Introduction to Gait Rehabilitation in Spinal Cord Injury
Original Editor -Ewa Jaraczewska based on the course by Maha Tayseer Mohammad
Top Contributors - Ewa Jaraczewska, Jess Bell and Kim Jackson
Introduction[edit | edit source]
Regaining walking function is a goal for many individuals with spinal cord injury and it is a target of various rehabilitative approaches. It is, however, essential to understand the "natural course of walking recovery"[1] in individuals with spinal cord injury (SCI), as well as prognostic factors that influence walking recovery when establishing goals and selecting interventions.[1] This article discusses two approaches to gait rehabilitation, the plasticity-based approach and the compensatory-based approach. It also explores factors that help predict ambulation recovery for patients with a spinal cord injury.
Plasticity-Based Approach[edit | edit source]
The plasticity-based approach to gait rehabilitation in spinal cord injury arises from activity-dependent neural adaptation and training research. Afferent input influences the activity-dependent plasticity of the spinal cord, which affects the neurobiological control of walking.[2]
Early research:
- Sherrington[3] proposed that "proprioceptors responding to hip extension are important for initiating swing"[4]
- Grillner and Rossignol[5] found that preventing hip extension in chronic spinal cats "inhibited the generation of the flexor burst and thus the onset of the swing phase"[4]
- Hiebert et al.[6] found that vibration of iliopsoas during stance resulted in an "earlier onset of swing in walking decerebrate cats"[4]
As a result of these studies, rehabilitation strategies to achieve ambulation in individuals with a spinal cord injury focused on hip extension, load and other sensory elements to facilitate walking.
In the plasticity-based approach, a patient intensively practices a specific task, like locomotion, in a specific training environment while an appropriate sensory input is provided.
The training environment for individuals with spinal cord injury may include a treadmill with body-weight support (BWS), a lokomat, or an Exoskeleton. Sensory input can be provided through limb loading and unloading, trunk posture, hip extension, or limb kinematics.
Example: Locomotor training (Lokomat or treadmill with a body-weight support system):[7]
- the goal of training is to generate stepping in response to specific afferent input associated with the task of walking
- general guidelines focus on maximising loading of the lower limbs through body-weight support systems or overground walking with assistive devices
Compensatory-Based Approach[edit | edit source]
Compensation is "a rehabilitation strategy for non-remediable deficits of strength (force-generating capacity), voluntary motor control, sensation, and balance."[4]
The compensatory-based approach is based on the principle that patients learn to compensate - i.e. they use their remaining abilities to complete a task, or the task or environment are modified to achieve the established goal.[4] In this approach, walking is accomplished using orthoses and assistive devices, and the outcome depends on the degree of motor and sensory loss.
Definitions of Walking Recovery in Spinal Cord Injury[edit | edit source]
General Definitions[edit | edit source]
Functional ambulation is “the ability to walk, with or without the aid of appropriate assistive devices (such as prostheses, orthoses, canes or walkers), safely and sufficiently to carry out mobility-related activities of daily living.”[8]
Ambulatory capacity is "the highest level of walking function achieved within a standardised environment."[9]
Community ambulation is “independent mobility outside the home, which includes the ability to confidently negotiate uneven terrain, private venues, shopping centres, and other public venues.”[10]
Dimensions of community ambulation:
- Ability to manage distances
- Temporal characteristics
- gait velocity, cadence, step length, and step time
- Speed
- Ambient conditions
- lighting, air temperature and weather conditions
- Terrain
- Promkeaw et al.[12] found that the temporal spatial characteristics of ambulatory patients with spinal cord injury are affected by the surfaces they walk on
- compared to a hard surface, the average stride length, cadence, and walking speed of individuals with spinal cord injury are decreased when walking on artificial grass, soft, and pebble surfaces[12]
- Physical load
- poor road conditions, side-walks with cracks, pot-holes, etc can affect ambulation in individuals with spinal cord injury
- Attentional demands
- gait changes in response to obstacles
- Postural transitions
- ability to maintain dynamic balance affects ambulation
- Density
- the number of people and objects in the immediate surroundings affect ambulation
Definitions of Ambulation in Spinal Cord Injury Research[edit | edit source]
There is no consistent definition of walking recovery after spinal cord injury. The following definitions have been used in publications that discuss predictors for the functional outcome of walking.
