Medical Imaging: Difference between revisions
No edit summary |
No edit summary |
||
| (17 intermediate revisions by 3 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> '''Original Editor '''- [[User:Rachael Lowe|Rachael Lowe]] '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> | <div class="editorbox"> '''Original Editor '''- [[User:Rachael Lowe|Rachael Lowe]] '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> | ||
== Overview == | == Overview == | ||
[[File: | [[File:Cardiac MRI flow.gif|alt=|thumb| Cardiac MRI flow ]] | ||
<p align="justify"> | <p align="justify"> | ||
Medical | Medical imaging refers to all diagnostic and therapeutic investigations/interventions conducted in a typical radiology department. It encompasses different imaging modalities and processes to obtain images of the human body for diagnostic, treatment and follow up purposes. | ||
</p> | </p> | ||
<p align="justify"> | <p align="justify"> | ||
Imaging investigations have improved significantly over the years and play in important role in diagnostics. It also plays an important role in initiatives to improve public health through screening for certain conditions<ref name=":2">WHO [https://www.who.int/diagnostic_imaging/en/ Diagnostic Imaging] Available from: https://www.who.int/diagnostic_imaging/en/<nowiki/>(accessed 7.4.2021)</ref>. Imaging does however need to be utilised with caution and sound clinical reasoning in order to avoid the potential harms of medical imaging, such as radiation and iatrogenic pain. | |||
</p> | </p> | ||
== | == Types of Imaging == | ||
* [[X-Rays|'''X-rays''']] (including plain radiographs, [[DEXA Scan|DEXA]] scans and fluoroscopy): Allows upright and dynamic imaging; assesses bony structures and can help to detect pulmonary pathology, abnormal growths, factures, oedema and deformities. | |||
[[ | * [[MRI Scans|'''Magnetic resonance imaging''']] (MRI): Advanced imaging of soft tissue structure | ||
* [[Ultrasound Scans|'''Ultrasound''']] (US) | |||
* [[CT Scans|'''Computed tomography''']] (CT): More accurate assessment of bony structures | |||
* '''[[Nuclear Medicine|Nuclear medicine]]:''' is the practice of utilising microscopic amounts of radioactive substances to diagnose, monitor and treat disease.<ref>Radiopedia Nuclear medicine Available:https://radiopaedia.org/articles/nuclear-medicine (accessed 8.10.20220</ref> | |||
* '''PET''' (positron emission tomography) scan: an imaging test that involves the intravenous injection of a positron-emitting radiopharmaceutical, waiting to allow for systemic distribution, and then scanning for detection and quantification of patterns of radiopharmaceutical accumulation in the body. Used to diagnose a variety of diseases (for example tumours, heart disease, brain disorders). Provides a picture of the body working.<ref>Radiopedia PET Available: https://radiopaedia.org/articles/positron-emission-tomography<nowiki/>(accessed 8.10.2022)</ref> | |||
* '''SPECT''' (Single photon emission computed tomography) similar to PET, is a nuclear medicine imaging techniques which provide metabolic and functional information unlike CT and MRI.<ref>Radiopedia SPECT vs PET Available:https://radiopaedia.org/articles/spect-vs-pet (accessed 8.10.2022)</ref> | |||
=== | === Hybrid Imaging === | ||
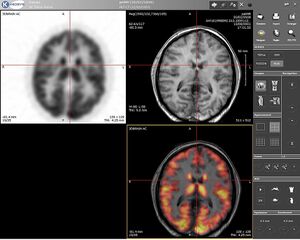
< | [[File:PET-MRI.jpeg|thumb|300x300px|PET-MRI]] | ||
Hybrid Imaging is the fusion of two (or more) imaging modalities to form a new technique<ref>Radiopedia [https://radiopaedia.org/articles/modality?lang=us Modalities] Available from:https://radiopaedia.org/articles/modality?lang=us (accessed 7.4.2021)</ref>. By combining the innate advantages of the fused imaging technologies synergistically, usually a new and more powerful modality comes into being. Existing hybrid imaging modalities include: PET-CT, SPECT-CT, MRI-PET, MRI-SPECT | |||
The general benefits of hybrid imaging include: Increased diagnostic accuracy, precise monitoring of interventional procedure and reduced radiation exposure, e.g. dynamic US after obtaining CT map. | |||
== | === Photoacoustic Imaging (PA) === | ||
