Greater Trochanteric Pain Syndrome
Original Editors - Kirianne Vander Velden
Top Contributors -Wendy Snyders, Kim Jackson, Admin, Lucinda hampton, Uchechukwu Chukwuemeka, Habibu Salisu Badamasi, Rishika Babburu, Andrea Nees and WikiSysop
Description[edit | edit source]
Lateral hip pain previously used to be referred to as trochanteric bursitis but this has been replaced by Greater Trochanteric Pain Syndrome (GTPS). GTPS is a clinical diagnosis of lateral hip pain and includes trochanteric bursitis associated with a tendinopathy[1][2][3] ,gluteus medius (GMed) and minimus (GMin) tendinopathy[3][4][5][6], tears of the GMed and GMin tendons[6][3] and external coxa saltans (snapping hip syndrome)[6][4]. Iliotibial band (ITB) abnormalities are also a possible cause of GTPS[1]. Fearon et al. (2012) proposed a clinical definition of GTPS: “a history of lateral hip pain and no difficulty with manipulating shoes and socks together with clinical findings of pain reproduction on palpation of the greater trochanter and lateral pain reproduction with the FABER test[7].” This was proposed as the authors found that being able to manipulate socks and shoes without pain differentiates GTPS from hip osteoarthritis (OA) and a positive FABER is sensitive and specific for GTPS[7].
Previously, trochanteric bursitis was seen as the main pain source, but recent research indicates that the fluid within the bursa rather exists due to the gluteal tendinopathy and not because of primary inflammation in the bursa[1][2][8]. The most recent research indicates GMed and GMin tendinopathy as the most frequent cause of GTPS[9][8][10][11][5] and managing the underlying tendinopathy should take priority[3]. GTPS is more common in females (outnumbering men by between 2.4 – 4: 1[9]) between the ages of 40 and 60[2][6][11] and accounts for 10 – 20% of patients presenting with hip pain in primary care. It has an incidence between 1.8 and 5.6 per 1000 per year[12][2][13][6].
Clinically Relevant Anatomy[edit | edit source]
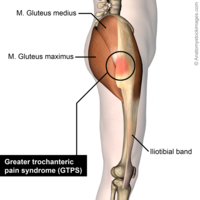
The greater trochanter is situated on the proximolateral side of the femur, just distal to the hip joint and the neck of the femur. The tendons of the GMed, GMin, gluteus maximus (GMax) and the tensor fascia lata (TFL) attach onto this bony outgrowth (apophysis). The greater trochanter is seen to have 4 facets by Pfirrmann et al.[14] and the above-mentioned muscle attachments have been equated to the “rotator cuff of the hip”[15][5].
The external iliac fossa is the origin of the GMed and GMin muscles, with the GMed attaching to the lateral and superolateral facets and the GMin inserting onto the anterior facet. The TFL lies over the GMed and GMin tendons and inserts onto the ITB[14].
The greater trochanteric region has a varying number of bursa but has an average of 6 bursae[16]. Williams and Cohen (2009) report that four bursae are consistently present and that there are multiple secondary bursa[17]. Bursae are fluid-filled structures that reduce friction between bones and soft tissues[14]. The three chief bursae at the hip include the subgluteus maximus, the subgluteus minimus and the subgluteus medius bursa[14]. These bursae and the periosteum of the greater trochanter are innervated by a small branch of the femoral nerve[14][18]. The locations of these bursae vary greatly when observed on cadavers - the size, location and number are not consistent [19][17][20].
The GMax muscle tensions the ITB via its ITB attachment and assists with improving the hip joint’s passive stability[21]. The ITB is also tensioned by the vastus lateralis and TFL and limits hip internal rotation and adduction passivley[21]. The GMed prevents excessive hip adduction and is often seen as the primary stabilizer of the pelvis[21].
The hip joint is innervated by rami articulares of the obturator nerve, the femoral nerve and the sciatic nerve[22] and the recently discovered branch of the femoral nerve that supplies the periosteum and bursa of the greater trochanter. This discovery may be useful to improve therapies, such as interventional denervation of the greater trochanter or anatomically guided injections with corticosteroids and local anesthetics[18]. The GMed, GMin and TFL are innervated by the superior gluteal nerve while the GMax is innervated by the inferior gluteal nerve.
Aetiology and pathomechanics[edit | edit source]
Since GMed and GMin tendinopathy, tears of the GMed and GMin tendons, external coxa saltans and ITB abnormalities can all be possible causes of GTPS, the aetiology of each of these structures/pathologies need to be considered.
Tendinopathy is a multifaceted problem and the exact mechanism is still not known.1Overuse of tendons[6], mechanical overload[6][11] and incomplete or failed healing1 have all proposed as possible causes of tendinopathy. Compression of the tendon at the enthesis is another possible cause[11] for insertional tendinopathies. A combination of high tensile loads and excessive compression is thought to be most detrimental[11].
In people with weak hip abductors, particularly GMed, greater hip adduction is seen causing increased compression of the GMed and GMin tendons at the greater trochanter. With the increased adduction, the ITB exerts higher compressive forces on the gluteal tendons, amplifying the compression[3]. Hip positions in higher ranges of flexion may also increase the compression of the GMed and GMin tendons due to increased tension in the ITB, explaining why pain that occurs with prolonged sitting[11].
Kummer (1993) found that pelvic control in a single leg stance position was controlled 70% by the abductor muscles and that the ITB tensioners (GMax, TFL and vastus lateralis) then accounted for the remaining 30%[11]. This is seen as the abductor mechanism. It has also been shown that people with gluteal tendinopathy tend to have GMed and GMin atrophy and TFL hypertrophy. Weakness and/or muscle bulk changes impact the balance of the abductor mechanism and increase the compression of the gluteal tendons[11].
It is postulated that women are more prone to GTPS because of pelvic biomechanics, different activity levels in the population and hormonal effects[14]. One study found that females have a smaller insertion of the GMed tendon, resulting in a smaller area across which tensile load could be dissipated. It also makes the moment arm shorter, causing reduced mechanical effeciency[9].
A previously mentioned, any increased fluid within the bursa is thought to be a consequence of the tendinopathy rather than it being due to inflammation of the bursa. This being said, one smaller study found that there was an increase in substance P within the bursa in patients with GTPS and specifically gluteal tendinopathy indicating that the bursa is a possible source of pain in GPTS[23].
Tears of the GMed and GMin tendons are a frequently missed cause of GTPS[24]. According to Domb et al. (2010), up to 25% of middle-aged women can have GMed tears, and up to 10% of middle-aged men[24]. Tears can be acute but degenerative tears are far more common with the GMed tendon being most frequently affected[5][24]. These tears at the GMed tendon insertion can be complete, intrasubstance or partial, with partial tears occurring most frequently[5][24].
Coxa saltans or snapping hip syndrome presents in about 5% to 10% of the general population[25]. It is either intra-articular or extra-articular[25], with the extra-articular presentation being relevant to GTPS. Extra-articular coxa sultans most commonly involves the anterior part of GMax or the posterior ITB snapping over the greater trochanter, causing a catching or sensation of “giving way” and an inflammatory response in the trochanteric bursa.[25][26]. There is also often an imbalance between TFL and GMax activation in these patients[26]. Patients can report a sensation of subluxation and pain is worst with activities such as climbing stairs, hiking and running[25]. There are, however, patients who do not experience pain when it snaps[26]. Coxa saltans is most commonly found in dancers and professional athletes, but can also occur due to physical trauma[25].
Risk factors in athletes include[14]:
- Running on an asymmetrical surface, cambered road
- Shoe wear
- Incorrect training
There is no clear evidence that a leg length discrepancy has any impact on a person developing GTPS[7][14].
Patients presenting with GTPS often have low back pain[6][9][13] or hip joint OA[6]. There is also a higher occurrence of GTPS in people with ITB syndrome and knee OA[27][14].
Characteristics/Clinical Presentation[edit | edit source]
GTPS typically presents with lateral hip pain that may radiate down the lateral thigh and buttocks and occasionally to the lateral knee. It can be described as aching and intense at times of greater aggravation caused by passive, active and resisted hip abduction and external rotation[20]. It is often characterized by the ‘jump’ sign where palpation of the greater trochanter causes the patient to nearly jump off the bed[2].