Walking recovery is defined as regaining the "ability to walk independently in the community, with or without the use of devices and braces."[1]
Functional ambulation is defined as:
- "The capacity to walk reasonable distances in and out of home unassisted by another person"[13]
- "Independent mobility outside the home to access goods and services in the community”[14]
Gait speed requirements for functional ambulation in spinal cord injury depend on an individual's functional level:[15]
- Individuals who require supervision to walk indoors and are wheelchair-dependent outdoors require a minimal speed of 0.09 ± 0.01 m/s
- Individuals who can walk indoors but are wheelchair-dependent outdoors require a minimal speed of 0.15 ± 0.08 m/s
- Individuals who need a walking aid outdoors (“assisted walker”) require a minimal speed of 0.44 ± 0.14 m/s
- Individuals who walk without a walking aid require a minimal speed of 0.70 ± 0.13 m/s
Outdoor walking is "the self-reported ability to walk more than 100 m outside using one cane, leg orthosis only, or no assistive devices."[16]
Managing curbs is considered a critical task for independent community ambulation.
Predictors for Walking[edit | edit source]
Motor and Sensory Loss[edit | edit source]
- Moon et al.[17] have found that the strength of the hip flexors, followed by the knee extensors, are the most important contributors to regaining independent walking in patients with incomplete spinal cord injury
- Van Middendorp et al.[18] developed a clinical prediction rule (CPR) for ambulation outcomes after traumatic spinal cord injury. A combination of age, motor scores for L3 (quadriceps femoris) and S1 (gastrocsoleus), and light touch sensation of L3 and S1 had "excellent discrimination in distinguishing independent walkers from dependent walkers and non-walkers"[18]
- Draganich et al.[16] validated a CPR for predicting outdoor walking one year after spinal cord injury. In this CPR, L3 motor score (quadriceps), L5 motor score (big toe extensors), and S1 sensory score (light touch) were used as predictor variables[16]
- According to Cathomen and colleagues,[19] the motor score of the L2 and L3 myotomes allow us to differentiate between walkers and non-walkers. The motor score of the L4-S1 myotomes are considered prognostic factors for indoor versus outdoor walkers (with and without aids).
Level of Injury and Severity of the Spinal Cord Lesion[edit | edit source]
The International Standards for Neurological Classification of Spinal Cord Injury (ISNCSCI) is performed 72 hours after a spinal cord injury. The ISNCSCI allows clinicians to determine the neurological level of injury and the severity of the lesion. The ASIA Impairment Scale (AIS) defines complete and incomplete spinal cord lesions.
Severity of the Spinal Cord Lesion[edit | edit source]
- AIS A:[1]
- very limited possibility of achieving functional walking
- 14% of patients who convert from complete to incomplete injury recover some walking function
- patients with an AIS A spinal cord injury at the thoracic or lumbar levels (T12-L3) who regain some walking abilities will need the support of braces and devices to walk
- gait is characterised by slow average velocities and great energy expenditure, which may not be functional for the patient
- AIS B:[1]
- about 33% of patients will recover the ability to ambulate
- pinprick preservation is a positive factor in walking recovery compared to the preservation of light touch only (the preservation of pinprick sensation and light touch suggests there has been less extensive damage to the spinothalamic tracts and posterior column)
- AIS C:[1]
- around 75% of patients have a positive prognosis for walking recovery (this includes patients who convert to AIS D and those who remain AIS C but who who achieve some walking function)
- walking recovery is more likely in patients with low thoracic or lumbar lesions
- will need braces and devices to ambulate
- age is a strong prognostic factor
- 80-90% of patients younger than 50 years can walk functionally
- 30-40% of older patients can achieve the same
- AIS D:[1]
- very good ambulation prognosis at one year post-injury
- regardless of age, most patients will likely be able to walk upon discharge from the rehabilitation facility
Level of Injury[edit | edit source]
Patients with the following levels of spinal cord injury may or may not recover their walking ability:[20]
- T11-T12 levels
- may be able to ambulate at home with lower extremity orthoses and a walker
- L1-L2 levels
- may be able to ambulate with knee-ankle-foot orthoses (KAFOs) for short distances, but need a wheelchair for long distances
- L3-L4 levels
