||
** Poor trunk control | |||
** Musculoskeletal complications | |||
** Scoliosis | |||
** Hip dysplasia | |||
** Hip dislocation | |||
** Hip/knee contracture | |||
** Clubfoot | |||
** Muscle Atrophy | |||
* PHYSICAL ASSESSMENT- The following may be observed during the physical assessment. | * PHYSICAL ASSESSMENT- The following may be observed during the physical assessment. | ||
| Line 85: | Line 114: | ||
* MEANS OF TREATMENT | * MEANS OF TREATMENT | ||
** Serial casting | ** Serial casting | ||
** Passive mobilization, graded exercises and stretches. | ** Passive mobilization, graded exercises and stretches. | ||
** Tactile stimulation | ** Tactile stimulation | ||
| Line 91: | Line 120: | ||
** Positioning | ** Positioning | ||
** Orthosis & Assistive devices | ** Orthosis & Assistive devices | ||
** Parent education: Parents should be educated about the child’s condition, progress, and prognosis and involved in treatment planning and home programmes.<ref>8. McDonnell G, McCann J. Issues of medical management in adults with spina bifida. Child's Nervous System. 2000;16(4):222-227.</ref> | ** Parent education: Parents should be educated about the child’s condition, progress, and prognosis and involved in treatment planning and home programmes.<ref>8. McDonnell G, McCann J. Issues of medical management in adults with spina bifida. Child's Nervous System. 2000;16(4):222-227.</ref> <br> | ||
== Complications == | == Complications == | ||
| Line 97: | Line 126: | ||
=== Common Complications of MMC Include the Following.<ref name=":1" /> === | === Common Complications of MMC Include the Following.<ref name=":1" /> === | ||
* Reproductive organs impairment | * Reproductive organs impairment | ||
* Only 5.0% to 7.5% of the MMC population have a normal urologic function | |||
* Only 5.0% to 7.5% of the MMC population have a normal urologic function | * Neurogenic Bowel: Traditional bowel continence is present in approximately 10% of children with MMC | ||
* Neurogenic Bowel: Traditional bowel continence is present in approximately 10% of children with MMC | * Musculoskeletal complications | ||
* Musculoskeletal complications | |||
* Psychosocial issues: Vulnerable child syndrome. | * Psychosocial issues: Vulnerable child syndrome. | ||
* Pressure sores | * Pressure sores | ||
| Line 107: | Line 135: | ||
=== Neurosurgical Complications === | === Neurosurgical Complications === | ||
* Wound infection rates range from 7% to 12% <ref name=":1" /> | * Wound infection rates range from 7% to 12% <ref name=":1" /> | ||
* Hydrocephalus | * Hydrocephalus | ||
* Ventriculitis | * Visual impairment | ||
* Ventriculitis | |||
* Low subsequent IQ | |||
* Shunt failure | * Shunt failure | ||
** 5% - 32% of infants with MMC will present with signs of Chiari compression, making it the most common cause of death in patients with MMC | ** 5% - 32% of infants with MMC will present with signs of Chiari compression, making it the most common cause of death in patients with MMC | ||
* Chiari compression can occur at any time, presentation in the first year of life is associated with up to 50% mortality.<ref name=":4">Campbell, SK, Linden, DW, Palisano RJ (2000). Physical Therapy for Children (2nd Edition). Philadelphia, PA: W.B. Saunders.</ref> | * Chiari compression can occur at any time, presentation in the first year of life is associated with up to 50% mortality.<ref name=":4">Campbell, SK, Linden, DW, Palisano RJ (2000). Physical Therapy for Children (2nd Edition). Philadelphia, PA: W.B. Saunders.</ref> | ||
* Chronic headaches are the most frequently reported symptom.<ref name=":4" /> | * Chronic headaches are the most frequently reported symptom.<ref name=":4" /> | ||
* Obesity - Obesity is prevalent in children with MMC. The higher the level of the lesion along the spine the higher | * Obesity - Obesity is prevalent in children with MMC. The higher the level of the lesion along the spine the higher the percentage of body fat.<ref name=":1" />In children with L1–L3 lesions, the effect of increasing obesity is a critical factor in the loss of ambulation.<ref name=":1" />Typically, children with MMC reach their peak ambulatory abilities around the age of 10 years. They then experience a slow decline in function over the next 10 years. The children who ambulate more have a lower percentage of body fat. <ref name=":1" /><br> | ||
== Conclusion == | == Conclusion == | ||
About 90% of babies born with Spina Bifida now live to be adults, about 80% have normal intelligence and about 75% play sports and do other fun activities | About 90% of babies born with Spina Bifida now live to be adults, about 80% have normal intelligence and about 75% play sports and do other fun activities. <ref name=":1" /> | ||
