Malignant Melanoma: Difference between revisions
No edit summary |
No edit summary |
||
| Line 126: | Line 126: | ||
*<u>Temodar</u>: Temodar is an alkylating agent that slows the development and growth of cancer cells. It is often used when other medications are not successful. Common side effects include constipation, headache, nausea, vomiting, unusual fatigue, and weakness. <ref name="DRUGS">Melanoma Medications. Drugs.com. Available at: http://www.drugs.com/condition/malignant-melanoma.html. Accessed at: March 18, 2014.</ref><br> | *<u>Temodar</u>: Temodar is an alkylating agent that slows the development and growth of cancer cells. It is often used when other medications are not successful. Common side effects include constipation, headache, nausea, vomiting, unusual fatigue, and weakness. <ref name="DRUGS">Melanoma Medications. Drugs.com. Available at: http://www.drugs.com/condition/malignant-melanoma.html. Accessed at: March 18, 2014.</ref><br> | ||
*<u>Yervoy</u>: Yervoy is an anti-CTLA-4 monoclonal antibody that inhibits the growth and spread of cancer cells. It is used for patients that are not surgical candidates to treat melanoma. Common side effects include diarrhea, severe stomach pain, vomiting, fever, itching skin, and rash. | *<u>Yervoy</u>: Yervoy is an anti-CTLA-4 monoclonal antibody that inhibits the growth and spread of cancer cells. It is used for patients that are not surgical candidates to treat melanoma. Common side effects include diarrhea, severe stomach pain, vomiting, fever, itching skin, and rash. <ref name="DRUGS" /> | ||
*<u>Intron A</u>: Intron A is an antineoplastic interferon that enhances the immune system's ability to fight cancer cells. Common side effects include depression, shortness of breath, wheezing, swelling of the face, chest tightness, and weight loss. | *<u>Intron A</u>: Intron A is an antineoplastic interferon that enhances the immune system's ability to fight cancer cells. Common side effects include depression, shortness of breath, wheezing, swelling of the face, chest tightness, and weight loss. <ref name="DRUGS" /> | ||
*<u>Pegintron</u>: Pegintron is an antineoplastic and antiviral interferon that may prevent the cancer cells from spreading and growing as well as the recurrence of melanoma. Common side effects include anxiety, chills, mood swings, fever, infection, and pale skin. | *<u>Pegintron</u>: Pegintron is an antineoplastic and antiviral interferon that may prevent the cancer cells from spreading and growing as well as the recurrence of melanoma. Common side effects include anxiety, chills, mood swings, fever, infection, and pale skin. <ref name="DRUGS" /> | ||
*<u>Sylatron</u>: Sylatron is an antineoplastic and antiviral interferon that is used to prevent the return of malignant melanoma after surgical removal. Common side effects include anxitey, chills, mood swings, fever, infection, and pale skin. | *<u>Sylatron</u>: Sylatron is an antineoplastic and antiviral interferon that is used to prevent the return of malignant melanoma after surgical removal. Common side effects include anxitey, chills, mood swings, fever, infection, and pale skin. <ref name="DRUGS" /> | ||
*<u>Proleukin</u>: Proleukin is an interleukin and antineoplastic is used when treating malignant melanoma that has metastasized to other areas of the body. It enhances the immune system to reduce cancer growth and development. Common side effects include tingling of the hands or feet, mouth sores, weight gain, fever, chills, and dizziness. | *<u>Proleukin</u>: Proleukin is an interleukin and antineoplastic is used when treating malignant melanoma that has metastasized to other areas of the body. It enhances the immune system to reduce cancer growth and development. Common side effects include tingling of the hands or feet, mouth sores, weight gain, fever, chills, and dizziness. <ref name="DRUGS" /> | ||
