Lung Cancer
Original Editor - Sarah Hansford and Kaden Johnson Top Contributors - Sarah Hansford, Lucinda hampton, Kaden Johnson, Kim Jackson, Vidya Acharya, Admin, WikiSysop, Kapil Narale, Aya Alhindi, 127.0.0.1, Mariam Hashem, Michelle Lee and Adam Vallely Farrell
Introduction[edit | edit source]
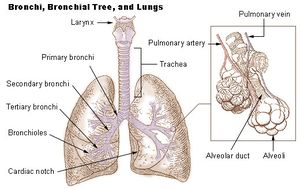
Lung cancer refers to tumors originating in the lung parenchyma or within bronchi. It is:
- A broad term referring to the main histological subtypes of primary lung malignancies that are mainly linked with inhaled carcinogens, with cigarette smoke being a key culprit.[1]
- The most common cancer worldwide, with 2 million new cases in 2018[2].
- One of the leading causes of cancer-related deaths in the United States.
At the beginning of the 20th century, lung cancer was a relatively rare disease. Its dramatic rise in later decades is mostly attributable to the increase in smoking among both males and females[3]
Epidemiology[edit | edit source]
Lung cancer is one of the most common and serious types of cancer. It is the second highest cancer incidence in both males and females, following prostate cancer in men and breast cancer in women.[4] It is diagnosed in over 41,000 people every year in the UK and is the leading cause of cancer death around the world.[4] In 2008, lung cancer contributed to 13% or 1.6 million of total cancer cases and 18% or 1.4 million cancer-related deaths worldwide.[4] Lung cancer incidence and mortality rates are highest in the United States and developed countries and almost 9 in 10 lung cancer cases occur in people aged 60 years or older.[4]
Aetiology[edit | edit source]
Smoking[edit | edit source]
Cigarette smoking is the leading cause of lung cancer and accounts for about 85% of diagnosed lung cancer patients. Smoking is also most strongly associated with small cell lung cancer and squamous-cell carcinoma.[5] Risk for lung cancer increases with how long a person has been smoking, the amount they smoke and the depth of smoke inhalation. Second-hand smoking also causes lung cancer, but is less strongly associated compared to active smoking. Cigarettes contain more than 60 carcinogens that have been shown to induce cancers. Nicotine causes addiction to cigarette smoking and has been shown to inhibit apoptosis, proliferate cells, and cause angiogenesis in lung tumours.[6] Cigar and pipe tobacco smoking produces relatively large particles that only reach the upper airways, where cigarette smoking reaches the distal airways because it produces fine particles.[6] Therefore, the risk of lung cancer is lower with cigar and pipe smoking. Smokers of all ages will benefit from the cessation of smoking, but the risk of developing lung cancer will still be increased compared to never smokers. Never smokers are individuals who smoked fewer than 100 cigarettes in their lifetime but this still accounts for 25% of lung cancers worldwide.[6]
Occupational and Environmental Exposure[edit | edit source]
A number of environmental risk factors have been identified, most of which often relates to occupational exposures such as asbestos, tar, soot, and a number of metals such as arsenic, chromium, and nickel. Air pollution has also been linked to increased risk of lung cancer.[6] Radon gas has been posed as a significant risk factor for lung cancer as well.[6] Genetics There is a genetic susceptibility which increases the risk of lung cancer among first-degree relatives.[6]
Other factors There are several other factors that increase the risk of developing lung cancer, and they include:[edit | edit source]
- Gender (men more predisposed than women)
- Dietary factors
- Individuals with chronic obstructive pulmonary disease
- Ethnicity
Investigations[edit | edit source]
Chest X-ray[edit | edit source]
A chest X-ray is usually the first step in diagnosing lung cancer. Tumours usually appear as white/grey masses.[7] Chest X-rays do not always give a clear enough diagnosis, due to the fact that they can’t distinguish between multiple conditions (ex. consolidation and lung abscess)
CT scan[edit | edit source]
A CT scan or Computerised (axial) tomography scan, usually carried out after a chest X-ray, takes a series of x-rays at different angles and through the use of computer processors produces a series of cross-sectional images of specific areas of a scanned object, allowing the user to see inside the object.[7] This scan gives a very accurate picture of where a tumour is and its size. Before having a CT scan, you will be given an injection of a contrast medium. This is a liquid containing a dye that makes the lungs show up more clearly on the scan. The scan is painless and takes 10-30 minutes to complete.[7]
PET-CT scan[edit | edit source]