- may be able to ambulate socially with elbow crutches and ankle-foot orthoses
- L5 and lower
- may be independent in all activities
Range of Motion of the Lower Extremities[edit | edit source]
Spasticity or contracture can impact whether an individual with spinal cord injury can achieve adequate joint range of motion for walking recovery:
- full knee extension range is needed to use a KAFO for ambulation[21]
- adequate ankle dorsiflexion is necessary for foot clearance[22]
- to achieve standing when the hip extensors are absent, an individual with spinal cord injury needs full hip extension range to lean backwards and move the centre of gravity of their trunk posterior to the hip joint[23]
- individuals with spinal cord injury need 110 degrees hip flexion to transition from sitting to standing with locked KAFOs[23]
Cardiovascular Endurance[edit | edit source]
"Walking requires increased energy demands on the body and the cardiovascular system, and walking with assistive devices will pose further increased demands."[21] -- Dr. Maha Tayseer Mohammad
- A swing-through crutch-assisted gait with bilateral knee-ankle-foot orthosis requires 43 percent more of an average oxygen consumption rate than that of the patients who use a wheelchair. [24]
- A swing-through crutch-assisted gait with bilateral knee-ankle-foot orthosis requires 38 per cent more of an average oxygen consumption rate than that of the patients who walk with a normal gait pattern. [24]
- A reciprocal crutch-assisted gait with ankle-foot orthosis required 20 per cent more of an average oxygen consumption rate than that required for wheelchair use and 15 per cent greater than that required for normal walking.[24]
Age[edit | edit source]
Age is an important factor in predicting the ambulation outcome following SCI.[25]
- Older individuals with an SCI demonstrate worse functional outcomes than younger individuals.
- It is more difficult to predict walking abilities for older SCI patients as the outcomes are more variable.
Assistive Devices[edit | edit source]
The primary goals of gait rehabilitation of patients with SCI are to increase their independence and to improve their health status. A prolonged wheelchair use has disadvantages, including:[26]
- restriction to mobility due to architectural barriers
- decubitus ulcers
- osteoporosis
- joint deformities, including hip joint adduction contracture
However, the use of orthosis for ambulation in spinal cord injury comes with a list of problems that include:[26]
- Donning and doffing the orthosis takes a significant amount of time.
- Depending on the walking style, a high percentage of the force is applied to the upper limb musculature. Up to 55% of body weight can be applied on the crutch during walking, leading to shoulder pain.
- High energy demand during ambulation with orthosis and slow walking speed of individuals with SCI with an orthosis.
Orthosis[edit | edit source]
"The performance of SCI patients and the efficiency of treatment approaches should be evaluated about all aspects of functions, such as activities of daily living and participation."[27]
The evaluation of the use of orthosis for a patient with spinal cord injury should be done by a multidisciplinary team and must include the patient in the decision making to participate in the following: [28]
- Establish the orthotic and rehab goal.
- Clarify the limitations of the orthosis.
The patient must receive early education on orthosis use, and a follow-up must be scheduled to ensure the patient's safety.
The most commonly used orthosis in gait rehabilitation in spinal cord injury are:
- Hip-Knee-Ankle-Foot Orthosis (HKAFO)
- Knee-Ankle-Foot Orthosis (KAFO)
- Ankle-Foot Orthosis (AFO)
Hip-Knee-Ankle-Foot Orthosis (HKAFO)[edit | edit source]
HKAFO is an orthosis that allows a reciprocal gait. It is designed with hybrid metal and plastic, drop lock knee joints, and plastic AFO at neutral. [28]
Patient example: T12, AIS A SCI presented with the following:
- bilateral lower extremity paralysis
- good trunk and arm control
- absent sensation
- mild lower extremities oedema
- 1+ increased tone based on the Modified Ashworth Scale
Watch this video of a person who sustained a spinal cord injury after a traffic accident. He is walking with HKAFO.
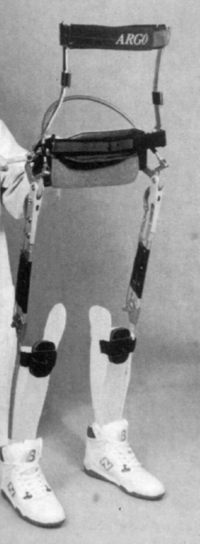
Reciprocating gait orthosis (RGOs)[edit | edit source]
Reciprocating Gait Orthosis (RGO) consists of hip-knee-ankle-foot orthosis, which allows full control of hip extension and assists with reciprocal hip flexion during the swing phase of gait. The lower limbs and the trunk are stabilised in sagittal and frontal planes. The reciprocal gait is possible due to a double or a single cable built between hip joints.
