Lower Extremity Motor Coordination Test (LEMOCOT): Difference between revisions
Kim Jackson (talk | contribs) m (Updated page link) |
Kapil Narale (talk | contribs) No edit summary |
||
| Line 1: | Line 1: | ||
== | == Introduction: == | ||
Lower Extremity Motor Coordination Test was developed as an easy, yet effective tool to clinically assess and evaluate the deficits in [[Lower Limb Motor Coordination]] in conditions such as [[stroke]], [[Spinal Cord Injury|spinal cord injuries]], [[ataxia]], [[Parkinson's - Clinical Presentation|Parkinson’s disease]], [[schizophrenia]] or other psychiatric illnesses. | Lower Extremity Motor Coordination Test was developed as an easy, yet effective tool to clinically assess, measure, and evaluate the deficits in [[Lower Limb Motor Coordination]] <ref name=":0" /> in conditions such as [[stroke]], [[Spinal Cord Injury|spinal cord injuries]], [[ataxia]], [[Parkinson's - Clinical Presentation|Parkinson’s disease]], [[schizophrenia]] or other psychiatric illnesses. | ||
The standard reference values were determined using healthy individuals, categorizing them into age and gender. <ref name=":0" /> | |||
It is able to detect motor coordination disturbances after stroke. It also gives a strong indicator of participation capabilities. <ref name=":0" /> | |||
It is interesting to note that LEMOCOT scores differentiated between stroke patients who were discharged to long-term care compared to other types of living environments. <ref name=":0" /> | |||
== Technique: == | == Technique: == | ||
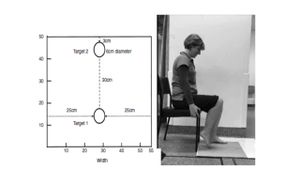
The patient, in a comfortable sitting position, with heels on the proximal target and with the knees at 90° of flexion, is instructed to alternately move his/her lower limb as quickly as possible and touch with the hallux two red targets with 6 cm in diameter (one proximal and one distal), separated by a distance of 30 cm for 20 seconds. An additional instruction is given not to sacrifice the accuracy of the touches nor the quality of the movement to increase speed. A familiarization trial is conducted first before the examiner counts the number of touched targets.<ref name=":0">de Menezes KK, Scianni AA, Faria-Fortini I, Avelino PR, Faria CD, Teixeira-Salmela LF. [https://pubmed.ncbi.nlm.nih.gov/25882758/ Measurement properties of the lower extremity motor coordination test in individuals with stroke]. Journal of Rehabilitation Medicine. 2015 Jun 5;47(6):502-7.</ref><ref>Menezes KP, Nascimento LR, Pinheiro MB, Scianni AA, Faria CD, Avelino P, Faria-Fortini I, Teixeira-Salmela LF. [https://pubmed.ncbi.nlm.nih.gov/28352935/ Lower limb motor coordination is significantly impaired in ambulatory people with chronic stroke: a cross-sectional study.] J Rehabil Med. 2017 Apr 1;49:322-6.</ref> | The patient, in a comfortable sitting position, with heels on the proximal target and with the knees at 90° of flexion, is instructed to alternately move his/her lower limb as quickly as possible and touch with the hallux two red targets with 6 cm in diameter (one proximal and one distal), separated by a distance of 30 cm for 20 seconds. An additional instruction is given not to sacrifice the accuracy of the touches nor the quality of the movement to increase speed. A familiarization trial is conducted first before the examiner counts the number of touched targets.<ref name=":0">de Menezes KK, Scianni AA, Faria-Fortini I, Avelino PR, Faria CD, Teixeira-Salmela LF. [https://pubmed.ncbi.nlm.nih.gov/25882758/ Measurement properties of the lower extremity motor coordination test in individuals with stroke]. Journal of Rehabilitation Medicine. 2015 Jun 5;47(6):502-7.</ref><ref>Menezes KP, Nascimento LR, Pinheiro MB, Scianni AA, Faria CD, Avelino P, Faria-Fortini I, Teixeira-Salmela LF. [https://pubmed.ncbi.nlm.nih.gov/28352935/ Lower limb motor coordination is significantly impaired in ambulatory people with chronic stroke: a cross-sectional study.] J Rehabil Med. 2017 Apr 1;49:322-6.</ref> | ||
==== Obtaining the LEMOCOT Score ==== | |||
There are a few possible ways to determine the LEMOCOT score, as illustrated by different researchers. | |||
== Validity and Reliability: == | |||
The convergent construct validity was shown by significantly high correlations with physical and functional tests, and the divergent validity was shown by a reduced association with cognitive or visual perceptual tests. | |||
== Evidence: == | == Evidence: == | ||
[[File:Setup of LEMOCOT.jpeg|thumb|Setup of Lower Extremity Motor Coordination LEMOCOT<ref>Kwan MS, Hassett LM, Ada L, Canning CG. [https://pubmed.ncbi.nlm.nih.gov/31708057/ Relationship between lower limb coordination and walking speed after stroke: an observational study.] Brazilian journal of physical therapy. 2019 Nov 1;23(6):527-31.</ref>]] | |||