The symptoms include:
- Tender lateral hip when palpated, especially near the greater trochanter[14][10][9][5][24]
- Pain with side-lying on the problematic side[14][10][9][28]
- Pain with weight-bearing activities such as walking, climbing stairs, standing and running[14][10][9][2][24][28][29]
- Pain may refer to the lateral thigh and knee[14][9][2][5]
- Pain with prolonged sitting[9][28]
- Pain with resisted abduction[5][24]
- Sitting with crossed legs increases pain[9]
- Pain can also occur when lying on the non-painful side if the painful hip falls into adduction
- Pain is usually episodic and will worsen over time with continued aggravation
- Weak hip abductors[29]
Differential Diagnosis[edit | edit source]
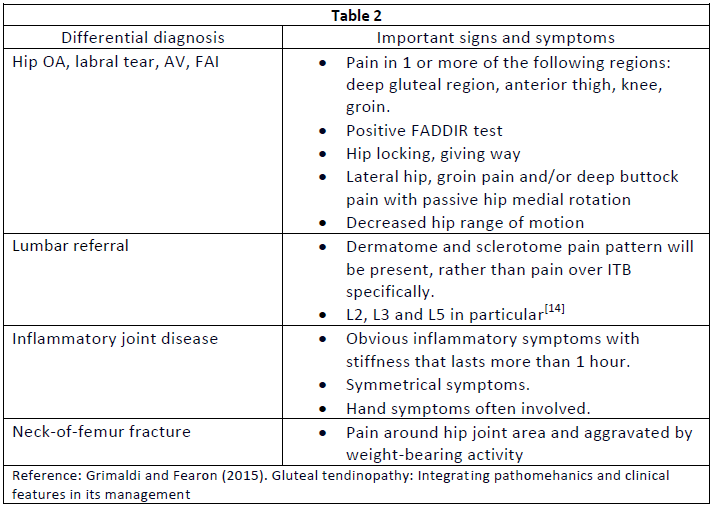
To be able to treat GTPS correctly, accurate differential diagnosis is crucial[7]. Conditions that may mimic GTPS include the following:
- Hip OA[7][29][14][11][9]. Similar site of symptoms, aggravated by weight-bearing activity and weakness in hip abductors[29].
- Femoral head avascular necrosis (AV)[30][14]
- Femoroacetabular impingement (FAI)[30][14][9]
- Lumbar spine referral or degenerative disease[30][11][9]
- Femoral-head stress fractures[14]
- Labral tears[14][9]
- Bony metastasis[9]
- Neck-of-femur fracture[9]
- Inflammatory disease such as RA[9]
Table 2 includes some important signs and symptoms of the differential diagnoses[9][14]:
Diagnostic Procedures[edit | edit source]
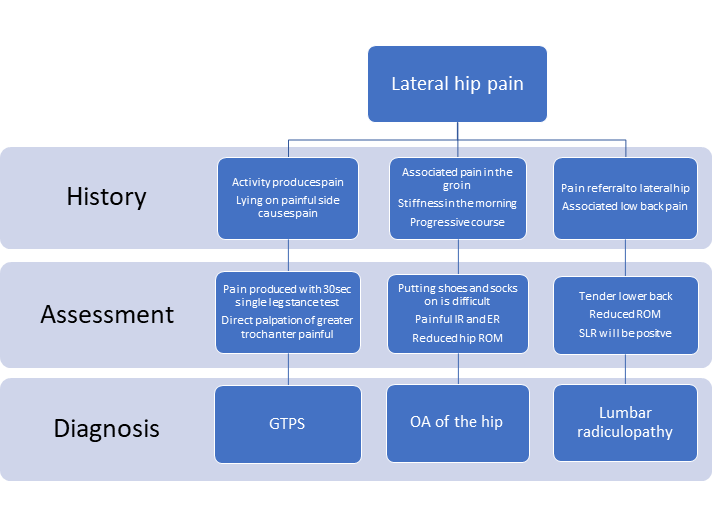
There is no one specific test to confirm GTPS and the tests available lack validity when done in isolation. Diagnostic accuracy can however be improved when a combination of tests is used[2].
When using pain provocation tests, the diagnostic value can be improved by the patient reporting pain on the specific site[9].
The single leg stance test for 30 seconds has a positive predictive value (PPV) of 100% and also has a very high sensitivity when pain is produced within 30 seconds of standing on the painful side[2],[14]. Grimaldi and Fearon (2015) however suggest that the test be done either to 30 seconds or until symptom production, whichever comes first[9].
Resisted hip medial rotation, lateral rotation and abduction can also be used to asses for GTPS. Resisted lateral rotation has the highest sensitivity (88%) and specificity (97.3%) when compared to resisted medial rotation and abduction[9]. Resisted medial rotation has been most assessed but the results change based on the position of the hip during the test. The highest sensitivity is achieved when medial rotation is assessed through range from end of range lateral rotation in prone. The highest specificity is achieved when the test is done in 90° hip flexion[11].
The FADER, OBER and FABER tests can also be added as they aim to increase the tensile load on the gluteal tendons[2]. The FABER test has a sensitivity of 82.9% and a specificity of 90% while the Ober test has a sensitivity of 41% and a specificity of 95%[9]. Fearon et al. (2012) found that the FABER test was the key test when differentiating between hip OA and GTPS, where a positive FABER with lateral hip symptoms indicates GTPS[7]. As mentioned previously, the ability to put one’s socks and shoes on without help will also help differentiate GTPS from OA, where the GTPS patient has no difficulty during the acitivity[2].
The “jump sign” carries a PPV of 83% so direct palpation of the greater trochanter is helpful in diagnosing GTPS[2]. The Trendelenburg sign is present in patients with GTPS and when used to assess for a GMed tear, it has a sensitivity of 73% and a specificity of 77%[14].
If external coxa saltans is suspected, the suggested clinical tests include FABER, Ober test, Hula-Hoop test and active hip flexion followed by passive extension and abduction[31].
Imaging is only suggested in the following situations:
- When it comes to diagnosing gluteal tears. Ultrasound or MRI should be used to confirm the diagnosis if suspected clinically[24][14]. Cook (2020) reports that ultrasound is the most accurate when assessing a tendon where MRI is helpful for differential diagnosis[32].
- When conservative treatment has failed[14][9].
- When diagnosis is unclear[9][14].
Below is a diagnostic flow chart created by Speers and Bhogal (2017) for the 3 most common causes of lateral hip pain[2].
Outcome Measures[edit | edit source]
- VISA-G - GTPS-specific outcome measure[33]
- HOOS - Hip Disability and Osteoarthritis Outcome Score
- HHS - Harris Hip Score
- iHOT - International Hip Outcome Tool
Examination[edit | edit source]
GTPS is a clinical diagnosis which means the diagnosis is based on the medical history as well as the signs and symptoms. This means that the assessment must include a good subjective assessment, so as to gather the necessary information regarding the signs and symptoms. Aside from doing a proper hip assessment, the below special tests can be used to help confirm or negate the suspected diagnosis of GTPS. In 2017, Ganderton et al. validated the following tests for GTPS: FABER, resisted external derotation test, greater trochanter palpation and resisted abduction[34]. Please click on the link to each test for more detailed information and/or a video regarding each test.
Trendelenburg Test: This is a quick test for assessing hip abductor muscle function and it can also be used to help determine if a tear is present in the hip abductors.A drop of the pelvis on the contralateral side of the stance leg indicates weakness of the stance leg's hip abductors and results in a positive test. Test administration is demonstrated here.
FABER Test: FABER is the acronym for flexion, abduction, external rotation. It is very helpful in confirming GTPS[7] and it assists with differentiating between hip OA and GTPS[2].
Noble Test: This is used to verify Iliotibial tightness and helps to distinguish iliotibial tightness from other common causes of lateral knee pain, such as lateral collateral ligament strain, bicipital or popliteal tendinopathy, knee OA and lateral meniscal pathology[35].Test administration is demonstrated here.
Modified Ober’s Test:This test and its modification are used to assess the TFL and ITB. The test is positive if the thigh does not go further than 10 degrees adduction.
Renne’s Test: This test is used to assess ITB syndrome and can be done alone or in conjunction with the Noble Test.
(30 second ) Single leg stance test: The person being tested must stand, unassisted, on one leg with their eyes open and one finger on a wall. As soon as the person’s foot is lifted of the floor, the 30 seconds start. A positive test for patients with GTPS is lateral hip by 30 seconds. Grimaldi and Fearon (2015) suggest holding the position until reproduction of symptoms[9].
Resisted external de-rotation test and modified external de-rotation test: The patient lies in supine and the examiner then passively flexes the hip to 90° with external rotation. The hip should be in neutral abduction/adduction. Slightly reduce the external rotation to decrease the compression of the tendon. The patient then actively rotates their leg to neutral against the therapist’s resistance. The modified test is exactly the same, but done in full hip adduction.[34]
Resisted abduction test: The examiner passively abducts the testing-limb to 45° abduction with the patient in side-lying or supine. The patient must then maintain this position against the examiner’s resistance. The resistance must be applied 1cm superior to the lateral malleolus[34]. This test has a 73% sensitivity and 87% specificity for GMed pathology[36].