*<u>DTIC-Dome</u>: DTIC-Dome is an alkylating agent that is used when treating advanced melanoma and helps block the growth of cancer cells. This drug is administered via injection. Common side effects include redness, pain, or swelling at injection site. | *<u>DTIC-Dome</u>: DTIC-Dome is an alkylating agent that is used when treating advanced melanoma and helps block the growth of cancer cells. This drug is administered via injection. Common side effects include redness, pain, or swelling at injection site. <ref name="DRUGS" /> | ||
*<u>Imiquimod Cream</u>: Imiquimod Cream is an immune response modifier that stops the abnormal cell growth. This topical cream is used for patients that are not surgical candidates to treat melanoma. Common side effects include redness, drying, flaking, scaling, scabbing, or crusting of the skin where the cream is applied. <ref name="ACS" /> | *<u>Imiquimod Cream</u>: Imiquimod Cream is an immune response modifier that stops the abnormal cell growth. This topical cream is used for patients that are not surgical candidates to treat melanoma. Common side effects include redness, drying, flaking, scaling, scabbing, or crusting of the skin where the cream is applied. <ref name="ACS" /> | ||
*<u>Bacille Calmette-Guerin "BCG" Vaccine</u>: BCG is a germ that activates the immune systems in humans. Although it cannot isolate malanoma cells, it may be used via injection into specific tumor sites. Common side effects include redness at injection site, fever, vomiting, blood in urine, and swollen lymph nodes. <ref name="ACS" /> | *<u>Bacille Calmette-Guerin "BCG" Vaccine</u>: BCG is a germ that activates the immune systems in humans. Although it cannot isolate malanoma cells, it may be used via injection into specific tumor sites. Common side effects include redness at injection site, fever, vomiting, blood in urine, and swollen lymph nodes. <ref name="ACS" /> | ||
Revision as of 01:32, 19 March 2014
Original Editors - Emily Erwin & Brooke Sowards from Bellarmine University's Pathophysiology of Complex Patient Problems project.
Top Contributors - Emily Erwin, Ellen Hosking, Brooke Sowards, Lucinda hampton, Elaine Lonnemann, Kim Jackson, Vidya Acharya, Calli Paydo, WikiSysop, 127.0.0.1 and Wendy Walker
Definition/Description[edit | edit source]
Malignant Melanoma is a cancer that begins in a specific type of skin cells known as melanocytes. This type of cancer may also be known as melanoma or cutaneous melanoma.
Melanocytes are located in the most superficial layer of skin, the epidermis. The epidermis protects the underlying dermis and subcutaneous tissue layers of the skin. Melanocytes are found in the basal layer, or the lowest layer, of the epidermis. These cells produce a brown pigment known as melanin, which gives the skin its tan appearance. After sun exposure, additional melanin is produced, resulting in a darkening or "tanning" of the skin. Melanin also plays an integral role in preventing skin damage from the sun's harmful rays. [1]
Malignant growths may occur following damage to skin cell DNA. If unrepaired, this damage initiates mutations that result in rapid proliferation of skin cells that form malignant tumors. [2]
Prevalence/Risk Factors
[edit | edit source]
Although Malignant Melanoma accounts for less than 2% of total skin cancer cases, it causes a much larger percentage of skin cancer deaths. The American Cancer Society predicts for melanoma in the United States for 2014:
- Approximately 76,100 new melanomas will be diagnosed (43,890 in men and 32,210 in women)[1]
- Aproximately 9,710 people are expected to die of melanoma (6,470 men and 3,240 women)[1]
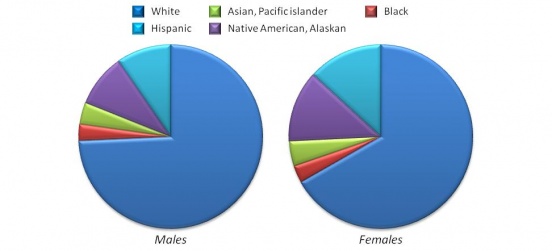
Overall, melanoma is more common in men than women. However, before the age of 40 the risk is higher for women and after the age of 40 the risk is higher for men. Although it is more likely to occur in the older population, it is one of the most common cancers in young individuals, particularly women under the age 30. The incidence of new cases is higher among whites than any other racial/ethnic group. [3] Whites with light hair color, blue or green eyes, or fair skin that easily burns are at an increased risk. [1]
