Lower Extremity Motor Coordination Test (LEMOCOT): Difference between revisions
Kapil Narale (talk | contribs) No edit summary |
Kapil Narale (talk | contribs) No edit summary |
||
| Line 14: | Line 14: | ||
There are a few possible ways to determine the LEMOCOT score, as illustrated by different researchers. | There are a few possible ways to determine the LEMOCOT score, as illustrated by different researchers. | ||
Yildrin et al ( ) took the highest score from three trials of the LEMOCOT post-operatively, while Desrosiers et al ( ) took the mean of two trials of stroke patients. <ref name=":0" /> | Yildrin et al ( ) took the highest score from three trials of the LEMOCOT post-operatively, while Desrosiers et al ( ) took the mean of two trials of stroke patients. <ref name=":0" /> | ||
The various scoring methods were not clinically significant, but did show test-retest reliability, which indicates that any method could be used. It is noted hat the average of a greater number of trials can reduce errors in overall scoring. | |||
However, when compared to healthy individuals, only one trial was needed for reliable values. <ref name=":0" /> | However, when compared to healthy individuals, only one trial was needed for reliable values. <ref name=":0" /> | ||
| Line 22: | Line 24: | ||
Deficits in motor coordination after stroke are seen to depend on the level of functional and motor recovery, and the time elapsed since the stroke incident. Therefore, the level of deficit should be assessed at different stages of the stroke rehabilitation. The LEMOCOT should detect differences between the paretic and non-paretic sides as well. | Deficits in motor coordination after stroke are seen to depend on the level of functional and motor recovery, and the time elapsed since the stroke incident. Therefore, the level of deficit should be assessed at different stages of the stroke rehabilitation. The LEMOCOT should detect differences between the paretic and non-paretic sides as well. | ||
It is seen that major differences, between healthy and impaired individuals, were only noticed when comparing the performance of the paretic limb, where as the performance of the non-paretic limb did not have a significant difference in the scoring. The mean score of the paretic limb represented 51% of the outcome of the non-dominant limb for healthy individuals. | |||
== Validity and Reliability: == | == Validity and Reliability: == | ||
Revision as of 02:48, 20 December 2022
Introduction:[edit | edit source]
Lower Extremity Motor Coordination Test was developed as an easy, yet effective tool to clinically assess, measure, and evaluate the deficits in Lower Limb Motor Coordination [1] in conditions such as stroke, spinal cord injuries, ataxia, Parkinson’s disease, schizophrenia or other psychiatric illnesses.
The standard reference values were determined using healthy individuals, categorizing them into age and gender. [1]
It is able to detect motor coordination disturbances after stroke. It also gives a strong indicator of participation capabilities. [1]
It is interesting to note that LEMOCOT scores differentiated between stroke patients who were discharged to long-term care compared to other types of living environments. [1]
Technique:[edit | edit source]
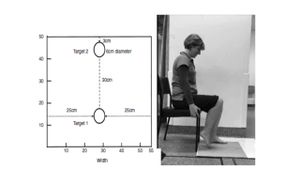
The patient, in a comfortable sitting position, with heels on the proximal target and with the knees at 90° of flexion, is instructed to alternately move his/her lower limb as quickly as possible and touch with the hallux two red targets with 6 cm in diameter (one proximal and one distal), separated by a distance of 30 cm for 20 seconds. An additional instruction is given not to sacrifice the accuracy of the touches nor the quality of the movement to increase speed. A familiarization trial is conducted first before the examiner counts the number of touched targets.[1][2]
Obtaining the LEMOCOT Score[edit | edit source]
There are a few possible ways to determine the LEMOCOT score, as illustrated by different researchers.
Yildrin et al ( ) took the highest score from three trials of the LEMOCOT post-operatively, while Desrosiers et al ( ) took the mean of two trials of stroke patients. [1]
The various scoring methods were not clinically significant, but did show test-retest reliability, which indicates that any method could be used. It is noted hat the average of a greater number of trials can reduce errors in overall scoring.
However, when compared to healthy individuals, only one trial was needed for reliable values. [1]
Applicability to Stroke[edit | edit source]
Prior to using the LEMOCOT with stroke patients, certain measurement properties need to be in place.
Deficits in motor coordination after stroke are seen to depend on the level of functional and motor recovery, and the time elapsed since the stroke incident. Therefore, the level of deficit should be assessed at different stages of the stroke rehabilitation. The LEMOCOT should detect differences between the paretic and non-paretic sides as well.
It is seen that major differences, between healthy and impaired individuals, were only noticed when comparing the performance of the paretic limb, where as the performance of the non-paretic limb did not have a significant difference in the scoring. The mean score of the paretic limb represented 51% of the outcome of the non-dominant limb for healthy individuals.
Validity and Reliability:[edit | edit source]
The convergent construct validity was shown by significantly high correlations with physical and functional tests. Construct validity can be evaluated by comparing outcomes of groups differing in some characteristics or abilities.
and the divergent validity was shown by a reduced association with cognitive or visual perceptual tests.
Evidence:[edit | edit source]
Test-retest reliability in stroke population[edit | edit source]
Intraclass correlation (ICC) >0.97
Construct validity p<0.0001
ICC values (dominant and non-dominant limbs) 0.90<ICC<0.99[1]
Validity and Reliability in Autosomal recessive spastic ataxia of Charlevoix-Saguenay (ARSACS) population[edit | edit source]
ICC 0.92 - 0.97[4]
Normative Values for LEMOCOT[5]
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 de Menezes KK, Scianni AA, Faria-Fortini I, Avelino PR, Faria CD, Teixeira-Salmela LF. Measurement properties of the lower extremity motor coordination test in individuals with stroke. Journal of Rehabilitation Medicine. 2015 Jun 5;47(6):502-7.
- ↑ Menezes KP, Nascimento LR, Pinheiro MB, Scianni AA, Faria CD, Avelino P, Faria-Fortini I, Teixeira-Salmela LF. Lower limb motor coordination is significantly impaired in ambulatory people with chronic stroke: a cross-sectional study. J Rehabil Med. 2017 Apr 1;49:322-6.
- ↑ Kwan MS, Hassett LM, Ada L, Canning CG. Relationship between lower limb coordination and walking speed after stroke: an observational study. Brazilian journal of physical therapy. 2019 Nov 1;23(6):527-31.
- ↑ Lessard I, Lavoie C, Côté I, Mathieu J, Brais B, Gagnon C. Validity and reliability of the LEMOCOT in the adult ARSACS population: a measure of lower limb coordination. Journal of the Neurological Sciences. 2017 Jun 15;377:193-6.
- ↑ Pinheiro MB, Scianni AA, Ada L, Faria CD, Teixeira-Salmela LF. Reference values and psychometric properties of the lower extremity motor coordination test. Archives of physical medicine and rehabilitation. 2014 Aug 1;95(8):1490-7.