A cross-sectional study (August 2020) by a multidisciplinary team describing health issues and living conditions in a cohort of adults living with Spina bifida suggest the presence of a higher prevalence of urinary and faecal incontinence, pain, and overweight in adults with Spina Bifida. Persons with the condition greater than 46 years had less complicated medical conditions, better physical and cognitive functions, and higher education, independent living, and participation in society, whereas individuals < 46 years had more secondary conditions such as hydrocephalus, Chiari II malformation, tethered cord symptoms, and latex allergy<ref>Bendt M, Gabrielsson H, Riedel D, Hagman G, Hultling C, Franzén E, Eriksson M, Seiger Å. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7428499/ Adults with spina bifida: A cross‐sectional study of health issues and living conditions.] Brain and Behavior. 2020 Aug;10(8):e01736.</ref>. | A cross-sectional study (August 2020) by a multidisciplinary team describing health issues and living conditions in a cohort of adults living with Spina bifida suggest the presence of a higher prevalence of urinary and faecal incontinence, pain, and overweight in adults with Spina Bifida. Persons with the condition greater than 46 years had less complicated medical conditions, better physical and cognitive functions, and higher education, independent living, and participation in society, whereas individuals < 46 years had more secondary conditions such as hydrocephalus, Chiari II malformation, tethered cord symptoms, and latex allergy<ref>Bendt M, Gabrielsson H, Riedel D, Hagman G, Hultling C, Franzén E, Eriksson M, Seiger Å. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7428499/ Adults with spina bifida: A cross‐sectional study of health issues and living conditions.] Brain and Behavior. 2020 Aug;10(8):e01736.</ref>. | ||
Revision as of 16:36, 3 April 2023
Introduction[edit | edit source]
Spina Bifida is a variable defect in which the vertebral arch of the spinal column is either incompletely formed or absent. The term Bifida is from the Latin word Bifidus, or "left in 2 parts." It is classified as a defect of the neural tube (i.e. the embryonic structure that develops into the spinal cord and brain). Neural tube defects have a range of presentations, from stillbirth to incidental radiographic findings of spina bifida occulta. The term myelodysplasia has been used as a synonym for Spina bifida.[1][2]Lesions most commonly occur in the lumbar and sacral regions but can be found anywhere along the entire length of the spine.[1] It is a treatable spinal cord malformation that occurs in varying degrees of severity.[2]
Types of Spina Bifida[edit | edit source]
Spina Bifida Occulta: It can occur without neurologic defects.
Meningocele: A cystic swelling of the dura and arachnoid protrudes through the spina bifida defect in the vertebral arch.
Meningomyelocele: when cord tissue extends into the meningocele.
Myeloschisis: If the spinal cord is exposed on the surface of the back, the condition is called myeloschisis .[3]
Embryology[edit | edit source]
Neural tube defects occur between the 17th and 30th days of gestation. This defect then disrupts all of the overlying tissues, preventing the vertebral arch from closing.[4]If the posterior vertebral arch and overlying tissues do not form normally, the normal spinal cord and meninges may then herniate out through the defect and cause a meningomyelocele (MMC). If the vertebral arch fails to grow and fuse normally and the spinal cord and meninges are not disturbed spina bifida occulta results.[2]
Pathophysiology[edit | edit source]
MMC is associated with abnormal development of the cranial neural tube, which results in several characteristic CNS anomalies. The Chiari type II malformation is characterized by cerebellar hypoplasia and varying degrees of caudal displacement of the lower brainstem into the upper cervical canal through the foramen magnum. This deformity impedes the flow and absorption of cerebrospinal fluid (CSF) and causes hydrocephalus, which occurs in more than 90% of infants with MMC. Non-neurologic associations include spine malformations, hydronephrosis, cardiac defects, and gastrointestinal anomalies.[2]
Epidemiology[edit | edit source]
The incidence of spina-bifada worldwide 18.6 per 10,000.[5] The United States of America has steadily decreased their rate by 25% to 1 per 1,500 births.[6] There are variations in incidence between some racial populations. [7] African-American cases are often a third of those found for white Americans, while those for Hispanic-Americans are two to three times greater[2].
Aetiology[edit | edit source]
The risk of an adult with MMC having a child with a neural tube defect is 5% [8]. Several risk factors have been linked to neural tube defect, including:[9]
- Chromosomal and genetic conditions:
- parents or siblings with neural tube defect
- trisomies 13 and 18
- HARD syndrome (Hydrocephalus, agyria and retinal dysplasia) etc.