===== Test-retest reliability in stroke population ===== | ===== Test-retest reliability in stroke population ===== | ||
| Line 15: | Line 27: | ||
ICC values (dominant and non-dominant limbs) 0.90<ICC<0.99<ref name=":0" /> | ICC values (dominant and non-dominant limbs) 0.90<ICC<0.99<ref name=":0" /> | ||
===== Validity and Reliability in | ===== Validity and Reliability in Autosomal recessive spastic ataxia of Charlevoix-Saguenay (ARSACS) population ===== | ||
ICC 0.92 - 0.97<ref>Lessard I, Lavoie C, Côté I, Mathieu J, Brais B, Gagnon C. [https://pubmed.ncbi.nlm.nih.gov/28477695/ Validity and reliability of the LEMOCOT in the adult ARSACS population: a measure of lower limb coordination.] Journal of the Neurological Sciences. 2017 Jun 15;377:193-6.</ref> | ICC 0.92 - 0.97<ref>Lessard I, Lavoie C, Côté I, Mathieu J, Brais B, Gagnon C. [https://pubmed.ncbi.nlm.nih.gov/28477695/ Validity and reliability of the LEMOCOT in the adult ARSACS population: a measure of lower limb coordination.] Journal of the Neurological Sciences. 2017 Jun 15;377:193-6.</ref> | ||
Revision as of 05:36, 19 December 2022
Introduction:[edit | edit source]
Lower Extremity Motor Coordination Test was developed as an easy, yet effective tool to clinically assess, measure, and evaluate the deficits in Lower Limb Motor Coordination [1] in conditions such as stroke, spinal cord injuries, ataxia, Parkinson’s disease, schizophrenia or other psychiatric illnesses.
The standard reference values were determined using healthy individuals, categorizing them into age and gender. [1]
It is able to detect motor coordination disturbances after stroke. It also gives a strong indicator of participation capabilities. [1]
It is interesting to note that LEMOCOT scores differentiated between stroke patients who were discharged to long-term care compared to other types of living environments. [1]
Technique:[edit | edit source]
The patient, in a comfortable sitting position, with heels on the proximal target and with the knees at 90° of flexion, is instructed to alternately move his/her lower limb as quickly as possible and touch with the hallux two red targets with 6 cm in diameter (one proximal and one distal), separated by a distance of 30 cm for 20 seconds. An additional instruction is given not to sacrifice the accuracy of the touches nor the quality of the movement to increase speed. A familiarization trial is conducted first before the examiner counts the number of touched targets.[1][2]
Obtaining the LEMOCOT Score[edit | edit source]
There are a few possible ways to determine the LEMOCOT score, as illustrated by different researchers.
Validity and Reliability:[edit | edit source]
The convergent construct validity was shown by significantly high correlations with physical and functional tests, and the divergent validity was shown by a reduced association with cognitive or visual perceptual tests.
Evidence:[edit | edit source]
Test-retest reliability in stroke population[edit | edit source]
Intraclass correlation (ICC) >0.97
Construct validity p<0.0001
ICC values (dominant and non-dominant limbs) 0.90<ICC<0.99[1]
Validity and Reliability in Autosomal recessive spastic ataxia of Charlevoix-Saguenay (ARSACS) population[edit | edit source]
ICC 0.92 - 0.97[4]
Normative Values for LEMOCOT[5]
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 de Menezes KK, Scianni AA, Faria-Fortini I, Avelino PR, Faria CD, Teixeira-Salmela LF. Measurement properties of the lower extremity motor coordination test in individuals with stroke. Journal of Rehabilitation Medicine. 2015 Jun 5;47(6):502-7.
- ↑ Menezes KP, Nascimento LR, Pinheiro MB, Scianni AA, Faria CD, Avelino P, Faria-Fortini I, Teixeira-Salmela LF. Lower limb motor coordination is significantly impaired in ambulatory people with chronic stroke: a cross-sectional study. J Rehabil Med. 2017 Apr 1;49:322-6.
- ↑ Kwan MS, Hassett LM, Ada L, Canning CG. Relationship between lower limb coordination and walking speed after stroke: an observational study. Brazilian journal of physical therapy. 2019 Nov 1;23(6):527-31.
- ↑ Lessard I, Lavoie C, Côté I, Mathieu J, Brais B, Gagnon C. Validity and reliability of the LEMOCOT in the adult ARSACS population: a measure of lower limb coordination. Journal of the Neurological Sciences. 2017 Jun 15;377:193-6.
- ↑ Pinheiro MB, Scianni AA, Ada L, Faria CD, Teixeira-Salmela LF. Reference values and psychometric properties of the lower extremity motor coordination test. Archives of physical medicine and rehabilitation. 2014 Aug 1;95(8):1490-7.