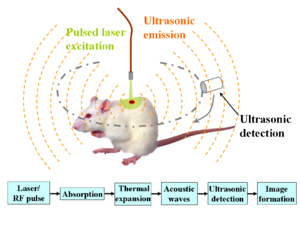
[[File:PA.png|thumb|Schematic illustration of PA imaging]] | |||
<p align="justify"> | <p align="justify"> | ||
Also known as | Also known as Optoacoustic Imaging, is an upcoming biomedical imaging modality availing the benefits of optical resolution and acoustic depth of penetration. Optoacoustic imaging has demonstrated promising potential in a wide range of preclinical and clinical applications.<ref name=":1">Amalina Binte Ebrahim Attia, Ghayathri Balasundaram, Mohesh Moothanchery, U.S. Dinish, Renzhe Bi, Vasilis Ntziachristos, Malini Olivo, A review of clinical photoacoustic imaging: Current and future trends, | ||
Photoacoustics, Volume 16, 2019, 100144, ISSN 2213-5979, obtained from https://www.sciencedirect.com/science/article/pii/S2213597919300679 doi: 10.1016/j.pacs.2019.100144 | Photoacoustics, Volume 16, 2019, 100144, ISSN 2213-5979, obtained from https://www.sciencedirect.com/science/article/pii/S2213597919300679 doi: 10.1016/j.pacs.2019.100144 | ||
</ref> | </ref> Clinical applications of optoacoustic imaging include: Musculoskeletal Imaging; Gastrointestinal Imaging; Breast imaging; Dermatologic Imaging eg Skin cancer; Vascular Imaging; Carotid Vessel Imaging.<ref name=":1" /> | ||
</p><p align="justify"> | |||
Studies have showed the potential use of optoacoustic imaging in the assessment, diagnosis and monitoring of treatment in patients with inflammatory arthritis<ref>Jo J, Tian C, Xu G, et al. Photoacoustic tomography for human musculoskeletal imaging and inflammatory arthritis detection. ''Photoacoustics''. 2018;12:82–89. Published 2018 Jul 27 obtained from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6306364/ doi:10.1016/j.pacs.2018.07.004 | |||
</ref> as well as limb and muscle ischemia.<ref>Chen L, Ma H, Liu H, et al. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5446508/ Quantitative photoacoustic imaging for early detection of muscle ischemia injury]. ''Am J Transl Res''. 2017;9(5):2255–2265. Published 2017 May 15 obtained from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5446508/</ref> | |||
</p> | </p> | ||
== Necessity of Medical Imaging == | |||
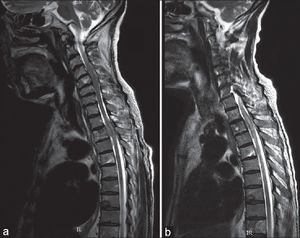
[[File:CT spinal cord.jpg|alt=|thumb|CT spinal cord]]Medical imaging is crucial in a variety of medical setting and at all major levels of health care. In public health and preventive medicine as well as in both curative and palliative care, effective decisions depend on correct diagnoses. Though clinical reasoning may be sufficient prior to treatment of many conditions, the use of diagnostic imaging services is paramount in confirming, correctly assessing and documenting courses of many diseases as well as in assessing responses to treatment. | |||
== Caution with Imaging == | |||
Imaging is a useful resource for many conditions and is an invaluable tool for clinicians/physiotherapists when used appropriately. It is important to know when imaging is appropriate, as unnecessary imaging will squander financial resources and increase the potential for premature surgery/ iatrogenic effects. | |||
Early or unnecessary referral for imaging may be influenced by patient expectations and clinician concerns, or may be used as way to reassure patients. These factors need to be managed with good communication and evidence based guidelines.<ref name=":0" /> | |||
Also see: [[Diagnostic Imaging: Best Practice|Diagnostic Imaging Best Practice]] | |||
=== Iatrogenic Effects === | |||
Abnormal radiologic findings of the musculoskeletal system can be very common. Not all abnormalities are relevant to a patient's complaint and over-emphasising radiologic findings can have harmful effects. | |||
* '''Routine MRI''' reports produce worse functional outcomes compared to a 'clinical report' (which includes reassurance of incidental findings) in patients with low back pain.<ref>Rajasekaran S, Dilip Chand Raja S, Pushpa BT, Ananda KB, Ajoy Prasad S, Rishi MK. The catastrophization effects of an MRI report on the patient and surgeon and the benefits of ‘clinical reporting’: results from an RCT and blinded trials. European Spine Journal. 2021 Jul;30:2069-81.</ref> | |||
