Hypokalemia: Difference between revisions
No edit summary |
No edit summary |
||
| Line 4: | Line 4: | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | </div> | ||
== | == Introduction == | ||
One of the most common [[Electrolytes|electrolyte]] disturbances seen in clinical practice is hypokalemia. Hypokalemia is known as a electrolyte imbalance that is lower than normal level of potassium in your bloodstream.<ref name=":0">Castro D, Sharma S. [https://www.ncbi.nlm.nih.gov/books/NBK482465/ Hypokalemia]. 2018 Available: https://www.ncbi.nlm.nih.gov/books/NBK482465/<nowiki/>(accessed 18.9.2021)</ref> | One of the most common [[Electrolytes|electrolyte]] disturbances seen in clinical practice is hypokalemia. Hypokalemia is known as a electrolyte imbalance that is lower than normal level of potassium in your bloodstream.<ref name=":0">Castro D, Sharma S. [https://www.ncbi.nlm.nih.gov/books/NBK482465/ Hypokalemia]. 2018 Available: https://www.ncbi.nlm.nih.gov/books/NBK482465/<nowiki/>(accessed 18.9.2021)</ref> | ||
| Line 11: | Line 11: | ||
Potassium helps control how our [[Muscle|muscles]], [[Anatomy of the Human Heart|heart]], and digestive system work. Hypokalemia occurs when your body loses too much potassium or does not absorb enough from food<ref>Drugs.com [https://www.drugs.com/cg/hypokalemia.html Hypokalemia] Avaulable: https://www.drugs.com/cg/hypokalemia.html<nowiki/>(accessed 18.9.2021)</ref>. | Potassium helps control how our [[Muscle|muscles]], [[Anatomy of the Human Heart|heart]], and digestive system work. Hypokalemia occurs when your body loses too much potassium or does not absorb enough from food<ref>Drugs.com [https://www.drugs.com/cg/hypokalemia.html Hypokalemia] Avaulable: https://www.drugs.com/cg/hypokalemia.html<nowiki/>(accessed 18.9.2021)</ref>. | ||
Few people meet the daily recommended potassium intake, which is 3,400 mg for men and 2,600 mg for women. Nevertheless, hypokalemia is rarely caused by dietary deficiency alone. It can be caused by a number of factors, including fluid loss, malnutrition, shock, using certain medications, and medical conditions like kidney failure.<ref name=":1">Healthline Hypokalemia Available: https://www.healthline.com/nutrition/potassium-deficiency-symptoms#bottom-line (accessed 3.6.2022)</ref> | |||
== Etiology == | == Etiology == | ||
| Line 18: | Line 20: | ||
# Transcellular shifts (increased intracellular uptake) | # Transcellular shifts (increased intracellular uptake) | ||
# Increased potassium loss (skin, gastrointestinal, and renal losses)<ref name=":0" /> | # Increased potassium loss (skin, gastrointestinal, and renal losses)<ref name=":0" /> | ||
Certain illnesses or other factors more likely the cause of hypokalemia, these include: | |||
* Chronic diarrhea. | * Chronic diarrhea. | ||
* Certain medications. eg diuretics, beta 2-agonists, theophylline, insulin, corticosteroids, and antimicrobials. | * Certain medications. eg [[diuretics]], beta 2-agonists, theophylline, insulin, corticosteroids, and antimicrobials. | ||
* Eating disorders. eg anorexia nervosa, refeeding syndrome, purging, laxative abuse. | * Eating disorders. eg anorexia nervosa, refeeding syndrome, purging, laxative abuse. | ||
* Cushing’s syndrome | * Cushing’s syndrome | ||
| Line 65: | Line 67: | ||
Management of the underlying disease or contributing factors constitutes the cornerstone of therapeutic approach. Potassium should be gradually replaced, preferably by oral administration if clinically feasible. In cases of severe/symptomatic hypokalemia and cardiac complications, i.v. administration with continuous ECG monitoring is recommended. In some patients, such as in endocrine related hypokalemia cases, multidisciplinary diagnostic and therapeutic approach is needed.<ref>Kardalas E, Paschou SA, Anagnostis P, Muscogiuri G, Siasos G, Vryonidou A. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5881435/ Hypokalemia: a clinical update. Endocrine connections]. 