- parents or siblings with neural tube defect
- Maternal environmental factors and exposure:
- alcohol use
- caffeine intake
- smoking, air pollution
- disinfectant byproducts in drinking water
- exposure to organic solvents, pesticides, nitrate-related compounds, polycyclic aromatic hydrocarbons, fumonisins, EM field
- maternal fever or hyperthermia ( especially in the first trimester) from febrile illness or external sources like sauna, hot tub[2]
- Maternal medical conditions:
- Women with low RBC cell folate levels during early pregnancy have up to a 6 times greater risk of having a child with a neural tube defect
- elevated glycemic index, and gestational diabetes mellitus
- infections
- obesity
- stress
- maternal diarrhoea.[8]
- Maternal nutritional deficiencies:
- folate
- methionine
- zinc
- vitamin C
- vitamin B12
- choline.
- Maternal medications:
- Intrauterine exposure to antiepileptic drugs, particularly valproate and carbamazepine
- drugs used to induce ovulation
- various folic acid antagonists
Diagnostic Procedures[edit | edit source]
The diagnosis in a newborn is usually obvious because of the visible bulge in the back which consists of protruding membrane-covered sac containing meninges, cerebrospinal fluid (CSF) and nerve tissue seen through a vertebral column defect. The clinical features of meningomyelocele depend on the:
- level of involvement
- presence of hydrocephalus
- associated brain abnormalities
In addition, the measurement of maternal serum α-fetoprotein (MSAFP) levels is a common screening test. If the level is elevated, indicating that any portion of the fetus is not covered by skin, this screening test is then followed by detailed ultrasonography. Ultrasound scans will diagnose 92% of neural tube defects. Mothers with elevated MSAFP levels and a normal-appearing ultrasound scan may be evaluated by amniocentesis for the presence of elevated acetylcholinesterase levels in the amniotic fluid.[2]
Management / Interventions[edit | edit source]
Generally, surgery follows within the first few days of life to close the spinal cord defect.[2] It is also important to prevent infection and additional trauma to the exposed tissues. Additional surgeries may be required to manage other problems in the feet, hips, or spine. Individuals with hydrocephalus will also require subsequent surgeries due to the shunt needing to be replaced. Due to the bowel and bladder problems that are often caused by the neural tube defect, catheterization may be necessary.
The Management of Myelomeningocele Study (MOMS).[10]The MOMS trial is an NIH-sponsored multicenter clinical trial that began in 2002 to evaluate what was the best treatment for myelomeningocele — fetal surgery or surgical repair after birth. The clinical trial results showed prenatal surgery significantly reduced the need to divert, or shunt, fluid away from the brain; improved mental development and motor function; and increased the likelihood that a child will walk unassisted. The MOMS trial has proved that some of the factors causing problems like Chiari II malformation and hydrocephalus are in fact those that develop during the second half of pregnancy. Closing the fetus’s back early may allow some nerve function to be restored in pregnancy, and actually, reverse the development of this serious condition.
Physiotherapy Management[edit | edit source]
A multidisciplinary approach towards managing patients with MMC is essential for successful outcomes. The patient should be assessed as soon after birth as possible. At different stages, the focus of physiotherapy will change with the changing needs of the patient. Regular review is essential to meet up with patient needs. Parents and caregivers should be involved in patient care.
- CLINICAL PRESENTATION - [2]Possible signs include:
- Flaccid or spastic paralysis of the lower limbs
- Urinary and or faecal incontinence
- Hydrocephalus
- Poor trunk control
- Musculoskeletal complications
- Scoliosis
- Hip dysplasia
- Hip dislocation
- Hip/knee contracture
- Clubfoot
- Muscle Atrophy
- PHYSICAL ASSESSMENT- The following may be observed during the physical assessment.
- Open wound
- Deformities
- Skin abnormalities
- Sensation
- Muscle tone
- Muscle Strength
- Range of Motion
- Contractures
- Dislocation
- Developmental Milestones
- PLAN OF CARE
- Prevent/correct deformity
- Maintain/improve physiological properties of joints and muscles
- Monitor normal motor development
- Educate parent(s), caregivers
- Encourage and maximise independent mobility
- Encourage participation in regular physical activity.
- MEANS OF TREATMENT
- Serial casting
- Passive mobilization, graded exercises and stretches.
- Tactile stimulation
- Balance & Trunk control exercises
- Positioning
- Orthosis & Assistive devices
- Parent education: Parents should be educated about the child’s condition, progress, and prognosis and involved in treatment planning and home programmes.[11]
Complications[edit | edit source]
Common Complications of MMC Include the Following.[2][edit | edit source]
- Reproductive organs impairment
- Only 5.0% to 7.5% of the MMC population have a normal urologic function
- Neurogenic Bowel: Traditional bowel continence is present in approximately 10% of children with MMC
- Musculoskeletal complications
- Psychosocial issues: Vulnerable child syndrome.