Resisted internal rotation: This test has a 92% sensitivity, 85% specificity and 88% accuracy for diagnosing GMed tears . To perform the test, place the problematic limb into 90° hip and knee flexion with 10° hip external rotation while the patient lies in supine. While the examiner provides resistance to the movement, the patient must perform active hip internal rotation. The test is positive if the patient experiences pain and/or weakness.[36]
Management[edit | edit source]
Physiotherapy management of GTPS is poorly described but conservative management is very effective[6]. The main goals should however include[2]:
- Load management
- Reduction of compressive forces
- Strengthening of the gluteal muscles and
- Management of any comorbidities
Surgery should only be done if conservative management has failed[2] or when there is a significant tendon tear[9].
Non-Surgical Intervention[edit | edit source]
Non-surgical treatment options include the following:
- Physiotherapy, which includes manual therapy and therapeutic exercise
- PRP injections
- Corticosteroid injections
- Low energy extracorporeal shockwave therapy (ESWT)
Non-steroidal anti-inflammatory drugs (NSAIDs) may help with analgesia in the acute phase or in primary bursitis, but it is not advised in chronic gluteal tendinopathy or gluteal tendon tears as NSAIDs have been found to potentially have a negative impact on tendon healing[14].
Therapeutic Modalities
The best documented therapeutic modalities include ESWT and corticosteroid injections:
- ESWT was found to be more effective than corticosteroid injections and multimodal therapy at a 1 year follow-up. The long-term results of ESWT are however controversial[37]. A study that combined exercise and ESWT found that this approach was superior to corticosteroid injection for pain relief at 15 months follow-up[14].
- Corticosteroid injection has been found to be effective in the short-term only[37] (3 to 4 months[11]) and is advised for bursitis rather than tendinopathy[14]. McEvoy et al. (2012) found that it was more effective to inject the greater trochanteric bursa than the subgluteus medius bursa[27]. It is worth mentioning that a study published in 2018 found that there was no difference between giving a corticosteroid injection or a saline injection and the conclusion was that corticosteroid injection was of limited benefit[13]. In this study, the needle was either placed into the trochanteric bursa or the GMed tendon if the bursa could not be visualised[13].
Platelet-Rich Plasma injections have been found to be a feasible alternative but it is unknown whether it or corticosteroids are more effective.
Dry-needling is a commonly-used intervention in physiotherapy. A study published in 2017 compared dry-needling to corticosteroid injections for pain relief in GTPS and found that corticosteroid injections did not offer greater pain relief or to dry-needling. There was also no difference in function improvement between the two groups. Based on this, dry needling may be a viable option for pain relief in GTPS[38].
Other modalities like TENS, cross-frictions and low-level laser have not been assessed properly for GTPS[39]. Ice and heat have been suggested for pain management, but there is limited supporting evidence[39] and there are no studies proving the effectiveness of ultrasound[39].
Manual Therapy
Myofascial restrictions of the joints below the hip, the hip itself and the lumbar spine can result in increased friction at the lateral hip and myofascial release is therefore indicated if a restriction is found[39]. Where joint restrictions exist at the lumbar spine, hip, knee and/or ankle, joint mobilization can be done to improve mobility, thereby correcting hip biomechanics and reducing friction at the lateral hip[39].
Education
Patients must be made aware of activities and positions that may further compress the gluteal tendons/bursa resulting in aggravated symptoms. Patients should avoid:
- Climbing stairs[28]
- Hip adduction across the midline[28][9]
- Walking uphill[28]
- Sitting with legs crossed[28][9]
- Sitting with their knees higher than hips[28]
- Standing with more weight on one leg[28][9]
- Side-lying postions[28]. If the patient struggles not to lie on their side, they should place pillows between their knees and ankles (modified side-lying) or lie on an eggshell overlay[9]
- Stretching of the ITB, gluteal muscles[9]
Advice regarding modification of exercise and activity should also be given[9]. This is further discussed in the therapeutic exercise paragraph below.
Therapeutic Exercise
Sadly, there is little evidence of the effect of exercise on pain and dysfunction in GTPS[28]. More recently, some studies have examined different exercise approaches which include the following:
Isometric contractions (for gluteal tendinopathy)
Isometric contractions are now commonly used as they release cortical inhibition targeting both peripheral and central pain drivers. This cortical inhibition causes immediate pain reduction and for 45 minutes afterwards[28]. Cook (2020) reported that the analgesic effect can last for 4 to 8 hours after isometrics[32]. Isometric contractions must be heavy to effectively achieve pain relief in the tendon[40][32]. The exact duration of the contraction is unknown, but 5 repetitions of 45 seconds has been found to be very effective[9][40][32]. A rest period of 2 minutes must occur between each of the isometric contractions[32].
Avoid Stretching
Stretching should be avoided when treating insertional tendinopathies as stretching, especially into adduction with the hip in flexion or extension increases the compression forces on the tendon[9].
Exercise
Exercise is important in the management of all the possible causes of GTPS:
- Gluteal tendinopathy requires gradual loading of the tendons to condition the tendon again so that it can tolerate load. More information about gluteal tendinopathy management can be found on the Gluteal tendinopathy page.
- Since Trochanteric bursitis is reported to most likely be secondary to a gluteal tendinopathy, gradual loading is also indicated in these patients.
- In patients with gluteal tendon repair, strengthening will be essential for optimal function and to improve the repaired tissue’s tensile strength.
- Patients with external coxa saltans may be experiencing the problem due to muscle imbalances or increased muscle tension which will require modification of neuromuscular control. This is achieved through the correct strengthening and/or motor control exercise.
Therapeutic exercise should be started early and consist of progressive tensile loading exercises in minimally adducted hip positions[9]. GMed has been found to activate better in weight-bearing positions compared to non-weight-bearing positions[9]. Exercise should be started at a moderate effort level and repetitions should be low. When night pain improves in patients with a gluteal tendinopathy, it is a good indicator that the tendon is responding to the exercise. If night pain increases it may indicate that the load was too high[9].
Strengthening should not only include the hip abductors but also the core and lumbopelvic stabilisers[14].
Ebert et al. (2018) provide a guideline for postoperative management for abductor tendon repair[41]. This guideline can be found in Table 2 below.