2018 Apr 1;7(4):R135-46. Available:https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5881435/ (accessed 18.9.2021)</ref> | Management of the underlying disease or contributing factors constitutes the cornerstone of therapeutic approach. Potassium should be gradually replaced, preferably by oral administration if clinically feasible. In cases of severe/symptomatic hypokalemia and cardiac complications, i.v. administration with continuous ECG monitoring is recommended. In some patients, such as in endocrine related hypokalemia cases, multidisciplinary diagnostic and therapeutic approach is needed.<ref>Kardalas E, Paschou SA, Anagnostis P, Muscogiuri G, Siasos G, Vryonidou A. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5881435/ Hypokalemia: a clinical update. Endocrine connections]. 2018 Apr 1;7(4):R135-46. Available:https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5881435/ (accessed 18.9.2021)</ref> | ||
Though diet alone usually will not resolve hypokalemia, it’s still beneficial to increase intake of potassium-rich foods, like fruits, vegetables, beans, and nuts<ref name=":1" />. | |||
The majority of patients who are treated for hypokalemia have a good outcome but those who remain untreated are at a risk for arrhythmias which may be fatal.<ref name="medline" /> | The majority of patients who are treated for hypokalemia have a good outcome but those who remain untreated are at a risk for arrhythmias which may be fatal.<ref name="medline" /> | ||
Revision as of 02:54, 3 June 2022
Original Editors - Kara Lawless from Bellarmine University's Pathophysiology of Complex Patient Problems project.
Top Contributors - Kara Lawless, Elaine Lonnemann, Lucinda hampton, Admin, Kim Jackson, Wendy Walker and WikiSysop
Introduction[edit | edit source]
One of the most common electrolyte disturbances seen in clinical practice is hypokalemia. Hypokalemia is known as a electrolyte imbalance that is lower than normal level of potassium in your bloodstream.[1]
- A normal blood potassium is 3.6 to 5.2 mmol/L.
- Severe and life threatening hypokalemia level is known as <2.5mmol/L. [2]
Potassium helps control how our muscles, heart, and digestive system work. Hypokalemia occurs when your body loses too much potassium or does not absorb enough from food[3].
Few people meet the daily recommended potassium intake, which is 3,400 mg for men and 2,600 mg for women. Nevertheless, hypokalemia is rarely caused by dietary deficiency alone. It can be caused by a number of factors, including fluid loss, malnutrition, shock, using certain medications, and medical conditions like kidney failure.[4]
Etiology[edit | edit source]
Potential etiologies resulting in hypokalemia are put into the following categories:
- Decreased potassium intake
- Transcellular shifts (increased intracellular uptake)
- Increased potassium loss (skin, gastrointestinal, and renal losses)[1]
Certain illnesses or other factors more likely the cause of hypokalemia, these include:
- Chronic diarrhea.
- Certain medications. eg diuretics, beta 2-agonists, theophylline, insulin, corticosteroids, and antimicrobials.
- Eating disorders. eg anorexia nervosa, refeeding syndrome, purging, laxative abuse.
- Cushing’s syndrome
- Hyperaldosteronism.
- Kidney failure and Kidney disorders.
- Hypomagnesemia.
- Overconsumption of licorice
- Excessive sweating
Characteristics/Clinical[edit | edit source]
In most cases, low potassium is found by a blood test that is done because of an illness, or because of diuretics use. It is rare for low potassium to cause isolated symptoms eg muscle cramps if person is feeling well in other respects.
Hypokalemia symptoms may include:
- Weakness
- Fatigue
- Muscle cramps
- Constipation
Abnormal heart rhythms (arrhythmias) are the most worrisome complication of very low potassium levels, particularly in people with underlying heart disease[5].
