Lower Limb Motor Coordination: Difference between revisions
No edit summary |
Chloe Waller (talk | contribs) (Added pictures) |
||
| (15 intermediate revisions by 4 users not shown) | |||
| Line 4: | Line 4: | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | </div> | ||
== | == Introduction == | ||
Motor coordination, otherwise referred to as dexterity refers to the ability to perform a motor task in an accurate, rapid and controlled manner | Motor [[Coordination Exercises|coordination]], otherwise referred to as dexterity, refers to the ability to perform a motor task in an accurate, rapid and controlled manner<ref>Bernstein, N.A. Dexterity and its development. (1st edition ed.). Mahwah: Lawrence Erlbaum Associates; 1996.</ref>. Coordination is dependent on interactions within feedforward and feedback mechanisms between the central nervous system (CNS), sensory information, body schema and motor control<ref>P. Weiss, and M. Jeannerod. Getting a Grasp on Coordination | ||
= | 01 APR 1998<nowiki/>https://pubmed.ncbi.nlm.nih.gov/11390765/</ref> <ref>R.S Johansson, K.J Cole. [https://www.sciencedirect.com/science/article/abs/pii/095943889290139C Sensory-motor coordination during grasping and manipulating actions]. Current Opinion in Neurobiology, Volume 2, Issue 6. December 1992, Pages 815-823 </ref>. For motor control, sufficient muscle tone, range of movement and strength are required<ref>Donna J. Cech DHS, PT, PCS, Suzanne “Tink” Martin MACT, PT. Posture and Balance. [https://www.elsevier.com/books/functional-movement-development-across-the-life-span/9781416049784 Functional Movement Development Across the Life Span (Third Edition)], 2012</ref>. Within the CNS, the cerebellum is primarily is responsible for coordination<ref>Potvin A.R. Tourtelotte W.W. Quantitative examination of neurologic functions. Boca Raton 1985</ref>. Motor coordination requires temporal and spatial accuracy<ref name=":0">Desrosiers J, Rochette A, Corriveau H. [https://www.archives-pmr.org/article/S0003-9993(04)01386-3/fulltext Validation of a new lower-extremity motor coordination test.] Archives of physical medicine and rehabilitation. 2005 May 1;86(5):993-8.</ref>. | ||
Lower limb motor [[Coordination Exercises|coordination]] is essential for the performance of most daily motor activities, such as walking, running, ascending/descending stairs and standing from a chair. The effective performance of these tasks are critical for an independent life<ref>Carr J, Shepherd R. Reabilitação neurológica: otimizando o desempenho motor. São Paulo: Manole; 2008</ref><ref name=":0" />. Impaired coordination impacts on strength, speed and precision of lower limb movement, thus affecting these functions <ref>John J. Lee. [https://www.sciencedirect.com/science/article/pii/B9780323553810000093 Limb Impairments After Stroke] in Stroke Rehabilitation, 2019</ref>. It is also important for community activities, and it’s limitation may cause people to become housebound and isolated from the society, especially for those who had suffered [[Stroke: Physiotherapy Treatment Approaches|stroke]]<ref>Gao KL, Ng SS, Kwok JW, Chow RT, Tsang WW. [https://europepmc.org/article/med/20461340 Eye–hand coordination and its relationship with sensori-motor impairments in stroke survivors]. Journal of Rehabilitation Medicine. 2010 Apr 1;42(4):368-73.</ref>. Motor tasks performed within different contexts require between-limb coordination, which is essential for an independent and safe life, especially in elderly individuals<ref>Capranica L, Tessitore A, Olivieri B, Minganti C, Pesce C. [https://www.researchgate.net/publication/8237848_Field_Evaluation_of_Cycled_Coupled_Movements_of_Hand_and_Foot_in_Older_Individuals Field evaluation of cycled coupled movements of hand and foot in older individuals.] Gerontology. 2004;50(6):399-406.