Advantages of using RGOs:[30]
- psychological benefit of assuming the upright position and talking to others at the same level
- possibility to achieve a functional level of home ambulation with limitations
Disadvantages of using RGOs:[30]
- high cost of orthosis
- discomfort with wearing the orthosis
- poor fitting
- didifficulties with donning and doffing
- slow walking as compared with wheelchair use
- difficulty with getting in and out of the car, walking outside, and climbing the stairs.
Patient example: Patient with AIS A T1 spinal cord injury
- no severe lower limb spasticity
- no lower limb oedema
- between 25 and 50 years old
Knee-Ankle-Foot Orthosis (KAFO)[edit | edit source]
KAFO can be metal, plastic, carbon, or hybrid with the following knee joint options:
- Free knee
- Drop lock
- Bail lock
- Trigger lock
- Ratchet lock
- Offset
- Trick knee
The most common design for KAFO in spinal cord injury gait rehabilitation is plastic with drop lock.
There is a new generation of stances controlling KAFO. It locks the knee joint automatically in stance but allows flexion during swing. The video below demonstrates gait training with bilateral stance controlling KAFOs.
Watch this video where a patient with a T12 spinal cord injury demonstrates walking with crutches and stairs negotiation with one crutch and one rail.
Patients with a spinal cord injury who require KAFO bilaterally for swing-through crutch-assisted ambulation prefer to use a wheelchair. [24] They use a wheelchair as the primary means of mobilisation and discontinue walking after gait training due to:[24][26]
- high energy demands during ambulation
- slow walking speed in comparison with wheelchair propulsion or normal walking[24]
Ankle-Foot Orthosis (AFO)[edit | edit source]
The AFO can be made of metal, plastic, carbon, or hybrid with anterior trim lines, mid-mall trim lines or posterior leaf springs. Plastic AFO with posterior leaf spring (PLS) is the most commonly used AFO in gait rehabilitation in spinal cord injury involving the lower lumbar spine. Thoracic or lumbar incomplete spinal cord injury may require AFO with anterior shell or anterior trim lines AFO. You can read more about different types of AFOs here.
Patient example: L4-5 spinal cord injury, AIS C presented with the following:
- Flaccid footdrop
- Mild sensory loss at the dorsum of the foot
- No oedema
- Bilateral posterior leaf AFOs
Watch the video below of a patient with an incomplete T7 spinal cord injury ambulating with bilateral AFOs with anterior shell:
Ambulatory Devices[edit | edit source]
The two most common ambulatory devices used by individuals with a spinal cord injury are walkers and crutches.
Walkers[edit | edit source]
A walker is a walking aid that provides a wide base of support. It usually has three sides, with the side closest to the patient being open. You can read more about walkers here.
Crutches[edit | edit source]
Crutches allow the person to ambulate with an increased base of support. They transfer weight from the legs to the upper body and are often used by individuals with spinal cord injuries who cannot use their legs to support their weight. You can read more about crutches here.
Footwear[edit | edit source]
When wearing orthotics, patients cannot "slip back" into their favourite pair of shoes.[35]
It is essential to emphasise the importance of appropriate footwear in promoting safe walking habits and minimising injury or falls. Remember to prioritise using suitable footwear to support the patient's rehabilitation journey.
- Proper shoe assessment must be performed, and the following should be considered:
- Presence of the lower extremities oedema
- Pressure points after the shoes are removed. Complete a thorough assessment of the ankles, heels, and toes, as the patient may not be able to feel their feet and is at risk of developing a pressure sore.
- Shoes recommended to wear with orthotics should include [36]
- Enclosed heel and toe
- Secure lace or velcro fastening
- Removable insole
- Heel height as recommended by the orthotist
Resources[edit | edit source]
- Ambulation Prediction After Spinal Cord Injury: What Have We Learned In The Past 10 Years?
- Fallahzadeh Abarghuei A, Karimi MT. The Effects of Lower Limb Orthoses on Health Aspects of the Spinal Cord Injury Patients: A Systematic Review Using International Classification of Functioning, Disability, and Health (ICF) as a Reference Framework. Med J Islam Repub Iran. 2022 Dec 14;36:153.
- Gait training in spinal cord injury
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 Scivoletto G, Tamburella F, Laurenza L, Torre M, Molinari M. Who is going to walk? A review of the factors influencing walking recovery after spinal cord injury. Frontiers in human neuroscience. 2014 Mar 13;8:141.
