Madelung's Deformity: Difference between revisions
No edit summary |
No edit summary |
||
| Line 19: | Line 19: | ||
== Pathogenesis == | == Pathogenesis == | ||
Premature growth plate arrest at the medial volar aspect of the distal radius causes Madelung deformity. Repetitive traumatic pressure may result in Madelung-like deformity. Mutation or absence of the short stature homeobox (SHOX) gene is thought to be the cause of congenital | Premature growth plate arrest at the medial volar aspect of the distal radius causes Madelung deformity. Repetitive traumatic pressure may result in Madelung-like deformity. Mutation or absence of the short stature homeobox (SHOX) gene is thought to be the cause of congenital Madelung deformity. | ||
Congenital | Congenital Madelung deformity can occur as a part of Leri-Weill dyschondrosteosis (LWD) or Turner syndrome.<ref>Tranmer A, Laub Jr D. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4993032/ Madelung deformity]. ''Eplasty''. 2016;16.</ref> | ||
== Diagnosis == | == Diagnosis == | ||
| Line 38: | Line 38: | ||
* Turner syndrome | * Turner syndrome | ||
* Nail-patella syndrome | * Nail-patella syndrome | ||
* Hereditary, multiple | * Hereditary, multiple exostoses | ||
* Ollier’s disease | * Ollier’s disease | ||
* [[Achondroplasia]] | * [[Achondroplasia]] | ||
| Line 47: | Line 47: | ||
==== '''Conservative Management''' ==== | ==== '''Conservative Management''' ==== | ||
Conservative management of Madelung’s deformity may be helpful for skeletally mature patients with following measures: | Conservative management of Madelung’s deformity may be helpful for skeletally mature patients with the following measures: | ||
* physiotherapy for wrist strengthening and to reduce pain<ref>Limb Lengthening and Reconstruction Society. Madelung Deformity. Available from: https://llrs.org/information-for-patients/specific-conditions/madelung/ [Last accessed on 27 December 2020] | |||
</ref> | |||
* oral analgesics | * oral analgesics | ||
* activity restriction | * activity restriction | ||
Revision as of 07:05, 27 December 2020
Introduction[edit | edit source]
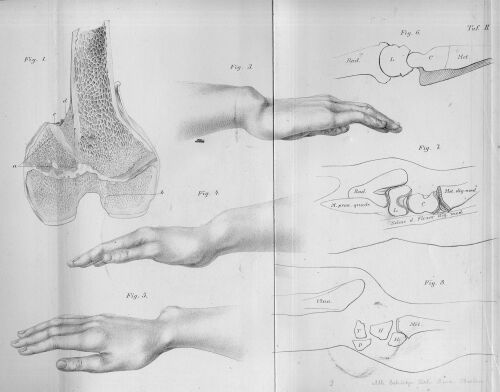
Madelung’s deformity is a condition of the wrist characterized by a shortened distal radius with volar–ulnar curvature and a dorsally prominent distal ulna.[1]
A Vickers’ ligament is the feature to differentiate Madelung’s deformity from Madelung-like deformities.[2]
Epidemiology[edit | edit source]
Predominantly adolescent females are affected by a ratio of 4:1. The deformity is bilateral most often.[3]
Clinical Features[edit | edit source]
- Initially asymptomatic, progressive clinical deformity
- Pain at wrist
- Loss of wrist extension
- Compromised forearm rotation
- “Bayonet” deformity- prominent distal ulna as a result of dorsal subluxation[4]
- Girls are more often affected than boys
- Presents between the ages of 6 and 13 years[5]
Pathogenesis[edit | edit source]
Premature growth plate arrest at the medial volar aspect of the distal radius causes Madelung deformity. Repetitive traumatic pressure may result in Madelung-like deformity. Mutation or absence of the short stature homeobox (SHOX) gene is thought to be the cause of congenital Madelung deformity.
Congenital Madelung deformity can occur as a part of Leri-Weill dyschondrosteosis (LWD) or Turner syndrome.[6]
Diagnosis[edit | edit source]
Key Features from X-Ray[edit | edit source]
- increased dorsal and radial convexity of the distal radius
- increased volar and ulnar tilt of the distal radial articular surface
- widened interosseous space
- relative dorsal position of the ulnar head
- pyramiding of the carpus[3]
MRI[edit | edit source]
MRI is done on the patients who need the surgical release of Vickers’ ligament to prevent deformity progression.[5]
Differential Diagnosis[edit | edit source]
- Turner syndrome
- Nail-patella syndrome
- Hereditary, multiple exostoses
- Ollier’s disease
- Achondroplasia
- Multiple epiphyseal dysplasias
- Mucopolysaccharidoses (Hurler and Morquio syndrome)[7]
Treatment[edit | edit source]
Conservative Management[edit | edit source]
Conservative management of Madelung’s deformity may be helpful for skeletally mature patients with the following measures:
- physiotherapy for wrist strengthening and to reduce pain[8]
- oral analgesics
- activity restriction
- volar splint[9]
Surgical Management[edit | edit source]
References[edit | edit source]
- ↑ Dubey A, Fajardo M, Green S, Lee SK. Madelung’s deformity: a review. Journal of Hand Surgery (European Volume). 2010 Mar;35(3):174-81.
- ↑ Prasad N, Venkatesh M. Madelung Deformity of the Wrist: A Classic Presentation. International Journal of Contemporary Medicine Surgery and Radiology. 2020;5:C4-5
- ↑ 3.0 3.1 Thomson C, Hawkes D, Nixon M. Madelung’s Deformity: Diagnosis, Classification and Treatment. Journal of Orthoplastic Surgery. 2020 Apr 17;4(1):1-1.
- ↑ Babu S, Turner J, Seewoonarain S, Chougule S. Madelung's Deformity of the Wrist—Current Concepts and Future Directions. Journal of wrist surgery. 2019 Jun;8(03):176-9.
- ↑ 5.0 5.1 Knutsen EJ, Goldfarb CA. Madelung's deformity. Hand. 2014 Sep;9(3):289-91.
- ↑ Tranmer A, Laub Jr D. Madelung deformity. Eplasty. 2016;16.
- ↑ Kakarla S. Madelung and pseudo Madelung deformities-Pictorial essay. Journal of Medical and Scientific Research. 2019;7:1-6
- ↑ Limb Lengthening and Reconstruction Society. Madelung Deformity. Available from: https://llrs.org/information-for-patients/specific-conditions/madelung/ [Last accessed on 27 December 2020]
- ↑ Shahi P, Sudan A, Sehgal A, Meher D, Meena U. Madelung Deformity of the Wrist Managed Conservatively. Cureus. 2020 May;12(5).
- ↑ Bebing M, de Courtivron B, Pannier S, Journeau P, Fitoussi F, Morin C, Violas P. Madelung's deformity in children: Clinical and radiological results from a French national multicentre retrospective study. Orthopaedics & Traumatology: Surgery & Research. 2020 Nov 1;106(7):1339-43.