</ref>. Lower limb joint coordination changes with age, increasing the risk of [[falls]] in the elderly population<ref>P.Ippersiel, S.M. Robbins, P.C. Dixon Lower-limb coordination and variability during gait: The effects of age and walking surface. Gait and Posture, Volume 85, March 2021</ref>. Adequate lower limb motor coordination significantly contributes to functionality of stroke individuals, its loss is the major contributor to disability in this population<ref name=":1">de Menezes KK, Scianni AA, Faria-Fortini I, Avelino PR, Faria CD, Teixeira-Salmela LF. [https://www.iomcworld.org/open-access/lower-limb-motor-coordination-of-stroke-survivors-based-upon-theirlevels-of-motor-recovery-and-ages-2155-9562-1000338.pdf Lower limb motor coordination of stroke survivors, based upon their levels of motor recovery and ages.] Journal of Neurology & Neurophysiology. 2015;6(6):1-3.</ref> <ref name=":2">Menezes KP, Nascimento LR, Pinheiro MB, Scianni AA, Faria CD, Avelino P, Faria-Fortini I, Teixeira-Salmela LF. [https://europepmc.org/article/med/28352935 Lower limb motor coordination is significantly impaired in ambulatory people with chronic stroke: a cross-sectional study]. Journal of Rehabilitation Medicine. 2017 Apr 1;49:322-6.</ref><ref name=":3">Menezes KK, Nascimento LR, Faria CD, Avelino PR, Scianni AA, Polese JC, Faria-Fortini I, Teixeira-Salmela LF. [https://europepmc.org/article/med/29927672 Deficits in motor coordination of the paretic lower limb best explained activity limitations after stroke]. Physiotherapy theory and practice. 2020 Mar 3;36(3):417-23.</ref>. Thus, therapeutic approaches aimed at restoring lower limb motor coordination are of great interest for rehabilitation professionals who are involved in research and clinical settings<ref>Ada, L, Canning, C. Changing the way we view the contribution of motor impairments to physical disability after stroke. In: Refshauge, K, Ada, L, Ellis E (2005) editors. Science-based rehabilitation: theories into practice. Sydney: Elsevier; 87–106.</ref>. | |||
== Medical conditions that may exhibit deficits in lower limb motor coordination == | |||
* [[Schizophrenia]] or other psychiatric disorders <ref name=":4">Krebs MO, Gut-Fayand A, Bourdel MC, Dischamp J, Olié JP. [https://pubmed.ncbi.nlm.nih.gov/11042442/ Validation and factorial structure of a standardized neurological examination assessing neurological soft signs in schizophrenia.] Schizophrenia Research. 2000 Oct 27;45(3):245-60.</ref> | |||
* [https://www.physio-pedia.com/Overview_of_spinal_cord_injuries Spinal cord injuries]<ref name=":5">Wirth B, van Hedel H, Curt A. [https://www.researchgate.net/publication/5465821_Foot_control_in_incomplete_SCI_Distinction_between_paresis_and_dexterity Foot control in incomplete SCI: distinction between paresis and dexterity.] Neurological research. 2008 Feb 1;30(1):52-60.</ref> | |||
* [[Ataxia]]<ref name=":6">Braga-Neto P, Godeiro-Junior C, Dutra LA, Pedroso JL, Barsottini OG. [https://pubmed.ncbi.nlm.nih.gov/20464290/ Translation and validation into Brazilian version of the Scale of the Assessment and Rating of Ataxia (SARA)]. Arquivos de neuro-psiquiatria. 2010 Apr;68(2):228-30.</ref> <ref name=":7">Schmitz-Hübsch T, Du Montcel ST, Baliko L, Berciano J, Boesch S, Depondt C, Giunti P, Globas C, Infante J, Kang JS, Kremer B. [https://pubmed.ncbi.nlm.nih.gov/16769946/ Scale for the assessment and rating of ataxia: development of a new clinical scale]. Neurology. 2006 Jun 13;66(11):1717-20.</ref> | |||
* [[Stroke]]<ref name=":0" /> <ref name=":1" /> <ref name=":2" /> <ref name=":3" /> <ref name=":8">Maki T, Quagliato EM, Cacho EW, Paz LP, Nascimento NH, Inoue MM, Viana MA. [https://www.scielo.br/scielo.php?script=sci_arttext&pid=S1413-35552006000200007&lng=pt&nrm=iso&tlng=pt Reliability study on the application of the Fugl-Meyer scale in Brazil]. Revista Brasileira Fisioterapia. 2006;10(2):177-83.</ref> <ref name=":9">Dittiger M, Bohannon RW, Andrews AW. [https://www.jstage.jst.go.jp/article/jpts/13/2/13_2_75/_pdf Reliability, responsiveness, and validity of timed, large amplitude, rapid alternating movement patterns among patients with stroke]. Journal of Physical Therapy Science. 2001;13(2):75-81.</ref> | |||