* '''Early-MRI''' in acute low back pain results in longer length of disability, higher medical cost and worse outcomes regardless of radiculopathy (even after controlling for severity and demographics)<ref name=":0">Webster BS, Bauer AZ, Choi Y, Cifuentes M, Pransky GS. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4235393/ Iatrogenic consequences of early magnetic resonance imaging in acute, work-related, disabling low back pain.] Spine. 2013 Oct 15;38(22):1939-46.</ref> | |||
It is therefore very important to carefully consider whether imaging is indicated, and to always view the results in the context of an in depth history and physical examination. This will help to discern whether findings correlate with the patient's complaint, or are in fact incidental and negligible. | |||
=== Radiation === | |||
Even though most imaging techniques use low doses of radiation, large, repeated doses have a cumulative effect and can be harmful to human health (including cancer and tissue damage). '''"Image gently"''' and '''"Image wisely"''' are initiatives that promote practices that reduce radiation exposure by eliminating unnecessary procedures (see resource section).<ref>Ford B, Dore M, Moullet P. [https://www.aafp.org/pubs/afp/issues/2021/0101/p42.pdf Diagnostic imaging: appropriate and safe use.] American Family Physician. 2021 Jan 1;103(1):42-50.</ref>Modern techniques have also resulted in reductions in radiation exposure during imaging. | |||
Factors that should be considered include a patient's age and lifetime exposure to radiation, as well as whether the benefit of the diagnostic test outweighs the risk. CT-scans have higher radiation risk than x-rays, whereas no ionising radiation is produced during MRI or ultrasound scans.<ref name=":3">Mafraji, M.A. Risk of Radiation in Medical Imaging [Internet]. Merck Manuals. 2023 [updated 2023 November; cited 2024 March]. Available from: https://www.msdmanuals.com/home/special-subjects/common-imaging-tests/computed-tomography-ct </ref> | |||
Radiation risk is of particular concern in the following scenarios:<ref name=":3" />: | |||
* During infancy and early childhood | |||
* During pregnancy (especially early) | |||
=== Asymptomatic Findings === | |||
<p align="justify">Although advanced imaging is generally very sensitive, it can be very non-specific. Various studies have found that imaging findings and symptoms often do not correlate. Consider the table below - these findings provide evidence that what we regard as pathology may not be that significant. Also see the pages on imaging of specific body regions for more detail:</p> | |||
* [[Diagnostic Imaging of the Foot and Ankle for Physical Therapists|Foot and Ankle]] | |||
* [[Diagnostic Imaging of the Knee for Physical Therapists|Knee]] | |||
* [[Diagnostic Imaging of the Hip for Physical Therapists|Hip]] | |||
* [[Common Diagnostic Imaging of the Lumbar Spine|Lumbar spine]] | |||
* [[Diagnostic Imaging of the Shoulder|Shoulder]] | |||
{| class="wikitable" | |||
|+Pathologies in asymptomatic subjects | |||
!'''Pathology''' | |||
!'''Prevalence among asymptomatic population''' | |||
|- | |||
|Lumbar disc herniation and/or spinal stenosis | |||
|20- 75% | |||
|- | |||
|Cervical disc bulging | |||
|75 - 90%<ref>Nakashima H, Yukawa Y, Suda K, Yamagata M, Ueta T, Kato F. Abnormal findings on magnetic resonance images of the cervical spines in 1211 asymptomatic subjects. Spine. 2015 Mar 15;40(6):392-8.</ref> | |||
|- | |||
|Cervical spinal cord compression | |||
|7 - 35% <ref>Smith SS, Stewart ME, Davies BM, Kotter MR. The prevalence of asymptomatic and symptomatic spinal cord compression on magnetic resonance imaging: a systematic review and meta-analysis. Global spine journal. 2021 May;11(4):597-607.</ref> | |||
|- | |||
|Rotator cuff tendinopathy | |||
|25 - 89% <ref name=":4">Girish G, Lobo LG, Jacobson JA, Morag Y, Miller B, Jamadar DA. Ultrasound of the shoulder: asymptomatic findings in men. American Journal of Roentgenology. 2011 Oct;197(4):W713-9.</ref> | |||
|- | |||