- ↑ Van de Crommert HW, Mulder T, Duysens J. Neural control of locomotion: sensory control of the central pattern generator and its relation to treadmill training. Gait Posture. 1998 May 1;7(3):251-263.
- ↑ Sherrington CS. Flexion-reflex of the limb, crossed extension-reflex, and reflex stepping and standing. J Physiol. 1910 Apr 26;40(1-2):28-121.
- ↑ 4.0 4.1 4.2 4.3 4.4 Behrman AL, Bowden MG, Nair PM. Neuroplasticity after spinal cord injury and training: an emerging paradigm shift in rehabilitation and walking recovery. Phys Ther. 2006 Oct;86(10):1406-25.
- ↑ Grillner S, Rossignol S. On the initiation of the swing phase of locomotion in chronic spinal cats. Brain Res. 1978 May 12;146(2):269-77.
- ↑ Hiebert GW, Whelan PJ, Prochazka A, Pearson KG. Contribution of hind limb flexor muscle afferents to the timing of phase transitions in the cat step cycle. J Neurophysiol. 1996 Mar;75(3):1126-37.
- ↑ Angeli CA, Boakye M, Morton RA, Vogt J, Benton K, Chen Y, Ferreira CK, Harkema S. Recovery of Over-Ground Walking after Chronic Motor Complete Spinal Cord Injury. N Engl J Med 2018; 379:1244-1250.
- ↑ Stroke Engine. Glossary of Terms. Available from http://www.medicine.mcgill.ca/strokengine/definitions-en.html. [last access 11.01.2023]
- ↑ Lam T, Noonan VK, Eng JJ; SCIRE Research Team. A systematic review of functional ambulation outcome measures in spinal cord injury. Spinal Cord. 2008 Apr;46(4):246-54.
- ↑ Lord SE, McPherson K, McNaughton HK, Rochester L, Weatherall M. Community ambulation after stroke: how important and obtainable is it and what measures appear predictive? Arch Phys Med Rehabil. 2004 Feb;85(2):234-9.
- ↑ 11.0 11.1 11.2 11.3 11.4 Salbach NM, O'Brien K, Brooks D, Irvin E, Martino R, Takhar P, Chan S, Howe JA. Speed and distance requirements for community ambulation: a systematic review. Arch Phys Med Rehabil. 2014 Jan;95(1):117-128.e11.
- ↑ 12.0 12.1 Promkeaw D, Arrayawichanon P, Thaweewannakij T, Mato L, Amatachaya P, Amatachaya S. Various surfaces challenge gait characteristics of ambulatory patients with spinal cord injury. Spinal Cord 2019; 57: 805–813.
- ↑ Hussey RW, Stauffer ES. Spinal cord injury: requirements for ambulation. Arch Phys Med Rehabil. 1973 Dec;54(12):544-7.
- ↑ Brehm MA, Ploeger HE, Nollet F. Self-reported functional ambulation is related to physical mobility status in polio survivors; a cross-sectional observational study. Ann Phys Rehabil Med. 2021 Jul;64(4):101428.
- ↑ van Hedel HJ; EMSCI Study Group. Gait speed in relation to categories of functional ambulation after spinal cord injury. Neurorehabil Neural Repair. 2009 May;23(4):343-50.
- ↑ 16.0 16.1 16.2 Draganich C, Weber KA 2nd, Thornton WA, Berliner JC, Sevigny M, Charlifue S, Tefertiller C, Smith AC. Predicting Outdoor Walking 1 Year After Spinal Cord Injury: A Retrospective, Multisite External Validation Study. J Neurol Phys Ther. 2023 Jul 1;47(3):155-161.
- ↑ Moon J, Yu J, Choi J, Kim M, Min K. Degree of contribution of motor and sensory scores to predict gait ability in patients with incomplete spinal cord injury. Annals of Rehabilitation Medicine. 2017 Dec 28;41(6):969-78.
- ↑ 18.0 18.1 Van Middendorp JJ, Hosman AJ, Donders AR, Pouw MH, Ditunno JF, Curt A, Geurts AC, Van de Meent H. A clinical prediction rule for ambulation outcomes after traumatic spinal cord injury: a longitudinal cohort study. The Lancet. 2011 Mar 19;377(9770):1004-10.