= | * [https://www.physio-pedia.com/Parkinson%27s Parkinson disease]<ref name=":10">Gunzler SA, Pavel M, Koudelka C, Carlson NE, Nutt JG. [https://europepmc.org/article/med/18978495 Foot-tapping rate as an objective outcome measure for Parkinson disease clinical trials]. Clinical Neuropharmacology. 2009 Mar 1;32(2):97-102.</ref> | ||
Lower limb motor coordination evaluation is very important for a physical therapist practice, as it enables the understanding of the nature and level of impairments of the individual in a standardized way ( | == Assessment of lower limb motor coordination == | ||
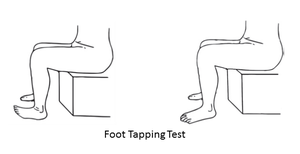
[[File:Foot tapping.png|thumb|Foot tapping test (FTT)]] | |||
Lower limb motor coordination evaluation is very important for a physical therapist practice, as it enables the understanding of the nature and level of impairments of the individual in a standardized way<ref>Cavaco NS, Alouche SR. [https://www.scielo.br/scielo.php?script=sci_arttext&pid=S1809-29502010000200015 Instrumentos de avaliação da função de membros superiores após acidente vascular encefálico: uma revisão sistemática]. Fisioterapia e Pesquisa. 2010 Jun;17(2):178-83.</ref> <ref>Soriano FF, Baraldi K. [https://periodicos.uninove.br/index.php?journal=saude&page=article&op=view&path%5B%5D=2227&path%5B%5D=1768 Escalas de avaliação funcional aplicáveis a pacientes pós acidente vascular encefálico.] ConScientiae Saúde. 2010;9(3):521-30.</ref>. The information gathered from the assessment tools may help planning the interventions and monitoring the clinical status of the patients before, during, and after physical therapy interventions<ref>Lima RC. [https://repositorio.ufmg.br/bitstream/1843/MSMR-6XLGKL/1/disserta__o_renata_cristina_magalh_es_lima.pdf Adaptação transcultural do Stroke Specific Quality of Life SSQOL: um instrumento específico para avaliar a qualidade de vida de hemiplégicos. [dissertação].] Belo Horizonte: Universidade Federal de Minas Gerais; 2006.</ref> <ref>Gadotti IC, Vieira ER, Magee DJ. [https://www.scielo.br/scielo.php?script=sci_arttext&pid=S1413-35552006000200002 Importance and clarification of measurement properties in rehabilitation.] Brazilian Journal of Physical Therapy. 2006;10(2):137-46.</ref>. | |||
* Auditory-paced ankle dorsi and plantarflexion task<ref name=":5" /> | |||
[[File:Lower Extremity Motor Coordination Test.png|thumb|Lower Extremity Motor Coordination Test (LEMOCOT)]] | |||
* [https://www.physio-pedia.com/Fugl-Meyer_Assessment_of_Motor_Recovery_after_Stroke Fugl Meyer Scale]<ref name=":8" /> | |||
* Rapid alternating movement patterns test (RAMP)<ref name=":9" /> | |||
* [[Scale for the Assessment and Rating of Ataxia (SARA)]]<ref name=":6" /> <ref name=":7" /> | |||
* [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3339227/ Standardized Neurological Examination in Schizophrenia (NSS)]<ref name=":4" /> | |||
* [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6698509/ Foot tapping test (FTT)]<ref name=":10" /> | |||
[[File:Heel - shin.jpg|thumb|Heel-Shin test]] | |||
* [https://www.archives-pmr.org/article/S0003-9993(04)01386-3/pdf Lower Extremity Motor Coordination Test (LEMOCOT)]<ref name=":0" /><ref>Handelzalts S, Koren Y, Goldhamer N, Yeshurun-Tayer A, Parmet Y, Shmuelof L, et al. Insights into motor performance deficits after stroke: an automated and refined analysis of the lower-extremity motor coordination test (LEMOCOT). J Neuroeng Rehabil [Internet]. 2021 [cited 2022 Apr 17];18(1):155. Available from: https://pubmed.ncbi.nlm.nih.gov/34702299/</ref> | |||