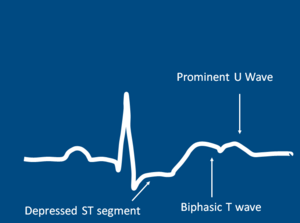
Diagnostic Tests/Lab Tests/Lab Values[edit | edit source]
Hypokalemia is commonly found in a blood test, with <3.5mmol/L as mild hypokalemia and <2.5mmol/L as severe hypokalmia.[2]
In severe cases, a 12-lead electrocardiogram may be necessary if to check for cardiac arrythymias. Findings such as T-wave flattening or prominent U waves will result in hospital admission.[6] Other tests may include:
- arterial blood gas
- basic or comprehensive metabolic panel
Blood tests will also be administered to check the following:
- glucose
- magnesium
- calcium
- sodium
- phosphorus
- thyroxine
- aldosterone levels.[7]
Management[edit | edit source]
The overarching goals of therapy for hypokalemia are to prevent or treat life-threatening complications, replace the potassium deficit, and to diagnose and correct the underlying cause.[1]
Management of the underlying disease or contributing factors constitutes the cornerstone of therapeutic approach. Potassium should be gradually replaced, preferably by oral administration if clinically feasible. In cases of severe/symptomatic hypokalemia and cardiac complications, i.v. administration with continuous ECG monitoring is recommended. In some patients, such as in endocrine related hypokalemia cases, multidisciplinary diagnostic and therapeutic approach is needed.[8]
Though diet alone usually will not resolve hypokalemia, it’s still beneficial to increase intake of potassium-rich foods, like fruits, vegetables, beans, and nuts[4].
The majority of patients who are treated for hypokalemia have a good outcome but those who remain untreated are at a risk for arrhythmias which may be fatal.[7]
Physical Therapy Management[edit | edit source]
Hypokalemia is not managed primarily by a physical therapist. Physical therapists should be mindful of common signs of symptoms of hypokalemia when working with patients.
- Potassium levels < 3.2 mEq/L is contraindicated for physical therapy intervention due to the potential for arrhythmia . Due to muscle weakness and cramping, exercise is not effective during the state of hypokalemia.
- Patients should be monitored for potassium levels in order to determine the appropriate time to participate in Physical Therapy.[9]
Differential Diagnosis[edit | edit source]
- Bartter syndrome
- Hyperthyroidism and thyrotoxicosis
- Hypocalcemia
- Hypochloremic alkalosis
- Hypomagnesemia
- Iatrogenic Cushing syndrome
- Metabolic alkalosis
References[edit | edit source]
- ↑ 1.0 1.1 1.2 Castro D, Sharma S. Hypokalemia. 2018 Available: https://www.ncbi.nlm.nih.gov/books/NBK482465/(accessed 18.9.2021)
- ↑ 2.0 2.1 Low Potassium(hypokalemia)[Internet]. 2012 August 10 [cited 2013 March 27] Available from:http://www.mayoclinic.com/health/low-potassium/MY00760
- ↑ Drugs.com Hypokalemia Avaulable: https://www.drugs.com/cg/hypokalemia.html(accessed 18.9.2021)
- ↑ 4.0 4.1 Healthline Hypokalemia Available: https://www.healthline.com/nutrition/potassium-deficiency-symptoms#bottom-line (accessed 3.6.2022)
- ↑ Mayo Clinic Hypokalemia Available: https://www.mayoclinic.org/symptoms/low-potassium/basics/when-to-see-doctor/sym-20050632 (accessed 19.9.2021)
- ↑ Hypokalemia [Internet]. 2012 [cited 2013 March 27] Available from:https://www.clinicalkey.com/topics/nephrology/hypokalemia.html#720089
- ↑ 7.0 7.1 Hypokalemia [Internet]. 2013 March 22 [cited 2013 March 27] Available from: http://www.nlm.nih.gov/medlineplus/ency/article/000479.htm
- ↑ Kardalas E, Paschou SA, Anagnostis P, Muscogiuri G, Siasos G, Vryonidou A. Hypokalemia: a clinical update. Endocrine connections. 2018 Apr 1;7(4):R135-46. Available:https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5881435/ (accessed 18.9.2021)
- ↑ Goodman CC. Fuller KS. In K Falk editor. Pathology: Implications for the Physical Therapist. St. Louis: Saunders Elsevier; 2009. pp.150, 157, 187-189, 480, 558, 927, 1243, 1640-1641
see adding references tutorial.