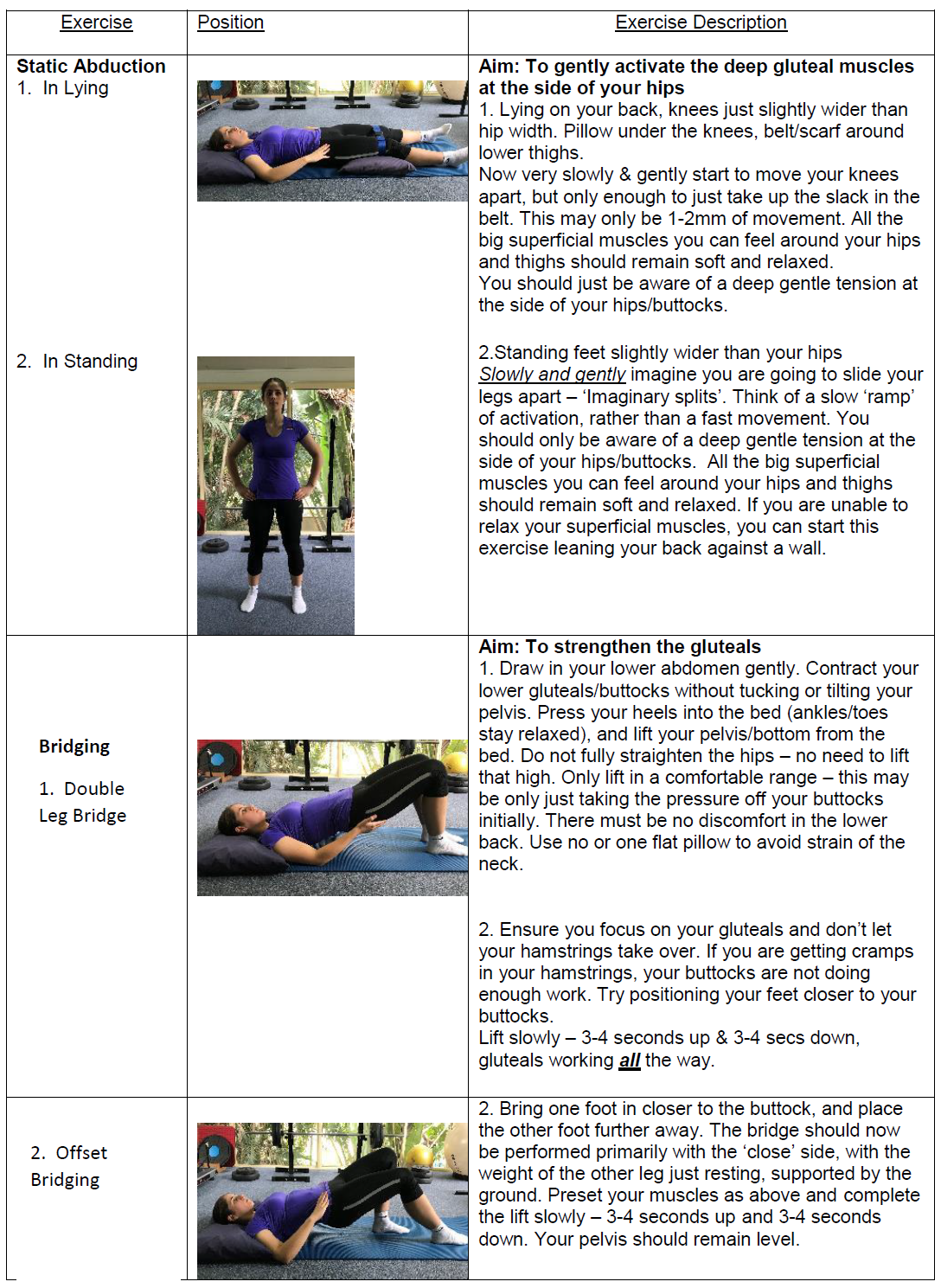
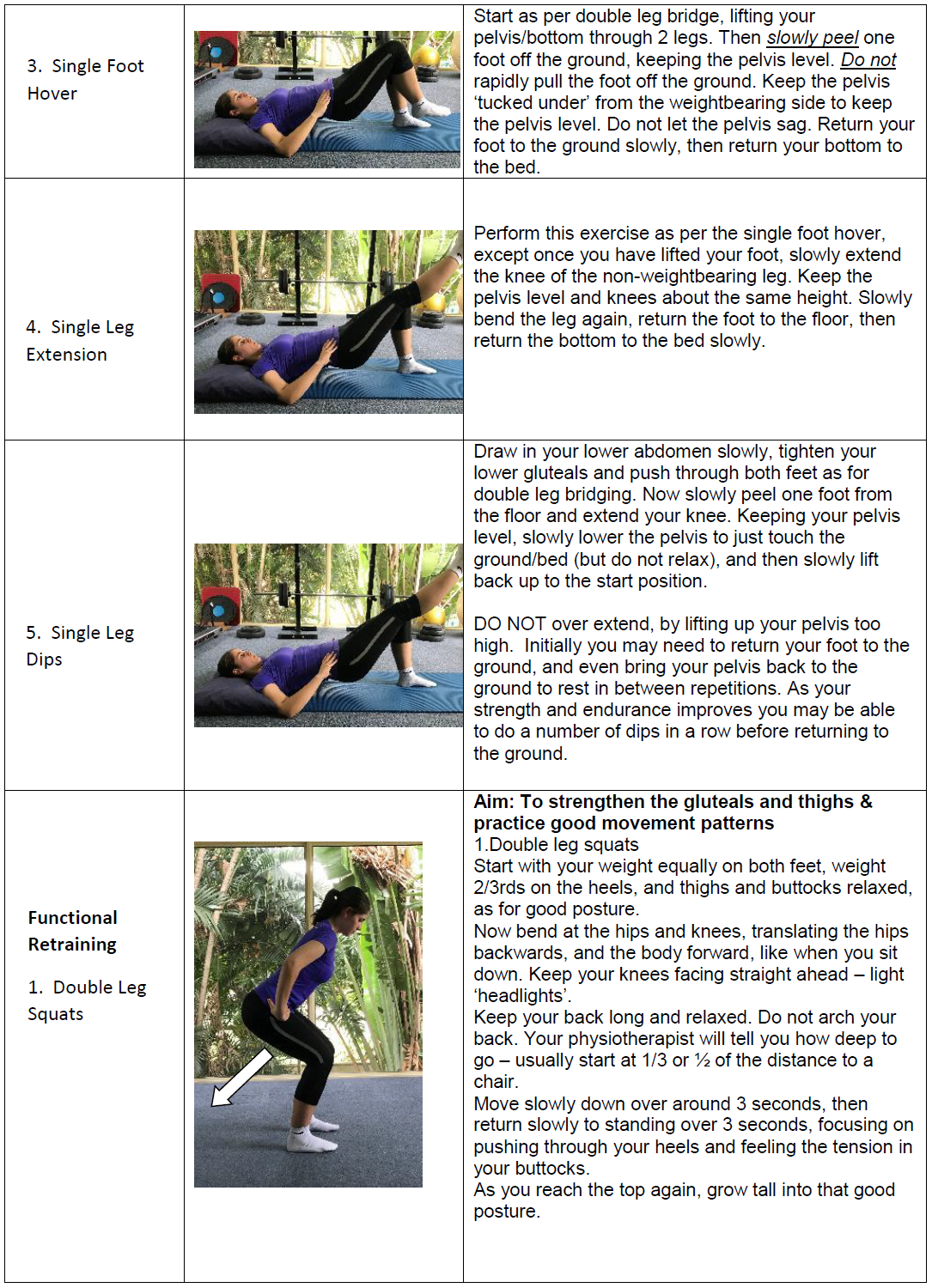
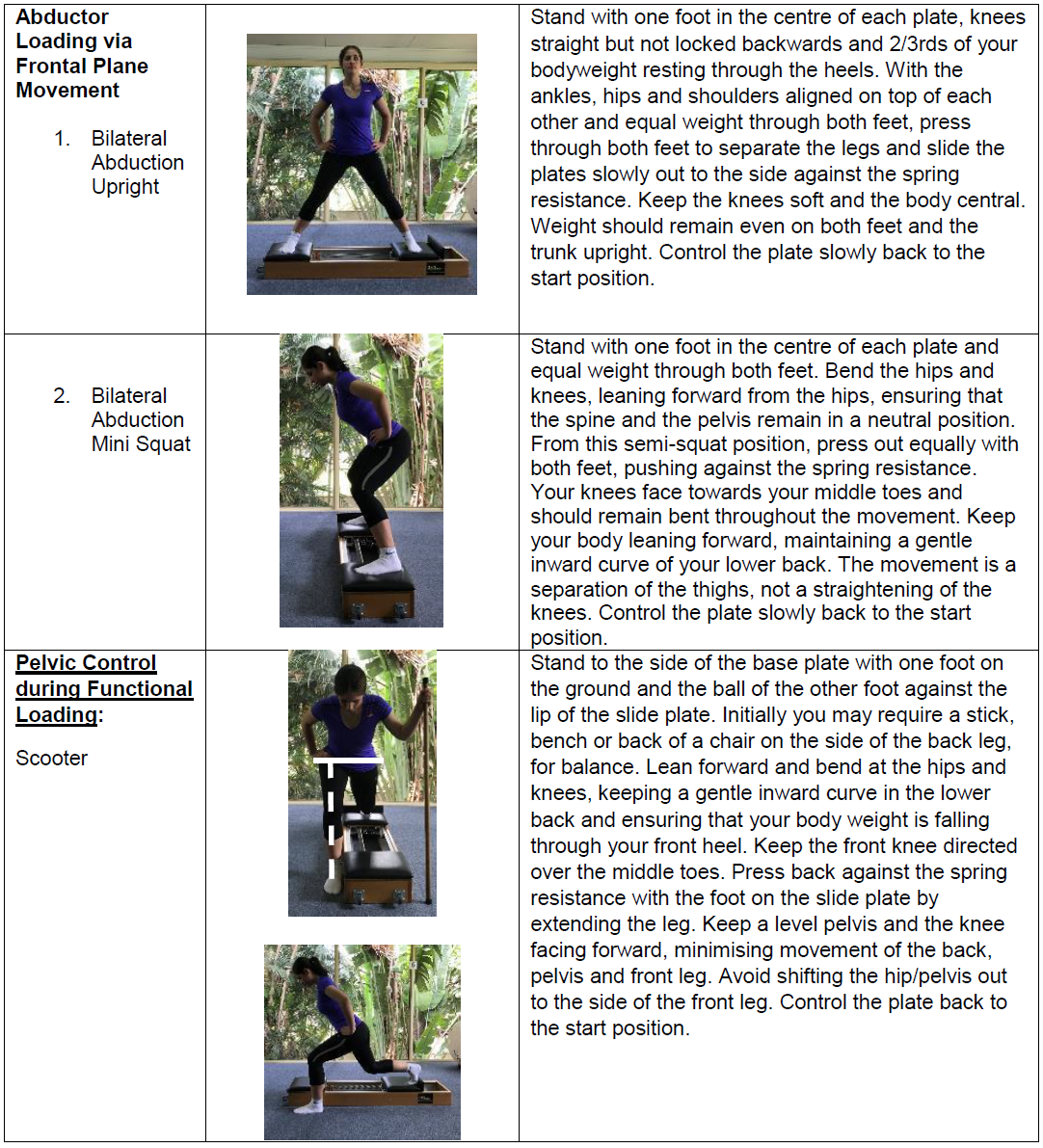
Ganderton et al. (2018) compared the GLoBE programme to a sham exercise programme for management of GTPS. There was no added benefit of either exercise program when added to education but the subjects in the GLoBE exercise group reported a better outcome than the sham exercise group. Ganderton et al. reported that this likely indicates sub-groups exist in GTPS[28]. The GLoBE exercise programme is outlined below in Table 3.
