Gluteal Fibrosis
Original Editor - User Name
Top Contributors - Khloud Shreif
This article or area is currently under construction and may only be partially complete. Please come back soon to see the finished work!
Clinically Relevant Anatomy[edit | edit source]
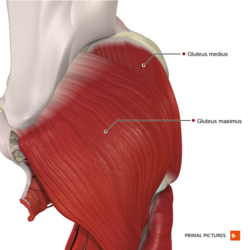
Gluteal muscles/ buttock muscles are muscles at the back of the thigh and formed of three layers; gluteus maximus, the superficial layer and the largest muscle, it is important as one of hip extensors and to maintain erect posture. Gluteus medius the middle layer on the lateral aspect of the pelvis below the iliac crest and it is important as a main hip abductor muscle. Gluteus minimus the deep layer and the smallest one of the gluteal muscles and helps with hip abduction and internal rotation.
Mechanism of Injury / Pathological Process[edit | edit source]
Gluteal fibrosis/ gluteal contracture was described early in 1970s, defined as fibrotic infiltration changes of gluteal muscles, most commonly associated with intramuscular injections that may cause functional limitation of hip joint movements[1], patients with gluteal contracture will present with hip abducted and externally rotated[2]. Acquired gluteal fibrosis/ contracture is the most common type, the prevalence increase when the injection was in younger ages.
The mechanism / pathophysiology of GF/ GMC seems to have more than one hypothesis; congenital, idiopathic that usually associated with some diseases such as cerebral palsy, brain atrophy, poliomyelitis[3], or acquired that is the most common type and happen because of intramuscular gluteal injection it known as “Injection-Contracture”, or injuries around the hip[2].
Classifications of GMC[edit | edit source]
Prevalence[edit | edit source]
GF/ GMC reported worldwide we can find it in Turkey, Iraq, England, Spain, Germany, Italy, Poland, Belgium, Uganda, the U.S, China, South Korea, India[4], but in china the incidence rate of childhood range from 1–2.5% from overall childhood and that a high percentage. In Africa the injection of quinine (used to treat malaria) intramuscular is the reported cause for GF[5].
Clinical Presentation[edit | edit source]
- Toe- out gait.
- Awkward gait be more obvious with running.
- Positive ober's test.
- Excessive hip external rotation and abduction when the hip is flexed.
- Frog leg posture at squatting or sitting.
- Difficulty in crossing legs.
- leg length discrepancy, the affected leg will be the longer it may be due to pelvic obliquity or prolonged traction of contracture bands.
- Palpable contracture bands.
- Skin dimples over the buttocks[4] or cone shaped buttocks[2].
- Usually there may be snapping sound at squatting because of the gliding movement of fibrotic bands over the greater trochanter[6].
Diagnostic Procedures[edit | edit source]
At first we need to exclude first poliomyelitis and other diseases; cerebral palsy, neuromuscular disorders, or other hip abnormalities are important to be ruled out through imaging and clinical examination.
Diagnostic ultrasound: it will show stripes of condensed sound waves (hyperechoic muscles) it had 88.9%sensitivity and 83.3% for specificity.
Magnetic Resonance Imaging MRI: it will show intramuscular atrophic changes and fibrotic cord that will be more common in the upper-third of the gluteus maximus, the fibrotic change may extend to the muscle's tendon, groove depression at the musculotendinous junction and external rotation of the proximal femur because of medial retraction of the muscle[7].
Radiography X- ray: early stage there will be no obvious changes but, with disease progression there will be iliac hyperdense line over the posterior iliac spine, pelvic obliquity, or coxa valga are other signs may be visible on x ray[2].
Outcome Measures[edit | edit source]
add links to outcome measures here (see Outcome Measures Database)
Management / Interventions[edit | edit source]
add text here relating to management approaches to the condition
Differential Diagnosis[edit | edit source]
add text here relating to the differential diagnosis of this condition
References[edit | edit source]
- ↑ Reilly AL, Owori FR, Obaikol R, Asige E, Aluka H, Penny N, Olupot R, Sabatini CS. Surgical release of gluteal fibrosis in children results in sustained benefit at 5-year follow-up. Journal of Pediatric Orthopaedics. 2021 Mar 11;41(3):e240-5.
- ↑ 2.0 2.1 2.2 2.3 Rai S, Meng C, Wang X, Chaudhary N, Jin S, Yang S, Wang H. Gluteal muscle contracture: diagnosis and management options. SICOT-J. 2017;3.
- ↑ Lixihua L, Zhangqing Z, Shengpingquan S, Zhaolei Z, Zhaoli Z, Cuixuee C, Liuxiaoqin L. P1. 43 The clinical and pathological analysis of the uniform type l fiber myopathy with brain atrophy and gluteal muscle contractures. Neuromuscular Disorders. 2010 Oct 1;20(9):613.
- ↑ 4.0 4.1 Alves K, Katz JN, Sabatini CS. Gluteal fibrosis and its surgical treatment. The Journal of Bone and Joint surgery. American Volume. 2019 Feb 20;101(4).
- ↑ Nikolaou S, Asige E, Francis O, Abaikol R. Gluteal fibrosis: A case series in eastern Uganda. Could our malarial treatment be causing long-term disability?. International Journal of Surgery. 2014 Nov 1;12:S64.
- ↑ Lewis CL. Extra-articular snapping hip: a literature review. Sports health. 2010 May;2(3):186-90.
- ↑ Chen CK, Yeh L, Chang WN, Pan HB, Yang CF. MRI diagnosis of contracture of the gluteus maximus muscle. American Journal of Roentgenology. 2006 Aug;187(2):W169-74.