Flexor Tendon Injuries: Difference between revisions
mNo edit summary |
m (small edits) |
||
| Line 2: | Line 2: | ||
== Introduction == | == Introduction == | ||
Flexor tendon injuries are some of the more common injuries, but yet complex injuries managed by hand surgeons. The flexor tendon mechanism plays a key role in the functionality of the hand. Physiotherapists and occupational therapists are often involved | Flexor tendon injuries are some of the more common injuries, but yet complex injuries managed by hand surgeons. The flexor tendon mechanism plays a key role in the functionality of the hand. Physiotherapists and occupational therapists are often involved and play a key role in the post-surgical rehabilitation of flexor tendon repairs. A good understanding of the treatment procedures, healing stages, clinically relevant anatomy and rehabilitation of these injuries is necessary for a satisfactory outcome in the patient with a flexor tendon injury. | ||
The below 8 minute video nicely outlines the key features of flexor [[Tendon Anatomy|tendon]] injuries treatment and | The below 8-minute video nicely outlines the key features of flexor [[Tendon Anatomy|tendon]] injuries treatment and anatomy. | ||
{{#ev:youtube|https://www.youtube.com/watch?v=nrZdYJdrSCo&app=desktop|width}}<ref>J Knight Flexor tendon surgery Available from: https://www.youtube.com/watch?v=nrZdYJdrSCo&app=desktop (last accessed 8.12.2019)</ref> | {{#ev:youtube|https://www.youtube.com/watch?v=nrZdYJdrSCo&app=desktop|width}}<ref>J Knight Flexor tendon surgery Available from: https://www.youtube.com/watch?v=nrZdYJdrSCo&app=desktop (last accessed 8.12.2019)</ref> | ||
== Epidemiology of Flexor Tendon Injuries == | == Epidemiology of Flexor Tendon Injuries == | ||
* Incidence rate of 33.2 injuries per 100 00 person-years<ref name=":3">de Jong JP, Nguyen JT, Sonnema AJ, Nguyen EC, Amadio PC, Moran SL. The incidence of acute traumatic tendon injuries in the hand and wrist: a 10-year population-based study. Clinics in orthopedic surgery. 2014 Jun 1;6(2):196-202.</ref> | * Incidence rate of 33.2 injuries per 100 00 person-years<ref name=":3">de Jong JP, Nguyen JT, Sonnema AJ, Nguyen EC, Amadio PC, Moran SL. The incidence of acute traumatic tendon injuries in the hand and wrist: a 10-year population-based study. Clinics in orthopedic surgery. 2014 Jun 1;6(2):196-202.</ref> | ||
* Highest incidence of injury occurs at 20 -29 years of age, and average age is 35 years<ref name=":3" /> | * Highest incidence of injury occurs at 20 -29 years of age, and the average age is 35 years<ref name=":3" /> | ||
* Higher incidence in males<ref name=":3" /><ref name=":4">Manninen M, Karjalainen T, Määttä J, Flinkkilä T. Epidemiology of flexor tendon injuries of the hand in a Northern Finnish population. Scandinavian journal of surgery. 2017 Sep;106(3):278-82.</ref> | * Higher incidence in males<ref name=":3" /><ref name=":4">Manninen M, Karjalainen T, Määttä J, Flinkkilä T. Epidemiology of flexor tendon injuries of the hand in a Northern Finnish population. Scandinavian journal of surgery. 2017 Sep;106(3):278-82.</ref> | ||
* Significant association between injury and age<ref name=":3" /><ref name=":4" /> | * Significant association between injury and age<ref name=":3" /><ref name=":4" /> | ||
* Incidence is inversely related to age (injuries decrease with increase in age)<ref name=":4" /> | * Incidence is inversely related to age (injuries decrease with increase in age)<ref name=":4" /> | ||
* Extensor tendon injuries occur more frequently than flexor tendon injuries<ref name=":3" /> | * Extensor tendon injuries occur more frequently than flexor tendon injuries<ref name=":3" /> | ||
* Majority of cases involve a single tendon, extensor tendon injuries involves Zone III of the index finger and flexor tendons | * Majority of cases involve a single tendon, extensor tendon injuries involves Zone III of the index finger and flexor tendons involve Zone II of the index finger<ref name=":3" /> | ||