| Table 3: GLoBE exercise phases[28][42] | ||
|---|---|---|
| Phase | Exercise | Description |
| 1 | Isometric hip hitch | Start with hip hitch with wall support. Progress to hip hitch without wall support, but with arm support. The unaffected limb should be hitched. Both knees should be kept straight. Begin with 2 x 15 second holds and progress to 4 x 40 second holds |
| Wall squats on both legs | Double leg quarter wall squats with hips in 20° external rotation. Progress to half wall squat. Begin with 1 set of 5 repetitions and increase to 4 sets of 5 repetitions. | |
| Calf raises on both feet | Calf raises on both feet with arm support. Begin with 2 x 5 repetitions and increase to 2 x 10 repetitions. | |
| 2 | Hip hitch with toe taps | Hip Hitch with toe taps onto 7.5cm step. Progress to a 10cm step. Begin with 2 x 5 repetitions and increase to 2 x 15 repetitions. |
| Sit to stand | Sit to stand off a standard chair with arms crossed over the chest. Gradually decrease the height of the chair as tolerated. Begin with 1 x 5 repetitions and increase to 2 x 10 repetitions. | |
| Calf raises with toe tap | Sustained calf raise with toe taps on the spot. Use a wall or chair for balance. Start with 2 x 5 repetitions and increase to 2 x 10 repetitions. | |
| 3 | Hip hitch with hip swing | The affected limb is the stance limb. Perform a sustained hip hitch on the affected limb. Complete hip swings 10° forwards and backwards with the contralateral leg. Begin with swings and then increase to 2 x 15 contralateral hip swings. |
| Sit to stand with split stance | Sit to stand off a standard chair with affected leg placed slightly behind the unaffected leg. Start with 2 x 5 repetitions and increase to 4 x 5 repetitions. | |
| Single leg calf raises | Single leg calf raise with arm support. Start with 2 x 5 repetitions and increase to 4 x 5 repetitions. | |
| 4 | Single leg wall squat | 2 x 5 repetitions |
| Step ups | 2 x 10 repetitions. | |
| Single leg calf raises with arm support | 2 x 15 repetitions. | |
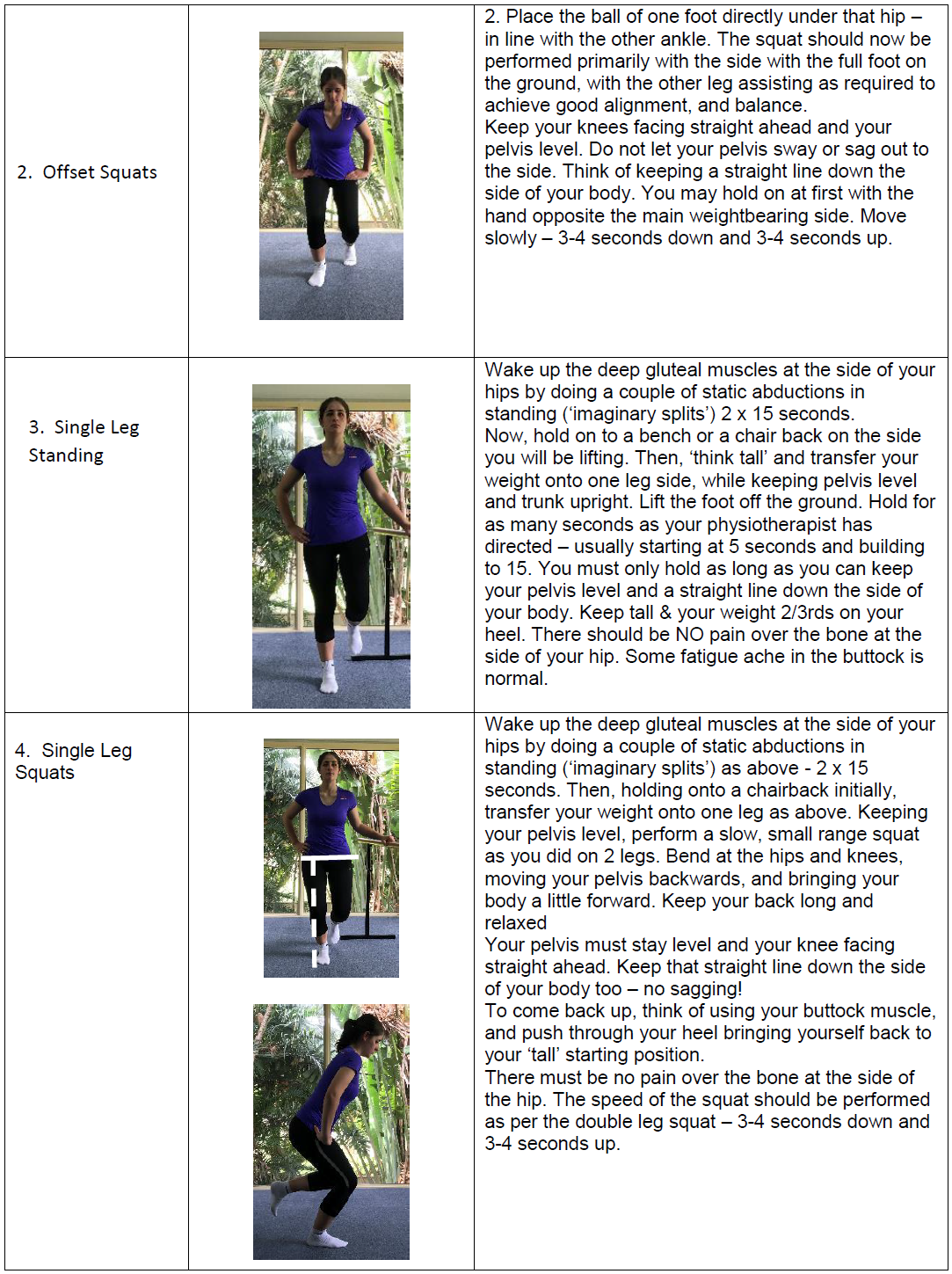
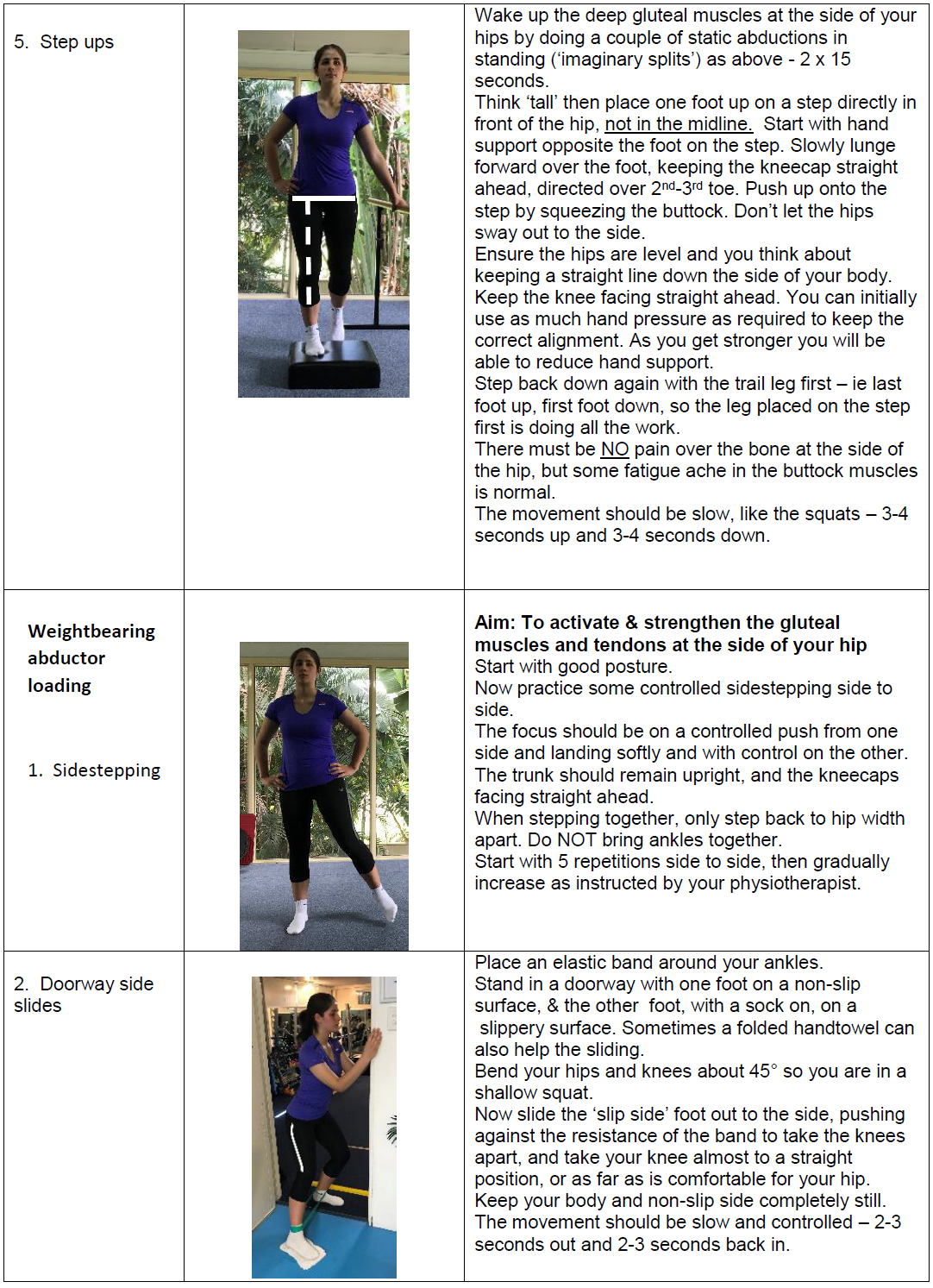
Mellor et al. (2018) found exercise plus education to be superior to corticosteroid injections and it remained that way at 52 weeks follow-up[43]. This study showed that exercise plus education was even superior to corticosteroid injections in the first 8 weeks, showing that exercise plus education is effective from early on[43]. They made use of a progressive exercise programme that can be found below in the LEAP trial images p1 to p5.[43].