A PET-CT or Positron Emission Tomography computerised tomography,is usually conducted if the results of a CT scan show an early stage cancer. the PET-CT is able to identify where there are active cancer cancer cells.[7] These results are quite useful in helping with diagnosis and treatment.Before undergoing a PET-CT the individual is injected with a slightly radioactive material. The scanner then works by detecting the radiation given off by the injected radiotracer. [7]
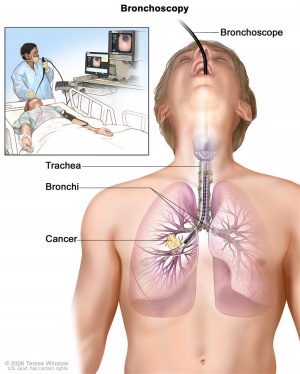
Bronchoscopy and Biopsy[edit | edit source]
A bronchoscopy is a procedure that allows a physician to remove a small sample of cells from the inside of the lung using a bronchoscope.[7] The bronchoscope is a small tube like device which is passed through the mouth or nose and down through the throat into the airways.[7] This procedure is slightly uncomfortable however it is relatively quick and only takes a few minutes.
Other types of biopsies include:
- Percutaneous needle biopsy
- Thoracoscopy
- Mediastinoscopy
- Screening
According to the NHS there is currently no national screening program for lung cancer in the UK.[7] The lack of a National screening program is due to the complexity of the tests required to identify lung cancer. No simple, and quick test sensitive enough to outweigh possible risks associated with screening is yet available (ex. radiation exposure during x-rays).
Clinical Manifestations[edit | edit source]
Clinical manifestations that may be presented include:
Cough
- Presence of mass irritates the cough receptors in the airway[5]
- Release of sputum
- More common in squamous cell carcinoma and small cell lung cancer (more commonly found in the central airways)
- Obstruction from central airway could also lead to post-obstructive pneumonia and distal atelectasis[5]
Weight loss
- Cancer induced proteolysis and lipolysis leads to loss of muscle and adipose tissue.[5]
- Loss of appetite also contributes to weight loss
Hemoptysis
- Tumor in the central airway
- Tumor-induced angiogenesis result in blood vessels that are leaky and twisted, leading to easy ruptures and causing hemoptysis[5]
Dyspnea
- Obstruction of Airway leading to shortness of breath
- Mechanoreceptors and chemoreceptors are activated in the lungs due to cachexia or hypoxemia/acidosis[5]
Chest pain
- Tumor involving pleural surface causing pleuritic chest pain[9]
Pleural effusion (chest pain, dyspnea)
- Benign pleural effusion may be due to lymphatic obstruction, post-obstructive pneumonitis, or atelectasis[5]
- Malignant pleural effusion occurs when malignant cells and present in pleural fluid[9]
Other signs and symptoms include:
- Wheezing
- Nausea/Vomiting
- Swelling of face and arms
- Fatigue
- Bone pain
- Clubbing
- Headache
- Seizures
Physiotherapy and Other Management[edit | edit source]
Physiotherapy management[edit | edit source]
I have shown it that hydration, autogenic drainage, gentle suctioning, postural drainage, chest physiotherapy, and external oscillation applications can be useful for patients with lung cancer.[10] The study by Hoffman L et al.[11] showed positive outcomes with inspiratory muscle training in patients with advanced lung disease. Smoking cessation is a very important form of management with lung cancer patients. In addition to education, counselling, and support for quitting smoking, there are three main interventions that are used which include:
- Nicotine replacement therapy (NRT): Available in many forms including gum and a transdermal patch. All forms of nicotine replacement increases the rate of quitting by 50-70%.[5]
- Antidepressants: bupropion and nortriptyline are as effective as nicotine replacement therapy[5]
- Nicotine receptor partial agonist: varenicline is more effective than bupropion and NRT.[5]
Exercise[edit | edit source]
Aerobic exercise and resistance training have a positive impact on lung functioning including a reduction in airflow obstruction and clearing of airways therefore the improved functional capabilities increase energy levels and the release of sputum.[10] Exercise programs should be supervised by the treating clinical team and should also be discussed with the general practitioner before participating in any exercise program. Surgery involves resection of the tumor and some normal tissue around it. This is the first line of choice of treatment for non-small cell lung cancer patients who are medically fit to undergo surgery.[9] An exploratory secondary trial data analysis suggests that breathlessness services must be easily accessible to patients and patients should be encouraged and assisted to attend[12]. Research shows positive results of physical exercises on cancer-related fatigue, physical function, symptom distress, sarcopenia and health-related quality of life (HRQoL)[13].