* Common injury in people working in physical construction jobs, using saws, glass or getting metal lacerations<ref name=":3" /><ref name=":4" /> | * Common injury in people working in physical construction jobs, using saws, glass or getting metal lacerations<ref name=":3" /><ref name=":4" /> | ||
* Also common in people working in food preparation with knife injuries<ref name=":3" /><ref name=":4" /> | * Also common in people working in food preparation with knife injuries<ref name=":3" /><ref name=":4" /> | ||
| Line 21: | Line 21: | ||
[[File:Interactive hand - hand - L17F1.jpg|right|frameless|329x329px]] | [[File:Interactive hand - hand - L17F1.jpg|right|frameless|329x329px]] | ||
The tendons that can be involved include: | The tendons that can be involved include: | ||
* Flexor pollicis longus (flexion tip of thumb) | * Flexor pollicis longus (flexion tip of the thumb) | ||
* [[Flexor digitorum longus|Flexor digitorum profundus]] (flexion of the fingers) | * [[Flexor digitorum longus|Flexor digitorum profundus]] (flexion of the fingers) | ||
* [[Flexor Digitorum Superficialis|Flexor digitorum superficialis]] (flexes the middle joint of each finger) | * [[Flexor Digitorum Superficialis|Flexor digitorum superficialis]] (flexes the middle joint of each finger) | ||
| Line 33: | Line 33: | ||
*[[File:Brachioradialis, Grays Anatomy.gif|thumb|463x463px]]lies in the anterior compartment of forearm, deep to [[Pronator Teres|pronator teres]], [[Palmaris Longus|palmaris longus]] and [[Flexor Carpi Ulnaris Muscle|flexors carpi ulnaris]] and [[Flexor Carpi Radialis|radialis]] | *[[File:Brachioradialis, Grays Anatomy.gif|thumb|463x463px]]lies in the anterior compartment of forearm, deep to [[Pronator Teres|pronator teres]], [[Palmaris Longus|palmaris longus]] and [[Flexor Carpi Ulnaris Muscle|flexors carpi ulnaris]] and [[Flexor Carpi Radialis|radialis]] | ||
* superficial to [[Flexor Digitorum Profundus|flexor digitorum profundus]] and flexor pollicis longus | * superficial to [[Flexor Digitorum Profundus|flexor digitorum profundus]] and flexor pollicis longus | ||
* muscle has long linear origin, but considered to arise by two heads | * muscle has a long linear origin, but considered to arise by two heads | ||
* Origin: | * Origin: | ||
** medial/ humeroulnar head: | ** medial/ humeroulnar head: | ||
| Line 51: | Line 51: | ||
*[[File:Flexor digitorum profundus grays anatomy.gif|thumb|445x445px]]lies deep to [[Flexor Digitorum Superficialis|flexor digitorum superficialis]] on medial side of forearm | *[[File:Flexor digitorum profundus grays anatomy.gif|thumb|445x445px]]lies deep to [[Flexor Digitorum Superficialis|flexor digitorum superficialis]] on medial side of forearm | ||
* Origin: | * Origin: | ||
** arises from medial side of the coronoid process of the ulna, the upper three quarters of the anterior and medial surfaces of the ulna, and the medial, middle | ** arises from medial side of the coronoid process of the ulna, the upper three quarters of the anterior and medial surfaces of the ulna, and the medial, middle third of the adjacent interosseus membrane | ||
** also arises from the aponeurosis that attaches the flexor carpi ulnaris to the posterior border of the ulna | ** also arises from the aponeurosis that attaches the flexor carpi ulnaris to the posterior border of the ulna | ||
* part of muscle arising from interosseus membrane forms a separate tendon halfway down the forearm, this passes to the index finger | * part of muscle arising from interosseus membrane forms a separate tendon halfway down the forearm, this passes to the index finger | ||
* remaining tendons formed just proximal to | * remaining tendons formed just proximal to the flexor retinaculum | ||