It is clear that strengthening of the hip abductors is an important component of GTPS management, but what exercise is most effective? Firstly, all prescribed exercise must patient-specific and should be determined by the phase of tissue healing, the patient’s tolerance of the exercise and/or the principles of progressive loading[44]. A study published in 2017 assessed various exercises to determine their degree of GMed activation[44]. A short summary of the results is found below in Table 4.
It is worth mentioning that the popular clam exercise was found by to produce negligible activation in the GMed (particularly the anterior and middle portions) by Ganderton et al. (2017)[45]. In this same study, the hip hitch was found to best activate the GMed and GMin[45].
| Table 4: GMed exercises in order of degree of activation[44] | |||
| Low | Moderate | Moderate to High | High to very High |
|
|
|
|
| Abbreviations: NWB, non-weight-bearing; WB, weight-bearing; IR, internal rotation | |||
Surgical Management[edit | edit source]
Bursectomy
This intervention used to be carried out by open surgery, but now it is most commonly done arthroscopically. Fox et al. (2002) found that arthroscopic trochanteric bursectomy is a minimally invasive technique, that appears to be a safe and an effective approach for managing GTPS[46][47]. In a more recent study by Mitchell et al. (2016) successful management of GTPS was achieved with endoscopic arthroscopic bursectomy together with an iliotibial band release[48].
Iliotibial band surgical options
Surgery is not the first choice of management but in cases where functional impairment is present, surgery can be done. There are three options in these patients: iliotibial tract (ITT) release, ITT bursectomy and lateral synovial recess resection[17]. Another study released in 2012 also found surgical ITT release and trochanteric bursectomy to be an effective and safe treatment[49].
Reduction-osteotomy of the greater trochanter
This is an option should bursectomy and ITT release fail. It requires a large incision of 7 to 10 cm[49] and is the procedure with the highest rate of complications[37]. During the procedure conducted by Govaert et al. (2003), a 5 to 10mm slice of bone was removed deep to the greater trochanter and continued distally beyond the vastus ridge. The GMed was left attached. Fixation with two lag screws was done once transfer of the medial and distal trochanter was completed[11].
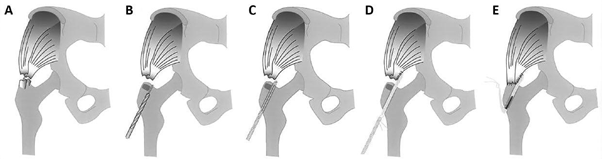
Reconstruction/Repair of the abductor tendon
When MRI and clinical findings are consistent with a tendon tear, surgical repair is an option. A retrospective study by Davies et al. (2013) revealed that in most cases, substantial improvement in abductor tendon strength and clinical performance occurred. A study published in 2016 found that a double-row endoscopic technique allowed the surgeon to visualize, debride and repair the tendon effectively[5]. There have also been cases where a GMax tendon transfer has been done to manage the tear[50]. A very recent study (2019) found that reinforcing the repair with an allograft increased the structural strength of the repaired tendon, preventing suture pullout. The authors also reported that this approach allowed for better graft compression to the bone, potentially allowing for an increased healing rate[50].
Ebert et al. (2018) published a postoperative management protocol for patients with abductor repairs[41]. This protocol can be found in Table 2.
| Table 2 | ||
|---|---|---|
| Phase | Postoperative goals | Patient education and exercise prescription |
| Phase 1
(1-2 weeks) |
1.Reduce postoperative pain/oedema.
2. Avoid excessive WB (>20% BW). 3. Avoid provocative postures and positions that may adversely stretch/load the repair site. 4. Maintain lower limb joint |
• Educate on strategies to reduce pain/inflammation.
• Education and practice in proficient heel-toe WB ambulation (≤20% BW), using 2 crutches. • Education on provocative postures and positions that may adversely stretch/load the repair site. • Passive and active-assisted hip ROM exercises within a pain-free ROM (avoidance of hip flexion >90°, internal rotation beyond neutral and/or hip adduction beyond the midline). • Active ankle dorsi- and plantar-flexion exercises. mobility, muscle tone and circulation. • Isometric contraction of the quadriceps, hamstrings, adductor and gluteal musculature. |
| Phase 2
(2-4 weeks) |
1. Pain and oedema well managed. 2. Proficient heel-toe gait at 50% BW with 1-2 crutches.
3. Proficiency in undertaking home-exercise programme. |
• Progress from ≤20% BW (1-2 weeks) to 50% BW (4 weeks), using 1-2 forearm crutches.
• Education on quality of gait, particularly with the progression toward a single forearm crutch. • Introduce gentle stretching of the hip flexors. • Introduce additional home-based exercises, such as: knee extensions, prone knee flexion, multi-plane isometric hip adduction, bilateral supine bridging, resisted knee flexion, heel raises and standing hip extension. • Introduce hydrotherapy, including: deep water walking (forwards, backwards,sideways), heel raises, mini squats, straight leg hip flexion and extension, cycling, scissor kicks. |
| Phase 3
(4-8 weeks) |
1.Pain-free full WB gait by 8 weeks (1 crutch permitted for protection, stability and/or safety as required.
2. Pain-free during low demand daily tasks. 3. Proficiency in performing all new homebased exercises. 4. Near full and comfortable hip ROM (≥75% hip ROM in all planes compared to the contralateral hip). |
• Progress from 50% BW (4 weeks) to full WB as tolerated from 6 weeks, using 1 forearm crutch as required.
• Progress toward full pain-free passive and active hip ROM. • Education on quality gait required. • Increase demand of home based exercises, including: isometric and isotonic external hip rotation (using theraband), clam exercises, supine hip flexion, straight leg raises, bilateral supine bridging (with added theraband resistance) and standing hip abduction (without resistance). • Introduce stationary cycling (week 4-6) and gentle freestyle swimming for hip ROM and/or cardiovascular fitness. • Hydrotherapy: add shallow water walking (waist depth), straight leg hip abduction and circumduction, deep squats, step ups/downs, lunges, single leg balance and proprioception exercises. • Gentle remedial massage and soft tissue mobilisation. |
| Phase 4
(8-12 weeks) |
1. Pain-free and full active hip ROM (≥90% hip ROM in all planes compared to contralateral hip).
2. Pain-free 6-minute walk test without the use of walking aids (gait speed patient dependent). 3. Ability to single leg stand for 15-30 seconds, with VAS ≤3/10. 4. Proficiency in performing home- and clinicbased exercises for the independent continuation of post-discharge rehabilitation. |
• Full WB as tolerated, crutch/cane for stability as required.