|Mild glenohumeral or acromioclavicular OA 12 | |||
|50 - 70%<ref name=":4" /> | |||
|- | |||
|Hip labrum tear 13/14 | |||
|54% <ref>Heerey, J.J., Kemp, J.L., Mosler, A.B., Jones, D.M., Pizzari, T., Souza, R.B. and Crossley, K.M., 2018. What is the prevalence of imaging-defined intra-articular hip pathologies in people with and without pain? A systematic review and meta-analysis. ''British Journal of Sports Medicine'', ''52''(9), pp.581-593.</ref> | |||
|- | |||
|Knee Meniscal abnormalities and OA 19 | |||
|60% <ref>Englund M, Guermazi A, Gale D, Hunter DJ, Aliabadi P, Clancy M, Felson DT. Incidental meniscal findings on knee MRI in middle-aged and elderly persons. New England Journal of Medicine. 2008 Sep 11;359(11):1108-15.</ref> | |||
|} | |||
== Health Care Team == | |||
Imaging for medical purposes involves a team which includes the service of radiologists, radiographers (x-ray technologists), sonographers (ultrasound technologists), medical physicists, nurses, biomedical engineers, and other support staff working together. Appropriate use of medical imaging requires a multidisciplinary approach.<ref name=":2" /> | |||
== Conclusion == | |||
Medical imaging is a crucial component of healthcare and provide a valuable tool for diagnosis, screening and treatment. It is however important to follow [[Diagnostic Imaging: Best Practice|best practice guidelines]] with a particular focus on avoiding unnecessary imaging and ensuring appropriate, evidence-based interpretation of results. '''We treat whole, complex persons - not images and scans.''' | |||
==Diagnostic Imaging for Body Regions== | ==Diagnostic Imaging for Body Regions== | ||
Latest revision as of 16:41, 21 March 2024
Overview[edit | edit source]
Medical imaging refers to all diagnostic and therapeutic investigations/interventions conducted in a typical radiology department. It encompasses different imaging modalities and processes to obtain images of the human body for diagnostic, treatment and follow up purposes.
Imaging investigations have improved significantly over the years and play in important role in diagnostics. It also plays an important role in initiatives to improve public health through screening for certain conditions[1]. Imaging does however need to be utilised with caution and sound clinical reasoning in order to avoid the potential harms of medical imaging, such as radiation and iatrogenic pain.
Types of Imaging[edit | edit source]
- X-rays (including plain radiographs, DEXA scans and fluoroscopy): Allows upright and dynamic imaging; assesses bony structures and can help to detect pulmonary pathology, abnormal growths, factures, oedema and deformities.
- Magnetic resonance imaging (MRI): Advanced imaging of soft tissue structure
- Ultrasound (US)
- Computed tomography (CT): More accurate assessment of bony structures
- Nuclear medicine: is the practice of utilising microscopic amounts of radioactive substances to diagnose, monitor and treat disease.[2]
- PET (positron emission tomography) scan: an imaging test that involves the intravenous injection of a positron-emitting radiopharmaceutical, waiting to allow for systemic distribution, and then scanning for detection and quantification of patterns of radiopharmaceutical accumulation in the body. Used to diagnose a variety of diseases (for example tumours, heart disease, brain disorders). Provides a picture of the body working.[3]
- SPECT (Single photon emission computed tomography) similar to PET, is a nuclear medicine imaging techniques which provide metabolic and functional information unlike CT and MRI.[4]
Hybrid Imaging[edit | edit source]
Hybrid Imaging is the fusion of two (or more) imaging modalities to form a new technique[5]. By combining the innate advantages of the fused imaging technologies synergistically, usually a new and more powerful modality comes into being. Existing hybrid imaging modalities include: PET-CT, SPECT-CT, MRI-PET, MRI-SPECT
The general benefits of hybrid imaging include: Increased diagnostic accuracy, precise monitoring of interventional procedure and reduced radiation exposure, e.g. dynamic US after obtaining CT map.