- ↑ Cathomen A, Maier D, Kriz J, Abel R, Röhrich F, Baumberger M, Scivoletto G, Weidner N, Rupp R, Jutzeler CR, Steeves JD; EMSCI study group; Curt A, Bolliger M. Walking Outcome After Traumatic Paraplegic Spinal Cord Injury: The Function of Which Myotomes Makes a Difference? Neurorehabil Neural Repair. 2023 May;37(5):316-327.
- ↑ Nas K, Yazmalar L, Şah V, Aydın A, Öneş K. Rehabilitation of spinal cord injuries. World J Orthop. 2015 Jan 18;6(1):8-16.
- ↑ 21.0 21.1 Mohammad MT. Gait Rehabilitation Using Orthotics in Spinal Cord Injury Course. Plus, 2024.
- ↑ Hope JM, Field-Fote EC. Assessment of Dorsiflexion Ability across Tasks in Persons with Subacute SCI after Combined Locomotor Training and Transcutaneous Spinal Stimulation. Bioengineering. 2023; 10(5):528.
- ↑ 23.0 23.1 Waters RL, Miller L. A Physiologic Rationale for Orthotic Prescription in Paraplegia. Clinical Prosthetics and Orthotics 1987;11(2):66-73.
- ↑ 24.0 24.1 24.2 24.3 24.4 24.5 Waters RL, Lunsford BR. Energy cost of paraplegic locomotion. J Bone Joint Surg Am. 1985 Oct;67(8):1245-50.
- ↑ Engel-Haber E, Zeilig G, Haber S, Worobey L, Kirshblum S. The effect of age and injury severity on clinical prediction rules for ambulation among individuals with spinal cord injury. Spine J. 2020 Oct;20(10):1666-1675.
- ↑ 26.0 26.1 26.2 Karimi MT. The physiological benefits and problems associated with standing and walking orthoses in individuals with spinal cord injury - a meta-analytic review. Journal of Orthopaedics, Trauma and Rehabilitation 2012; 16(1): 37-40.
- ↑ Fallahzadeh Abarghuei A, Karimi MT. The Effects of Lower Limb Orthoses on Health Aspects of the Spinal Cord Injury Patients: A Systematic Review Using International Classification of Functioning, Disability, and Health (ICF) as a Reference Framework. Med J Islam Repub Iran. 2022 Dec 14;36:153.
- ↑ 28.0 28.1 Uustal H. Lower Extremity Orthotics. Pathology and Prescription. Available from https://medicine.missouri.edu/sites/default/files/orthotics%20review%20case/LowerExtremityOrthotics.pdf [last access 13.01.2023]
- ↑ Hope Rehab.HKAFO - Hip Knee Ankle Foot ORTHOSIS, Helping To Rehabilitate Ahmed. Available from: https://www.youtube.com/watch?v=Zsbxak-mBNo [last accessed 13/01/2024]
- ↑ 30.0 30.1 Scivoletto G, Petrelli A, Lucente LD, Giannantoni A, Fuoco U, D'Ambrosio F, Filippini V. One year follow up of spinal cord injury patients using a reciprocating gait orthosis: preliminary report. Spinal Cord. 2000 Sep;38(9):555-8.
- ↑ Jaco Deist. Tania van Twisk, Reciprocating Gate Orthosis. Available from: https://www.youtube.com/watch?v=VoDVZjAoh7M [last accessed 18/01/2024]
- ↑ Good Shepherd Rehabilitation Network. Spinal Cord Injury: Kevin Oldt Walks in KAFO Leg Braces. Available from: https://www.youtube.com/watch?v=ikRZZMR8Wkc [last accessed 13/01/2024]
- ↑ Health is Wealth. Spinal Cord Injury: paraplegic T12 walking with elbow crutch and stair climbing training. Available from: https://www.youtube.com/watch?v=Nrr-YkVixeo [last accessed 10/02/2024]
- ↑ Jaime Newell. Walking in AFOs - T7 Incomplete spinal cord injury. Available from: https://www.youtube.com/watch?v=vSiwEqcw_5U [last accessed 13/01/2023]
- ↑ Wearing Shoes After A SCI: Three Things You Should Know. Available from https://passionatepeople.invacare.eu.com/wearing-shoes-sci-three-things-know/ [last access 9.2.2024]
- ↑ KAFO Buying Guide: What Physicians Should Know When Selecting One for Their Patients. Available from https://www.anatomicalconceptsinc.com/articles/kafo-buying-guide-what-physicians-should-know-when-selecting-one-for-their-patients [last access 9.2.2024]