* [https://pubmed.ncbi.nlm.nih.gov/33410389/ Comprehensive Coordination Scale]<ref>Molad R, Alouche SR, Demers M, Levin MF. Development of a comprehensive outcome measure for motor coordination, step 2: Reliability and construct validity in chronic stroke patients. Neurorehabil Neural Repair [Internet]. 2021 [cited 2022 Apr 17];35(2):194–203. Available from: https://pubmed.ncbi.nlm.nih.gov/33410389/</ref> | |||
* Heel-Shin Test<ref>Krishna R, Pathirana PN, Horne M, Power L, Szmulewicz DJ. Quantitative assessment of cerebellar ataxia, through automated limb functional tests. J Neuroeng Rehabil [Internet]. 2019 [cited 2022 Apr 17];16(1):31. Available from: https://pubmed.ncbi.nlm.nih.gov/30813963</ref> | |||
== Resources == | |||
*Pinheiro M, Scianni A, Ada L, Faria C, Teixeira-Salmela L. [https://pubmed.ncbi.nlm.nih.gov/24681388/ Reference Values and Psychometric Properties of the Lower Extremity Motor Coordination Test]. Archives of Physical Medicine and Rehabilitation. 2014;95(8):1490-1497. | |||
== | |||
*Pinheiro M, Scianni A, Ada L, Faria C, Teixeira-Salmela L. Reference Values and Psychometric Properties of the Lower Extremity Motor Coordination Test. Archives of Physical Medicine and Rehabilitation. 2014;95(8):1490-1497 | |||
== References == | |||
<references /> | <references /> | ||
Latest revision as of 07:38, 19 April 2022
Original Editor - Joseph Olamide
Top Contributors - Joseph Olamide, Chloe Waller, Kim Jackson and Leana Louw
Introduction[edit | edit source]
Motor coordination, otherwise referred to as dexterity, refers to the ability to perform a motor task in an accurate, rapid and controlled manner[1]. Coordination is dependent on interactions within feedforward and feedback mechanisms between the central nervous system (CNS), sensory information, body schema and motor control[2] [3]. For motor control, sufficient muscle tone, range of movement and strength are required[4]. Within the CNS, the cerebellum is primarily is responsible for coordination[5]. Motor coordination requires temporal and spatial accuracy[6].
Lower limb motor coordination is essential for the performance of most daily motor activities, such as walking, running, ascending/descending stairs and standing from a chair. The effective performance of these tasks are critical for an independent life[7][6]. Impaired coordination impacts on strength, speed and precision of lower limb movement, thus affecting these functions [8]. It is also important for community activities, and it’s limitation may cause people to become housebound and isolated from the society, especially for those who had suffered stroke[9]. Motor tasks performed within different contexts require between-limb coordination, which is essential for an independent and safe life, especially in elderly individuals[10]. Lower limb joint coordination changes with age, increasing the risk of falls in the elderly population[11]. Adequate lower limb motor coordination significantly contributes to functionality of stroke individuals, its loss is the major contributor to disability in this population[12] [13][14]. Thus, therapeutic approaches aimed at restoring lower limb motor coordination are of great interest for rehabilitation professionals who are involved in research and clinical settings[15].
Medical conditions that may exhibit deficits in lower limb motor coordination[edit | edit source]
- Schizophrenia or other psychiatric disorders [16]
Assessment of lower limb motor coordination[edit | edit source]
Lower limb motor coordination evaluation is very important for a physical therapist practice, as it enables the understanding of the nature and level of impairments of the individual in a standardized way[23] [24]. The information gathered from the assessment tools may help planning the interventions and monitoring the clinical status of the patients before, during, and after physical therapy interventions[25] [26].