Radiation Therapy[edit | edit source]
Radiation therapy is a form of treatment that is indicated for patients with stage I, II or III of non-small cell lung cancer.[9] With respect to lung cancer, stages I, II, and III determine various sizes of primary tumor and lymph node involvement without distant metastasis and any distant metastasis is automatically stage IV.[9] It is also used in combination with surgery for non-small cell lung cancer and with chemotherapy for small cell lung cancer. Chemotherapy The first line of treatment for small cell lung cancer, which are often spread upon clinical presentation.[9] It is also indicated for patients with more advanced stage of non-small cell lung cancer to improve prognosis, disease control or for palliative care.[5]
Recent Updates and News
| [14] | [15] |
Prevention[edit | edit source]
Smoking cessation[edit | edit source]
The best way to prevent lung cancer is to quit smoking. The risk of getting diagnosed with lung cancer will decrease the sooner an individual quits smoking. After 10 years of not smoking, the chance of developing lung cancer decreases to half that of someone who smokes.[6] Diet Research suggests that eating a low-fat, high-fibre diet, including at least five portions of fresh fruit and vegetables and whole grains every day, can help reduce the risk of developing lung cancer, as well as other types of cancer and heart disease.[16]
Physical Activity/Exercise[edit | edit source]
Studies show that higher levels of physical activity may lower lung cancer risk.[17] It is important to exercise regularly, attempting to perform at least 150 minutes of moderate intensity aerobic activity each week and incorporate muscle strengthening activities two days per week.[16]
Aspirin[edit | edit source]
Some research has found that taking aspirin may reduce the risk of getting lung cancer.[18] Other studies have found that aspirin may only reduce risk in people who take aspirin daily or may only reduce the risk in men.[6] It is important to check with a doctor before taking aspirin every day as it can damage the lining of the stomach and potentially cause bleeding.
References[edit | edit source]
1. Yoder LH. An overview of lung cancer symptoms, pathophysiology, and treatment. Medsurg Nurs. 2006;15(4):231–4.
2. McMaster Pathology Review. Lung Cancer. www.dh.gov.uk/PolicyAndGuidance/fs/en (accessed 22 May 2015).
3. Alberg AJ, Samet JM. Epidemiology of Lung Cancer Epidemiology of Lung Cancer. 2007
4. Cancer Research UK. Lung Cancer Statistics. http://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/lung-cancer (accessed 17 May 2015)
5. Dela Cruz CS, Tanoue LT, Matthay R a. Lung Cancer: epidemiology, etiology and prevention. Clin Chest Med. 2011;32(4):1–61.