• Education on quality gait and undertaking functional activities (i.e.risingfrom sitting) required. • Increase demand of home based exercises, including: trunk flexion and core stability activities, prone hip extension, quadruped exercises with hip extension, standing resisted (theraband) hip extension and abduction, side-lying hip abduction. • Introduce WB functional activities as permitted (week 11-12), including: bilateral wall and free-standing squats (with assistance if required), single leg stance balance and weight shift activities, proprioceptive WB exercises. |
| Phase 5
(3-6 months) |
1. Normal, pain-free and unaided gait.
2. Hip abductor strength ≤75% on MMT and/or HHD, compared with the contra-lateral limb. 3. Comfort in ambulating stairs (ascent and descent) and gradients. 4. Return to work (dependent on occupational demands). 5. Proficiency in performing all full WB strengthening, functional and proprioception activities. |
•Education and exercises pertinent to the training of daily activities for the individual patient is required.
• End range and multi-plane stretching and soft tissue therapy of surrounding hip musculature, including: gluteus medius, minimus, iliotibial band and tensor fascia lata. •Increase demand of home based exercises, including: single limb supine bridge exercise, side and prone bridging, pelvic drops and lateral band walks. • Increase demand of WB functional activities as required, including: single limb squat, lunge, single leg balance and stepping activities. • Outdoor road cycling is permitted, while rowing ergometry and elliptical trainers can be introduced. • Please note: graduation in WB activities should be based upon the assumed healing and maturation of the surgical repair, as well as the individuals’ surgical details, lower limb strength/function and tolerance to exercises (pain and control). |
| Phase 6
(6 months onwards) |
1. Ability to tolerate pain-free walking distances of any length/duration.
2. Hip abductor strength ≥90% on MMT and/or HHD, compared with the contra-lateral limb. 3. Ability to perform all activities of daily living pain-free. 4. Ability to effectively negotiate uneven terrain and soft sand. 5. Return to pre-operative low-impact recreational activities and/or sport as required. |
•Ongoing education may be required in undertaking specific work, recreational and/or sporting activities, with particular reference to optimal ergonomic and/or technique modification to avoid provocative positions and/or movements that could be implicated in a recurrence of symptoms.
• Exercises employed should begin to replicate what is required for the patient’s individual activity goals, which may include sport specific activities. |
| BW = body weight; HHD = hand held dynamometry; MMT = manual muscle testing; ROM = range of motion; VAS = visual analogue pain scale; WB = weight-bearing. | ||
| Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license. Ebert JR, Bucher TA, Mullan CJ, Janes GC. Clinical and functional outcomes after augmented hip abductor tendon repair. HIP International. DOI: 10.5301/hipint.5000525. 2018, Vol. 28(1) 74–83. Published online: September 21, 2017. SAGE original pubisher. https://journals.sagepub.com/doi/pdf/10.5301/hipint.5000525 | ||
references[edit | edit source]
- ↑ 1.0 1.1 1.2 Long SS, Surrey DE, Nazarian LN. Sonography of greater trochanteric pain syndrome and the rarity of primary bursitis. American Journal of Roentgenology. 2013 Nov;201(5):1083-6.
- ↑ 2.00 2.01 2.02 2.03 2.04 2.05 2.06 2.07 2.08 2.09 2.10 2.11 2.12 2.13 2.14 2.15 Speers CJB, Bhogal GS. Greater trochanteric pain syndrome: a review of diagnosis and management in general practice. British Journal of General Practice. 2017;67:479-480.
- ↑ 3.0 3.1 3.2 3.3 3.4 Jacobson JA, Yablon CM, Henning PT, Kazmers FS, Urquhart A, Hallstrom B, Bedi A, Parameswaran A. Greater Trochanteric Pain Syndrome: Percutaneous Tendon Fenestration Versus Platelet-Rich Plasma Injection for Treatment of Gluteal Tendinosis. J Ultrasound Med. 2016;35:2413–2420.
- ↑ 4.0 4.1 Khoury AN, Brooke K, Helal A, Bishop B, Erikson L, Palmer IJ, Martin HD. Proximal iliotibial band thickness as a cause for recalcitrant greater trochanteric pain syndrome. Journal of Hip Preservation Surgery. 2018;5(3):296–300.
- ↑ 5.0 5.1 5.2 5.3 5.4 5.5 5.6 5.7 5.8 Domb BG, Carreira DS. Endoscopic Repair of Full-Thickness Gluteus Medius Tears. Arthroscopy Techniques. 2013;2(2):e77-e81
- ↑ 6.0 6.1 6.2 6.3 6.4 6.5 6.6 6.7 6.8 6.9 Reid D. The management of greater trochanteric pain syndrome: A systematic literature review. Journal of Orthopaedics. 2016;13:15-28.
- ↑ 7.0 7.1 7.2 7.3 7.4 7.5 7.6 Fearon AM, Scarvell JM, Neeman T, Cook JL, Cormick W, Smith PN. Greater trochanteric pain syndrome: Defining the clinical syndrome. Br J Sports Med. 2012;0:1–5.
- ↑ 8.0 8.1 Ali M, Oderuth E, Atchia I, Malviya A. The use of platelet-rich plasma in the treatment of greater trochanteric pain syndrome: a systematic literature review. Journal of Hip Preservation Surgery. 2018;5(3):209–219
- ↑ 9.00 9.01 9.02 9.03 9.04 9.05 9.06 9.07 9.08 9.09 9.10 9.11 9.12 9.13 9.14 9.15 9.16 9.17 9.18 9.19 9.20 9.21 9.22 9.23 9.24 9.25 9.26 9.27 9.28 9.29 9.30 9.31 9.32 9.33 9.34 9.35 9.36 Grimaldi A, Fearon A. Gluteal Tendinopathy: Integrating Pathomechanics and Clinical Features in Its Management. JOSPT. 2015;45(11):910-924.
- ↑ 10.0 10.1 10.2 10.3 Klauser AS, Martinoli C, Tagliafico A, Bellmann-Weiler R, Feuchtner GM, Wick M, Jaschke WR. Greater Trochanteric Pain Syndrome. Seminars in Musculoskeletal Radiology. 2013;17(1):43-48.
- ↑ 11.00 11.01 11.02 11.03 11.04 11.05 11.06 11.07 11.08 11.09 11.10 11.11 11.12 Grimaldi A, Mellor R, Hodges P, Bennell K, Wajswelner H, Vicenzino B. Gluteal Tendinopathy: A Review of Mechanisms, Assessment and Management. Sports Med. 2015;45(8):1107-1119.
- ↑ Lievense A, Bierma-Zeinstra S, Schouten B, Bohnen A, Verhaar J, Koes B. Prognosis of trochanteric pain in primary care. Br J Gen Pract. 2005 Mar 1;55(512):199-204.
- ↑ 13.0 13.1 13.2 13.3 Nissen MJ, Brulhart L, Faundez A, Finckh A, Courvoisier DS, Genevay S. Glucocorticoid injections for greater trochanteric pain syndrome: a randomised double-blind placebo-controlled (GLUTEAL) trial. Clinical Rheumatology. 2018;38(3):647-655.
- ↑ 14.00 14.01 14.02 14.03 14.04 14.05 14.06 14.07 14.08 14.09 14.10 14.11 14.12 14.13 14.14 14.15 14.16 14.17 14.18 14.19 14.20 14.21 14.22 14.23 14.24 14.25 14.26 14.27 Lin CY, Fredericson M. Greater Trochanteric Pain Syndrome: An Update on Diagnosis and Management. Curr Phys Med Rehabil Rep. 2015;3(1);60-66.
- ↑ Bunker TD, Esler CAN, Leach WJ. Rotator-cuff tear of the hip. J Bone Joint Surg. 1997;79-B:618-620.
- ↑ Woodley SJ, Mercer SR, Nicholson HD. Morphology of the Bursae Associated with the Greater Trochanter of the Femur. J Bone Joint Surg Am. 2008;90:284-94.
- ↑ 17.0 17.1 17.2 Williams BS, Cohen SP. Greater Trochanteric Pain Syndrome: A Review of Anatomy, Diagnosis and Treatment. International Anesthesia Research Society. 2009;108(5):1662-1670.
- ↑ 18.0 18.1 Genth B. Von Düring M, Von Engelhardt LV, Ludwig J, Teske W, Von Schulze-Pellengahr C. Analysis of the sensory innervations of the greater trochanter for improving the treatment of greater trochanteric pain syndrome. Clin Anat. 2012 Nov;25(8):1080-6.