An individual’s risk of developing melanoma is also greater if an immediate relatives such as a parent, brother, sister, or child, has had melanoma. Around 10% of all people with melanoma report a positive family history of the disease. This increased risk could be associated with a similar lifestyle of frequent sun exposure, a common characteristic of fair skin, or a combination of factors. It may also be caused by gene mutations that are hereditary. In families that have a high rate of melanoma, up to 40% have a known gene mutation. [1]
Another major risk factor for developing melanoma is the excessive exposure to UV radiation through sunlight and tanning booths. There are three types of UV rays; UVA, UVB, UVC. UVA and UVB, which are found in sunlight and tanning booths, cause damage to skin cell DNA which promotes the development of melanoma. UVC rays are not found in sunlight therefore are not damaging or associated with melanoma. [4]
Characteristics/Clinical Presentation[edit | edit source]
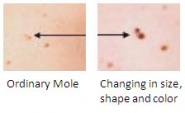
The most common early indication of malignant melanoma is often the presence of an abnormal mole. There are five specific characteristics that can help you identify whether a mole is cancerous or not. Health care professionals may educate patients on the “ABCDE” warning signs of melanoma. Research with digital imaging has confirmed that the ABCDE warning signs have a sensitivity ranging from 57% to 90% and a specificity from 59% to 90%.[5]
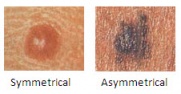
A = Asymmetry; uneven edges, lopsided in shape, one half unlike the other half. If you draw a line through the asymmetrical mole, the two halves will not match. [2][5]
B = Border; irregularity, irregular edges, scalloped, notched, or poorly defined edges[2][5]
C = Color; black, shades of brown, red, white, occasionally blue. Having multiple colors present is also an abnormal finding.[2][5]
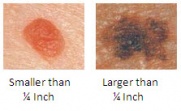
D = Diameter; larger than a pencil eraser (1/4 in or 6 mm)[2][5]
E = Evolving; mole or skin lesion that looks different from the rest, or is changing in size, shape, or color. Other changes, such as bleeding, itching, or crusting, may also occur.[2][5]
Associated Comorbidities
[edit | edit source]
Individuals who have been diagnosed with dysplastic nevus syndrome often develop malignant melanoma later in life. This syndrome, also known as atypical mole syndrome, is a familial disorder that results in a significant number of large moles that have an irregular shape or color. They frequently appear on skin that is exposed to the sun but can develop anywhere on the body. The dysplastic nevi have up to a 50% chance of developing into malignant melanoma; therefore, they are often surgically removed to prevent cancer. Individuals with this syndrome are encouraged to have routine skin exams by a dermatologist and should preform monthly self skin exams. [4][1]
There are no specific comorbidities that are closely linked to malignant melanoma. However, individuals with melanoma may present with a variety of common comorbidities such as congestive heart failure, peripheral vascular disease, dementia, diabetes mellitus, and pulmonary disease. Research has shown an association between comorbidities such as these with delay of melanoma diagnosis, more advanced stages of melanoma, and less aggressive treatments. Therefore, improved efforts to treat these comorbidities may result in decreased mortality rates among individuals with melanoma.[6]
Medications[edit | edit source]
- Temodar: Temodar is an alkylating agent that slows the development and growth of cancer cells. It is often used when other medications are not successful. Common side effects include constipation, headache, nausea, vomiting, unusual fatigue, and weakness. [7]
- Yervoy: Yervoy is an anti-CTLA-4 monoclonal antibody that inhibits the growth and spread of cancer cells. It is used for patients that are not surgical candidates to treat melanoma. Common side effects include diarrhea, severe stomach pain, vomiting, fever, itching skin, and rash. [7]
- Intron A: Intron A is an antineoplastic interferon that enhances the immune system's ability to fight cancer cells. Common side effects include depression, shortness of breath, wheezing, swelling of the face, chest tightness, and weight loss. [7]