- Auditory-paced ankle dorsi and plantarflexion task[17]
- Rapid alternating movement patterns test (RAMP)[21]
- Lower Extremity Motor Coordination Test (LEMOCOT)[6][27]
- Comprehensive Coordination Scale[28]
- Heel-Shin Test[29]
Resources[edit | edit source]
- Pinheiro M, Scianni A, Ada L, Faria C, Teixeira-Salmela L. Reference Values and Psychometric Properties of the Lower Extremity Motor Coordination Test. Archives of Physical Medicine and Rehabilitation. 2014;95(8):1490-1497.
References[edit | edit source]
- ↑ Bernstein, N.A. Dexterity and its development. (1st edition ed.). Mahwah: Lawrence Erlbaum Associates; 1996.
- ↑ P. Weiss, and M. Jeannerod. Getting a Grasp on Coordination 01 APR 1998https://pubmed.ncbi.nlm.nih.gov/11390765/
- ↑ R.S Johansson, K.J Cole. Sensory-motor coordination during grasping and manipulating actions. Current Opinion in Neurobiology, Volume 2, Issue 6. December 1992, Pages 815-823
- ↑ Donna J. Cech DHS, PT, PCS, Suzanne “Tink” Martin MACT, PT. Posture and Balance. Functional Movement Development Across the Life Span (Third Edition), 2012
- ↑ Potvin A.R. Tourtelotte W.W. Quantitative examination of neurologic functions. Boca Raton 1985
- ↑ 6.0 6.1 6.2 6.3 Desrosiers J, Rochette A, Corriveau H. Validation of a new lower-extremity motor coordination test. Archives of physical medicine and rehabilitation. 2005 May 1;86(5):993-8.
- ↑ Carr J, Shepherd R. Reabilitação neurológica: otimizando o desempenho motor. São Paulo: Manole; 2008
- ↑ John J. Lee. Limb Impairments After Stroke in Stroke Rehabilitation, 2019
- ↑ Gao KL, Ng SS, Kwok JW, Chow RT, Tsang WW. Eye–hand coordination and its relationship with sensori-motor impairments in stroke survivors. Journal of Rehabilitation Medicine. 2010 Apr 1;42(4):368-73.
- ↑ Capranica L, Tessitore A, Olivieri B, Minganti C, Pesce C. Field evaluation of cycled coupled movements of hand and foot in older individuals. Gerontology. 2004;50(6):399-406.
- ↑ P.Ippersiel, S.M. Robbins, P.C. Dixon Lower-limb coordination and variability during gait: The effects of age and walking surface. Gait and Posture, Volume 85, March 2021
- ↑ 12.0 12.1 de Menezes KK, Scianni AA, Faria-Fortini I, Avelino PR, Faria CD, Teixeira-Salmela LF. Lower limb motor coordination of stroke survivors, based upon their levels of motor recovery and ages. Journal of Neurology & Neurophysiology. 2015;6(6):1-3.
- ↑ 13.0 13.1 Menezes KP, Nascimento LR, Pinheiro MB, Scianni AA, Faria CD, Avelino P, Faria-Fortini I, Teixeira-Salmela LF. Lower limb motor coordination is significantly impaired in ambulatory people with chronic stroke: a cross-sectional study. Journal of Rehabilitation Medicine. 2017 Apr 1;49:322-6.
- ↑ 14.0 14.1 Menezes KK, Nascimento LR, Faria CD, Avelino PR, Scianni AA, Polese JC, Faria-Fortini I, Teixeira-Salmela LF. Deficits in motor coordination of the paretic lower limb best explained activity limitations after stroke. Physiotherapy theory and practice. 2020 Mar 3;36(3):417-23.
- ↑ Ada, L, Canning, C. Changing the way we view the contribution of motor impairments to physical disability after stroke. In: Refshauge, K, Ada, L, Ellis E (2005) editors. Science-based rehabilitation: theories into practice. Sydney: Elsevier; 87–106.