- ↑ Segal NA, Felson DT, Torner JC, Zhu Y, Curtis JR, Niu J, Nevitt MC, Group MO. Greater trochanteric pain syndrome: epidemiology and associated factors. Archives of physical medicine and rehabilitation. 2007 Aug 1;88(8):988-92.
- ↑ 20.0 20.1 Shbeeb MI, Matteson EL. Trochanteric bursitis (greater trochanter pain syndrome). InMayo Clinic Proceedings 1996 Jun 1 (Vol. 71, No. 6, pp. 565-569). Elsevier.
- ↑ 21.0 21.1 21.2 Louw M, Deary C. The biomechanical variables involved in the aetiology of iliotibial band syndrome in distance runners–A systematic review of the literature. Physical Therapy in sport. 2014 Feb 1;15(1):64-75.
- ↑ Fernandez E, Gastaldi P. Hip pain from the orthopeadic point of view. European journal of radiology. 2012 Dec 1;81(12):3737-9.
- ↑ Fearon AM, Twin J, Dahlstrom JE, Cook JL, Cormick W, Smith PN, Scott A. Increased substance P expression in the trochanteric bursa of patients with greater trochanteric pain syndrome. Rheumatol Int. 2014; 34(10):1441–1448.
- ↑ 24.0 24.1 24.2 24.3 24.4 24.5 24.6 24.7 Domb BG, Nasser RM, Botser IB. Partial-thickness tears of the gluteus medius: rationale and technique for trans-tendinous endoscopic repair. Arthroscopy: The Journal of Arthroscopic & Related Surgery. 2010 Dec 1;26(12):1697-705.
- ↑ 25.0 25.1 25.2 25.3 25.4 Lewis CL. Extra-articular snapping hip: a literature review. Sports health. 2010 May;2(3):186-90.
- ↑ 26.0 26.1 26.2 Yen YM, Lewis CL, Kim YJ. Understanding and treating the snapping hip. Sports medicine and arthroscopy review. 2015 Dec;23(4):194.
- ↑ 27.0 27.1 McEvoy, J.R., Lee, K.S., Blankenbaker, D.G., Rio, A.M.D. and Keene, J.S., 2013. Ultrasound-guided corticosteroid injections for treatment of greater trochanteric pain syndrome: greater trochanter bursa versus subgluteus medius bursa. American Journal of Roentgenology, 201(2), pp.W313-W317.
- ↑ 28.00 28.01 28.02 28.03 28.04 28.05 28.06 28.07 28.08 28.09 28.10 28.11 28.12 28.13 Ganderton C, Semciw A, Cook J, Moreira E, Pizzari T. Gluteal loading versus sham exercises to improve pain and dysfunction in postmenopausal women with greater trochanteric pain syndrome: a randomized controlled trial. Journal of Women's Health. 2018 Jun 1;27(6):815-29.
- ↑ 29.0 29.1 29.2 29.3 Fearon A, Neeman T, Smith P, Scarvell J, Cook J. Pain, not structural impairments may explain activity limitations in people with gluteal tendinopathy or hip osteoarthritis: a cross sectional study. Gait & posture. 2017 Feb 1;52:237-43.
- ↑ 30.0 30.1 30.2 Klontzas ME, Karantanas AH. Greater trochanter pain syndrome: a descriptive MR imaging study. European journal of radiology. 2014 Oct 1;83(10):1850-5.
- ↑ Via AG, Fioruzzi A, Randelli F. Diagnosis and Management of Snapping Hip Syndrome: A Comprehensive Review of Literature. Rheumatology (Sunnyvale). 2017;7(228):2161-1149.
- ↑ 32.0 32.1 32.2 32.3 32.4 Cook J. Lower Limb Tendinopathy. Lower Limb Tendinopathy course; 2020 Mar 9-10; Cape Town, South Africa. P1-102.
- ↑ Fearon AM, Ganderton C, Scarvell JM, Smith PN, Neeman T, Nash C, Cook JL. Development and validation of a VISA tendinopathy questionnaire for greater trochanteric pain syndrome, the VISA-G. Manual therapy. 2015 Dec 1;20(6):805-13.
- ↑ 34.0 34.1 34.2 Ganderton C, Semciw A, Cook J, Pizzari T. Demystifying the clinical diagnosis of greater trochanteric pain syndrome in women. Journal of Women's Health. 2017 Jun 1;26(6):633-43.
- ↑ Dubin J. Evidence Based Treatment for Iliotibial Band Friction Syndrome: Review of Literature. BioMechanics 2005.
- ↑ 36.0 36.1 Ortiz-Declet V, Chen AW, Maldonado DR, Yuen LC, Mu B, Domb BG. Diagnostic accuracy of a new clinical test (resisted internal rotation) for detection of gluteus medius tears. Journal of Hip Preservation Surgery. 2019 Nov 14.
- ↑ 37.0 37.1 37.2 Koulischer S, Callewier A, Zorman D. Management of greater trochanteric pain syndrome: a systematic review. Acta Orthop Belg. 2017 Jun;83:205-14.
- ↑ Brennan KL, Allen BC, Maldonado YM. Dry Needling Versus Cortisone Injection in the Treatment of Greater Trochanteric Pain Syndrome: A Noninferiority Randomized Clinical Trial. Journal of orthopaedic & sports physical therapy. 2017;47(4):232-239.
- ↑ 39.0 39.1 39.2 39.3 39.4 Wyss J, Patel A. Therapeutic Programs for Musculoskeletal Disorders. United States of America: Bradford & Bigelow Printing, 2013.
- ↑ 40.0 40.1 Rio E, Kidgell D, Purdam C, Gaida J, Moseley GL, Pearce AJ, Cook J.Isometric exercise induces analgesia and reduces inhibition in patellar tendinopathy. Br J Sports Med. 2015;49:1277–1283.
- ↑ 41.0 41.1 Ebert JR, Bucher TA, Mullan CJ, Janes GC. Clinical and functional outcomes after augmented hip abductor tendon repair. Hip International. 2018 Jan;28(1):74-83.
- ↑ Ausralian New Zealand Clinical Trials Regisry. Available from: https://www.anzctr.org.au/Trial/Registration/TrialReview.aspx?id=366865&isReview=true. Accessed 14 March 2020.
- ↑ 43.0 43.1 43.2 Mellor R, Bennell K, Grimaldi A, Nicolson P, Kasza J, Hodges P, Wajswelner H, Vicenzino B. Education plus exercise versus corticosteroid injection use versus a wait and see approach on global outcome and pain from gluteal tendinopathy: prospective, single blinded, randomised clinical trial. BMJ. 2018;360:1-9.
- ↑ 44.0 44.1 44.2 Ebert JR, Edwards PK, Fick DP, Janes GC. http://www.scielo.br/pdf/motriz/v25n3/1980-6574-motriz-25-03-e101983.pdf. Journal of Sport Rehabilitation. 2017;26:418 -436.
- ↑ 45.0 45.1 Ganderton C, Pizzari T, Cook J, Semciw A. Gluteus Minimus and Gluteus Medius Muscle Activity During Common Rehabilitation Exercises in Healthy Postmenopausal Women. JOSPT. 2017;47(12):914-922.
- ↑ Bird PA, Oakley SP, Shnier R, Kirkham BW. Prospective evaluation of magnetic resonance imaging and physical examination findings in patients with greater trochanteric pain syndrome. Arthritis & Rheumatism: Official Journal of the American College of Rheumatology. 2001 Sep;44(9):2138-45.
- ↑ Fox JL. The role of arthroscopic bursectomy in the treatment of trochanteric bursitis. Arthroscopy: The Journal of Arthroscopic & Related Surgery. 2002 Sep 1;18(7):1-4.
- ↑ Mitchell JJ, Chahla J, Vap AR, Menge TJ, Soares E, Frank JM, Dean CS, Philippon MJ. Endoscopic trochanteric bursectomy and iliotibial band release for persistent trochanteric bursitis. Arthroscopy techniques. 2016 Oct 1;5(5):e1185-9.
- ↑ 49.0 49.1 49.2 Govaert LH, van Dijk CN, Zeegers AV, Albers GH. Endoscopic bursectomy and iliotibial tract release as a treatment for refractory greater trochanteric pain syndrome: a new endoscopic approach with early results. Arthroscopy techniques. 2012 Dec 1;1(2):e161-4.
- ↑ 50.0 50.1 Suppauksorn S, Nwachukwu BU, Beck EC, Okoroha KR, Nho SJ. Superior Gluteal Reconstruction for Severe Hip Abductor Deficiency. Arthroscopy Techniques. 2019 Oct 1;8(10):e1255-61.