- Pressure sores
- Learning disabilities
Neurosurgical Complications[edit | edit source]
- Wound infection rates range from 7% to 12% [2]
- Hydrocephalus
- Visual impairment
- Ventriculitis
- Low subsequent IQ
- Shunt failure
- 5% - 32% of infants with MMC will present with signs of Chiari compression, making it the most common cause of death in patients with MMC
- Chiari compression can occur at any time, presentation in the first year of life is associated with up to 50% mortality.[12]
- Chronic headaches are the most frequently reported symptom.[12]
- Obesity - Obesity is prevalent in children with MMC. The higher the level of the lesion along the spine the higher the percentage of body fat.[2]In children with L1–L3 lesions, the effect of increasing obesity is a critical factor in the loss of ambulation.[2]Typically, children with MMC reach their peak ambulatory abilities around the age of 10 years. They then experience a slow decline in function over the next 10 years. The children who ambulate more have a lower percentage of body fat. [2]
Conclusion[edit | edit source]
About 90% of babies born with Spina Bifida now live to be adults, about 80% have normal intelligence and about 75% play sports and do other fun activities. [2]
A cross-sectional study (August 2020) by a multidisciplinary team describing health issues and living conditions in a cohort of adults living with Spina bifida suggest the presence of a higher prevalence of urinary and faecal incontinence, pain, and overweight in adults with Spina Bifida. Persons with the condition greater than 46 years had less complicated medical conditions, better physical and cognitive functions, and higher education, independent living, and participation in society, whereas individuals < 46 years had more secondary conditions such as hydrocephalus, Chiari II malformation, tethered cord symptoms, and latex allergy[13].
References[edit | edit source]
- ↑ 1.0 1.1 Lundy-Ekman L (2007). Neuroscience: Fundamentals for Rehabilitation. 3rd edition. St. Louis: Saunders, 2007
- ↑ 2.00 2.01 2.02 2.03 2.04 2.05 2.06 2.07 2.08 2.09 2.10 2.11 2.12 2.13 2.14 Spina Bifida: Background, Pathophysiology, Etiology [Internet]. Emedicine.medscape.com. 2019 [cited 2 March 2019]. Available from: http://emedicine.medscape.com/article/311113-overview
- ↑ 4. Burke R, Liptak G. Providing a Primary Care Medical Home for Children and Youth With Spina Bifida. PEDIATRICS. 2011;128(6):e1645-e1657.
- ↑ Fletcher JM, Copeland K, Frederick JA (2005). Spinal lesion level in spina bifida: a source of neural and cognitive heterogeneity. Journal of Neurosurgery. 102(3 Suppl):268-79
- ↑ Hassan AE, Du YL, Lee SY, Wang A, Farmer DL. Spina Bifida: A Review of the Genetics, Pathophysiology and Emerging Cellular Therapies. Journal of Developmental Biology. 2022 Jun 6;10(2):22.
- ↑ Oumer M, Taye M, Aragie H, Tazebew A. Prevalence of spina bifida among newborns in Africa: a systematic review and Meta-analysis. Scientifica. 2020 Oct 6;2020:1-2.
- ↑ 5. Shin M, Besser L, Siffel C, Kucik J, Shaw G, Lu C et al. Prevalence of Spina Bifida Among Children and Adolescents in 10 Regions in the United States. PEDIATRICS. 2010;126(2):274-279.
- ↑ 8.0 8.1 6. Canfield M, Ramadhani T, Shaw G, Carmichael S, Waller D, Mosley B et al. Anencephaly and spina bifida among Hispanics: maternal, sociodemographic, and acculturation factors in the National Birth Defects Prevention Study. Birth Defects Research Part A: Clinical and Molecular Teratology. 2009;85(7):637-646.
- ↑ Copp AJ, Adzick NS, Chitty LS, Fletcher JM, Holmbeck GN, Shaw GM. Spina bifida. Nat Rev Dis Primers. 2015 Apr 30;1:15007.
- ↑ 7. McLone D, Knepper P. The Cause of Chiari II Malformation: A Unified Theory. Pediatric Neurosurgery. 1989;15(1):1-12.
- ↑ 8. McDonnell G, McCann J. Issues of medical management in adults with spina bifida. Child's Nervous System. 2000;16(4):222-227.
- ↑ 12.0 12.1 Campbell, SK, Linden, DW, Palisano RJ (2000). Physical Therapy for Children (2nd Edition). Philadelphia, PA: W.B. Saunders.
- ↑ Bendt M, Gabrielsson H, Riedel D, Hagman G, Hultling C, Franzén E, Eriksson M, Seiger Å. Adults with spina bifida: A cross‐sectional study of health issues and living conditions. Brain and Behavior. 2020 Aug;10(8):e01736.