- ↑ 16.0 16.1 Krebs MO, Gut-Fayand A, Bourdel MC, Dischamp J, Olié JP. Validation and factorial structure of a standardized neurological examination assessing neurological soft signs in schizophrenia. Schizophrenia Research. 2000 Oct 27;45(3):245-60.
- ↑ 17.0 17.1 Wirth B, van Hedel H, Curt A. Foot control in incomplete SCI: distinction between paresis and dexterity. Neurological research. 2008 Feb 1;30(1):52-60.
- ↑ 18.0 18.1 Braga-Neto P, Godeiro-Junior C, Dutra LA, Pedroso JL, Barsottini OG. Translation and validation into Brazilian version of the Scale of the Assessment and Rating of Ataxia (SARA). Arquivos de neuro-psiquiatria. 2010 Apr;68(2):228-30.
- ↑ 19.0 19.1 Schmitz-Hübsch T, Du Montcel ST, Baliko L, Berciano J, Boesch S, Depondt C, Giunti P, Globas C, Infante J, Kang JS, Kremer B. Scale for the assessment and rating of ataxia: development of a new clinical scale. Neurology. 2006 Jun 13;66(11):1717-20.
- ↑ 20.0 20.1 Maki T, Quagliato EM, Cacho EW, Paz LP, Nascimento NH, Inoue MM, Viana MA. Reliability study on the application of the Fugl-Meyer scale in Brazil. Revista Brasileira Fisioterapia. 2006;10(2):177-83.
- ↑ 21.0 21.1 Dittiger M, Bohannon RW, Andrews AW. Reliability, responsiveness, and validity of timed, large amplitude, rapid alternating movement patterns among patients with stroke. Journal of Physical Therapy Science. 2001;13(2):75-81.
- ↑ 22.0 22.1 Gunzler SA, Pavel M, Koudelka C, Carlson NE, Nutt JG. Foot-tapping rate as an objective outcome measure for Parkinson disease clinical trials. Clinical Neuropharmacology. 2009 Mar 1;32(2):97-102.
- ↑ Cavaco NS, Alouche SR. Instrumentos de avaliação da função de membros superiores após acidente vascular encefálico: uma revisão sistemática. Fisioterapia e Pesquisa. 2010 Jun;17(2):178-83.
- ↑ Soriano FF, Baraldi K. Escalas de avaliação funcional aplicáveis a pacientes pós acidente vascular encefálico. ConScientiae Saúde. 2010;9(3):521-30.
- ↑ Lima RC. Adaptação transcultural do Stroke Specific Quality of Life SSQOL: um instrumento específico para avaliar a qualidade de vida de hemiplégicos. [dissertação.] Belo Horizonte: Universidade Federal de Minas Gerais; 2006.
- ↑ Gadotti IC, Vieira ER, Magee DJ. Importance and clarification of measurement properties in rehabilitation. Brazilian Journal of Physical Therapy. 2006;10(2):137-46.
- ↑ Handelzalts S, Koren Y, Goldhamer N, Yeshurun-Tayer A, Parmet Y, Shmuelof L, et al. Insights into motor performance deficits after stroke: an automated and refined analysis of the lower-extremity motor coordination test (LEMOCOT). J Neuroeng Rehabil [Internet]. 2021 [cited 2022 Apr 17];18(1):155. Available from: https://pubmed.ncbi.nlm.nih.gov/34702299/
- ↑ Molad R, Alouche SR, Demers M, Levin MF. Development of a comprehensive outcome measure for motor coordination, step 2: Reliability and construct validity in chronic stroke patients. Neurorehabil Neural Repair [Internet]. 2021 [cited 2022 Apr 17];35(2):194–203. Available from: https://pubmed.ncbi.nlm.nih.gov/33410389/
- ↑ Krishna R, Pathirana PN, Horne M, Power L, Szmulewicz DJ. Quantitative assessment of cerebellar ataxia, through automated limb functional tests. J Neuroeng Rehabil [Internet]. 2019 [cited 2022 Apr 17];16(1):31. Available from: https://pubmed.ncbi.nlm.nih.gov/30813963