- Pegintron: Pegintron is an antineoplastic and antiviral interferon that may prevent the cancer cells from spreading and growing as well as the recurrence of melanoma. Common side effects include anxiety, chills, mood swings, fever, infection, and pale skin. [7]
- Sylatron: Sylatron is an antineoplastic and antiviral interferon that is used to prevent the return of malignant melanoma after surgical removal. Common side effects include anxitey, chills, mood swings, fever, infection, and pale skin. [7]
- Proleukin: Proleukin is an interleukin and antineoplastic is used when treating malignant melanoma that has metastasized to other areas of the body. It enhances the immune system to reduce cancer growth and development. Common side effects include tingling of the hands or feet, mouth sores, weight gain, fever, chills, and dizziness. [7]
- DTIC-Dome: DTIC-Dome is an alkylating agent that is used when treating advanced melanoma and helps block the growth of cancer cells. This drug is administered via injection. Common side effects include redness, pain, or swelling at injection site. [7]
- Imiquimod Cream: Imiquimod Cream is an immune response modifier that stops the abnormal cell growth. This topical cream is used for patients that are not surgical candidates to treat melanoma. Common side effects include redness, drying, flaking, scaling, scabbing, or crusting of the skin where the cream is applied. [1]
- Bacille Calmette-Guerin "BCG" Vaccine: BCG is a germ that activates the immune systems in humans. Although it cannot isolate malanoma cells, it may be used via injection into specific tumor sites. Common side effects include redness at injection site, fever, vomiting, blood in urine, and swollen lymph nodes. [1]
Diagnostic Tests/Lab Tests/Lab Values[edit | edit source]
add text here
Etiology/Causes[edit | edit source]
add text here
Systemic Involvement[edit | edit source]
discuss common metastases here. p 504 diff dx book
Medical Management (current best evidence)[edit | edit source]
add text here
Physical Therapy Management (current best evidence)[edit | edit source]
add text here
Alternative/Holistic Management (current best evidence)[edit | edit source]
add text here
Differential Diagnosis[edit | edit source]
add text here
Case Reports/ Case Studies[edit | edit source]
add links to case studies here (case studies should be added on new pages using the case study template)
Resources
[edit | edit source]
add appropriate resources here
Recent Related Research (from Pubmed)[edit | edit source]
see tutorial on Adding PubMed Feed
Extension:RSS -- Error: Not a valid URL: addfeedhere|charset=UTF-8|short|max=10
References[edit | edit source]
see adding references tutorial.
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 Melanoma Skin Cancer. American Cancer Society. Available at http://www.cancer.org/cancer/skincancer-melanoma/index. Accessed March 17, 2014.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 Melanoma. Skin Cancer Foundation. Available at http://www.skincancer.org/skin-cancer-information/melanoma. Accessed March 17, 2014.
- ↑ SEER Stat Fact Sheets: Melanoma of the Skin. National Cancer Institute. Available at: http://seer.cancer.gov/statfacts/html/melan.html. Accessed: March 17, 2014
- ↑ 4.0 4.1 Goodman C, Fuller K. The Integumentary System. In: Pathology Implications for the Physical Therapist. 3rd ed. St. Louis, MO: Saunders Elsevier; 2009: 392-452.
- ↑ 5.0 5.1 5.2 5.3 5.4 5.5 Goodman CC, Snyder TE. Screening for Cancer. In: Differential Diagnosis for Physical Therapists, Screening for Referral. W B Saunders Company; 2012: 487-543.
- ↑ A F Grann, T Frøslev, A B Olesen, H Schmidt, T L Lash. The impact of comorbidity and stage on prognosis of Danish melanoma patients, 1987–2009: a registry-based cohort study [Internet]. British Journal of Cancer. 2013. p. 265–71. Available from: http://www.nature.com/bjc/journal/v109/n1/full/bjc2013246a.html
- ↑ 7.0 7.1 7.2 7.3 7.4 7.5 7.6 Melanoma Medications. Drugs.com. Available at: http://www.drugs.com/condition/malignant-melanoma.html. Accessed at: March 18, 2014.