6. National Health Services. Lung Cancer Diagnosis. http://www.nhs.uk/Conditions/Cancer-of-the-lung/Pages/Diagnosis.aspx (accessed 26 May 2015)
7. Ozalevli S. Impact of physiotherapy on patients with advanced lung cancer. Chron Respir Dis [Internet]. 2013;10(4):223–32. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24177683
8. National Health Services. Lung Cancer Prevention. http://www.nhs.uk/Conditions/Cancer-of-the-lung/Pages/Prevention.aspx (accessed 6 May 2015)
9. Hanrahan EO, Glisson B. Lung Cancer: [Internet]. Current. 2010. 395-434 p. Available from: http://www.springerlink.com/index/10.1007/978-1-60761-524-8
10. Youtube. Can the Herpes Virus Kill Cancer?. https://www.youtube.com/watch?v=qXxMffXHBnQ (accessed 3 June 2015)
11. Youtube. Cold Sore Virus Could Treat Skin Cancer, Says Scientists. https://www.youtube.com/watch?v=7PHc-dFtNJ0 (accesssed 3 June 2015)
<span style="line-height: 1.5em;" />
- ↑ Radiopedia Lung cancer Available from:https://radiopaedia.org/articles/lung-cancer-3 (last accessed 7.9.2020)
- ↑ World cancer research fund Lung cancer Available from:https://www.wcrf.org/dietandcancer/cancer-trends/lung-cancer-statistics (last accessed 7.9.2020)
- ↑ Siddiqui F, Siddiqui AH. Cancer, lung. InStatPearls [Internet] 2020 Apr 12. StatPearls Publishing.Available from:https://www.ncbi.nlm.nih.gov/books/NBK482357/ (last accessed 7.9.2020)
- ↑ 4.0 4.1 4.2 4.3 Cancer Research UK. Lung Cancer Statistics. http://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/lung-cancer (accessed 17 May 2015)
- ↑ 5.00 5.01 5.02 5.03 5.04 5.05 5.06 5.07 5.08 5.09 5.10 McMaster Pathology Review. Lung Cancer. www.dh.gov.uk/PolicyAndGuidance/fs/en (accessed 22 May 2015).
- ↑ 6.0 6.1 6.2 6.3 6.4 6.5 6.6 6.7 Dela Cruz CS, Tanoue LT, Matthay R a. Lung Cancer: epidemiology, etiology and prevention. Clin Chest Med. 2011;32(4):1–61.
- ↑ 7.0 7.1 7.2 7.3 7.4 7.5 7.6 7.7 National Health Services. Lung Cancer Diagnosis http://www.nhs.uk/Conditions/Cancer-of-the-lung/Pages/Diagnosis.aspx (accessed 26 May 2015)
- ↑ CancerResearchUK. Cancer Stages and Having a PET Scan. Cancer Research UK. Available from: https://www.youtube.com/watch?v=lk-VzATcv4M [last accessed 7/6/15]
- ↑ 9.0 9.1 9.2 9.3 9.4 9.5 Yoder LH. An overview of lung cancer symptoms, pathophysiology, and treatment. Medsurg Nurs. 2006;15(4):231–4.
- ↑ 10.0 10.1 Ozalevli S. Impact of physiotherapy on patients with advanced lung cancer. Chron Respir Dis [Internet]. 2013;10(4):223–32. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24177683
- ↑ Hoffman M, Augusto VM, Eduardo DS, Silveira BM, Lemos MD, Parreira VF. Inspiratory muscle training reduces dyspnea during activities of daily living and improves inspiratory muscle function and quality of life in patients with advanced lung disease. Physiotherapy theory and practice. 2019 Aug 21:1-1.
- ↑ Johnson MJ, Nabb S, Booth S, Kanaan M. Openness Personality Trait Associated With Benefit From a Nonpharmacological Breathlessness Intervention in People With Intrathoracic Cancer: An Exploratory Analysis. Journal of pain and symptom management. 2020 Feb 20.
- ↑ Edbrooke L, Granger CL, Denehy L. Physical activity for people with lung cancer. Australian Journal of General Practice. 2020 Apr;49(4):175.
- ↑ DNews. Can The Herpes Virus Kill Cancer?. Available from: https://www.youtube.com/watch?v=qXxMffXHBnQ [last accessed 7/6/15]
- ↑ VideoUKNewsDaily. Cold sore virus could treat skin cancer, say scientists. Available from: https://www.youtube.com/watch?v=7PHc-dFtNJ0 [last accessed 7/6/15]
- ↑ 16.0 16.1 National Health Services. Lung Cancer Prevention. http://www.nhs.uk/Conditions/Cancer-of-the-lung/Pages/Prevention.aspx (accessed 6 May 2015)
- ↑ Lee IM. Physical activity and cancer prevention--data from epidemiologic studies. Medicine and science in sports and exercise. 2003 Nov;35(11):1823-7.
- ↑ Rothwell PM, Wilson M, Price JF, Belch JF, Meade TW, Mehta Z. Effect of daily aspirin on risk of cancer metastasis: a study of incident cancers during randomised controlled trials. The Lancet. 2012 Apr 28;379(9826):1591-601.