Photoacoustic Imaging (PA)[edit | edit source]
Also known as Optoacoustic Imaging, is an upcoming biomedical imaging modality availing the benefits of optical resolution and acoustic depth of penetration. Optoacoustic imaging has demonstrated promising potential in a wide range of preclinical and clinical applications.[6] Clinical applications of optoacoustic imaging include: Musculoskeletal Imaging; Gastrointestinal Imaging; Breast imaging; Dermatologic Imaging eg Skin cancer; Vascular Imaging; Carotid Vessel Imaging.[6]
Studies have showed the potential use of optoacoustic imaging in the assessment, diagnosis and monitoring of treatment in patients with inflammatory arthritis[7] as well as limb and muscle ischemia.[8]
Necessity of Medical Imaging[edit | edit source]
Medical imaging is crucial in a variety of medical setting and at all major levels of health care. In public health and preventive medicine as well as in both curative and palliative care, effective decisions depend on correct diagnoses. Though clinical reasoning may be sufficient prior to treatment of many conditions, the use of diagnostic imaging services is paramount in confirming, correctly assessing and documenting courses of many diseases as well as in assessing responses to treatment.
Caution with Imaging[edit | edit source]
Imaging is a useful resource for many conditions and is an invaluable tool for clinicians/physiotherapists when used appropriately. It is important to know when imaging is appropriate, as unnecessary imaging will squander financial resources and increase the potential for premature surgery/ iatrogenic effects.
Early or unnecessary referral for imaging may be influenced by patient expectations and clinician concerns, or may be used as way to reassure patients. These factors need to be managed with good communication and evidence based guidelines.[9]
Also see: Diagnostic Imaging Best Practice
Iatrogenic Effects[edit | edit source]
Abnormal radiologic findings of the musculoskeletal system can be very common. Not all abnormalities are relevant to a patient's complaint and over-emphasising radiologic findings can have harmful effects.
- Routine MRI reports produce worse functional outcomes compared to a 'clinical report' (which includes reassurance of incidental findings) in patients with low back pain.[10]
- Early-MRI in acute low back pain results in longer length of disability, higher medical cost and worse outcomes regardless of radiculopathy (even after controlling for severity and demographics)[9]
It is therefore very important to carefully consider whether imaging is indicated, and to always view the results in the context of an in depth history and physical examination. This will help to discern whether findings correlate with the patient's complaint, or are in fact incidental and negligible.
Radiation[edit | edit source]
Even though most imaging techniques use low doses of radiation, large, repeated doses have a cumulative effect and can be harmful to human health (including cancer and tissue damage). "Image gently" and "Image wisely" are initiatives that promote practices that reduce radiation exposure by eliminating unnecessary procedures (see resource section).[11]Modern techniques have also resulted in reductions in radiation exposure during imaging.
Factors that should be considered include a patient's age and lifetime exposure to radiation, as well as whether the benefit of the diagnostic test outweighs the risk. CT-scans have higher radiation risk than x-rays, whereas no ionising radiation is produced during MRI or ultrasound scans.[12]
Radiation risk is of particular concern in the following scenarios:[12]:
- During infancy and early childhood
- During pregnancy (especially early)
Asymptomatic Findings[edit | edit source]
Although advanced imaging is generally very sensitive, it can be very non-specific. Various studies have found that imaging findings and symptoms often do not correlate. Consider the table below - these findings provide evidence that what we regard as pathology may not be that significant. Also see the pages on imaging of specific body regions for more detail:
| Pathology | Prevalence among asymptomatic population |
|---|---|
| Lumbar disc herniation and/or spinal stenosis | 20- 75% |
| Cervical disc bulging | 75 - 90%[13] |
| Cervical spinal cord compression | 7 - 35% [14] |
| Rotator cuff tendinopathy | 25 - 89% [15] |
| Mild glenohumeral or acromioclavicular OA 12 | 50 - 70%[15] |
| Hip labrum tear 13/14 | 54% [16] |
| Knee Meniscal abnormalities and OA 19 | 60% [17] |
Health Care Team[edit | edit source]
Imaging for medical purposes involves a team which includes the service of radiologists, radiographers (x-ray technologists), sonographers (ultrasound technologists), medical physicists, nurses, biomedical engineers, and other support staff working together. Appropriate use of medical imaging requires a multidisciplinary approach.[1]
Conclusion[edit | edit source]
Medical imaging is a crucial component of healthcare and provide a valuable tool for diagnosis, screening and treatment. It is however important to follow best practice guidelines with a particular focus on avoiding unnecessary imaging and ensuring appropriate, evidence-based interpretation of results. We treat whole, complex persons - not images and scans.
Diagnostic Imaging for Body Regions[edit | edit source]
- Diagnostic Imaging of the Hip for the Physical Therapist
- Diagnostic Imaging of the Knee for the Physical Therapist
- Diagnostic Imaging of the Ankle and Foot for the Physical Therapist
- Diagnostic Imaging of the Shoulder
References[edit | edit source]
- ↑ 1.0 1.1 WHO Diagnostic Imaging Available from: https://www.who.int/diagnostic_imaging/en/(accessed 7.4.2021)
- ↑ Radiopedia Nuclear medicine Available:https://radiopaedia.org/articles/nuclear-medicine (accessed 8.10.20220
- ↑ Radiopedia PET Available: https://radiopaedia.org/articles/positron-emission-tomography(accessed 8.10.2022)
- ↑ Radiopedia SPECT vs PET Available:https://radiopaedia.org/articles/spect-vs-pet (accessed 8.10.2022)
- ↑ Radiopedia Modalities Available from:https://radiopaedia.org/articles/modality?lang=us (accessed 7.4.2021)
- ↑ 6.0 6.1 Amalina Binte Ebrahim Attia, Ghayathri Balasundaram, Mohesh Moothanchery, U.S. Dinish, Renzhe Bi, Vasilis Ntziachristos, Malini Olivo, A review of clinical photoacoustic imaging: Current and future trends, Photoacoustics, Volume 16, 2019, 100144, ISSN 2213-5979, obtained from https://www.sciencedirect.com/science/article/pii/S2213597919300679 doi: 10.1016/j.pacs.2019.100144
- ↑ Jo J, Tian C, Xu G, et al. Photoacoustic tomography for human musculoskeletal imaging and inflammatory arthritis detection. Photoacoustics. 2018;12:82–89. Published 2018 Jul 27 obtained from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6306364/ doi:10.1016/j.pacs.2018.07.004
- ↑ Chen L, Ma H, Liu H, et al. Quantitative photoacoustic imaging for early detection of muscle ischemia injury. Am J Transl Res. 2017;9(5):2255–2265. Published 2017 May 15 obtained from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5446508/
- ↑ 9.0 9.1 Webster BS, Bauer AZ, Choi Y, Cifuentes M, Pransky GS. Iatrogenic consequences of early magnetic resonance imaging in acute, work-related, disabling low back pain. Spine. 2013 Oct 15;38(22):1939-46.
- ↑ Rajasekaran S, Dilip Chand Raja S, Pushpa BT, Ananda KB, Ajoy Prasad S, Rishi MK. The catastrophization effects of an MRI report on the patient and surgeon and the benefits of ‘clinical reporting’: results from an RCT and blinded trials. European Spine Journal. 2021 Jul;30:2069-81.
- ↑ Ford B, Dore M, Moullet P. Diagnostic imaging: appropriate and safe use. American Family Physician. 2021 Jan 1;103(1):42-50.
- ↑ 12.0 12.1 Mafraji, M.A. Risk of Radiation in Medical Imaging [Internet]. Merck Manuals. 2023 [updated 2023 November; cited 2024 March]. Available from: https://www.msdmanuals.com/home/special-subjects/common-imaging-tests/computed-tomography-ct
- ↑ Nakashima H, Yukawa Y, Suda K, Yamagata M, Ueta T, Kato F. Abnormal findings on magnetic resonance images of the cervical spines in 1211 asymptomatic subjects. Spine. 2015 Mar 15;40(6):392-8.
- ↑ Smith SS, Stewart ME, Davies BM, Kotter MR. The prevalence of asymptomatic and symptomatic spinal cord compression on magnetic resonance imaging: a systematic review and meta-analysis. Global spine journal. 2021 May;11(4):597-607.
- ↑ 15.0 15.1 Girish G, Lobo LG, Jacobson JA, Morag Y, Miller B, Jamadar DA. Ultrasound of the shoulder: asymptomatic findings in men. American Journal of Roentgenology. 2011 Oct;197(4):W713-9.
- ↑ Heerey, J.J., Kemp, J.L., Mosler, A.B., Jones, D.M., Pizzari, T., Souza, R.B. and Crossley, K.M., 2018. What is the prevalence of imaging-defined intra-articular hip pathologies in people with and without pain? A systematic review and meta-analysis. British Journal of Sports Medicine, 52(9), pp.581-593.
- ↑ Englund M, Guermazi A, Gale D, Hunter DJ, Aliabadi P, Clancy M, Felson DT. Incidental meniscal findings on knee MRI in middle-aged and elderly persons. New England Journal of Medicine. 2008 Sep 11;359(11):1108-15.