* separate tendons pass below the flexor retinaculum, lying side by side, deep to the tendons of flexor digitorum superficialis, but in the same synovial sheath | * separate tendons pass below the flexor retinaculum, lying side by side, deep to the tendons of flexor digitorum superficialis, but in the same synovial sheath | ||
* the four tendons pass to their respective fingers in the palm | * the four tendons pass to their respective fingers in the palm | ||
| Line 88: | Line 88: | ||
The tendons of flexor digitorum superficialis provide attachments for the vincula tendinum, which convey blood vessels to the tendon. The flexor tendons are encapsulated in a sheath. The flexor digitorum superficialis and flexor digitorum profundus have two vinicula each.<ref name=":6" /> These tendons are not well-vascularised and there are some avascular areas that receive nutrition by diffusion.<ref name=":7" /> | The tendons of flexor digitorum superficialis provide attachments for the vincula tendinum, which convey blood vessels to the tendon. The flexor tendons are encapsulated in a sheath. The flexor digitorum superficialis and flexor digitorum profundus have two vinicula each.<ref name=":6" /> These tendons are not well-vascularised and there are some avascular areas that receive nutrition by diffusion.<ref name=":7" /> | ||
This mechanisms puts the tendons at risk for adhesions. When adhesions are present, the tendon can not glide freely and this leads to limited range of motion and limited functional capacity.<ref name=":7" /> | This mechanisms puts the tendons at risk for adhesions. When adhesions are present, the tendon can not glide freely and this leads to a limited range of motion and limited functional capacity.<ref name=":7" /> | ||
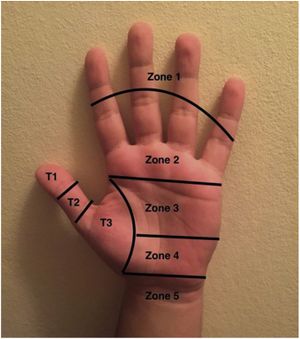
== Tendon Injury Zones == | == Tendon Injury Zones == | ||
| Line 97: | Line 97: | ||
Tendon zones differ for the extensors and the flexors. For the finger flexors the zones are as follows<ref name=":8">Klifto CS, Capo JT, Sapienza A, Yang SS, Paksima N. Flexor tendon injuries. JAAOS-Journal of the American Academy of Orthopaedic Surgeons. 2018 Jan 15;26(2):e26-35.</ref><ref name=":0">Ortho bullets [https://www.orthobullets.com/hand/6031/flexor-tendon-injuries Flexion tendon injuries] Available from: https://www.orthobullets.com/hand/6031/flexor-tendon-injuries (last accessed 8.12.2019)</ref>: | Tendon zones differ for the extensors and the flexors. For the finger flexors the zones are as follows<ref name=":8">Klifto CS, Capo JT, Sapienza A, Yang SS, Paksima N. Flexor tendon injuries. JAAOS-Journal of the American Academy of Orthopaedic Surgeons. 2018 Jan 15;26(2):e26-35.</ref><ref name=":0">Ortho bullets [https://www.orthobullets.com/hand/6031/flexor-tendon-injuries Flexion tendon injuries] Available from: https://www.orthobullets.com/hand/6031/flexor-tendon-injuries (last accessed 8.12.2019)</ref>: | ||
* Zone I - distal to the flexor digitorum superficialis (FDS) | * Zone I - distal to the flexor digitorum superficialis (FDS) | ||
* Zone II - from the FDS insertion | * Zone II - from the FDS insertion to distal portion of the A1 pulley | ||
* Zone III - from the A1 pulley to the transverse carpal ligament | * Zone III - from the A1 pulley to the transverse carpal ligament | ||
* Zone IV - the carpal tunnel | * Zone IV - the carpal tunnel | ||
* Zone V - proximal to carpal tunnel | * Zone V - proximal to carpal tunnel | ||
The thumb has its own zone distrubution | The thumb has its own zone distrubution: | ||
* Zone I - distal to the interphalangeal joint (IP) in the thumb | * Zone I - distal to the interphalangeal joint (IP) in the thumb | ||
* Zone II - between the metacarpophalangeal (MCP) and interphalangeal (IP) joints | * Zone II - between the metacarpophalangeal (MCP) and interphalangeal (IP) joints | ||
| Line 120: | Line 120: | ||
== Diagnostic Procedures == | == Diagnostic Procedures == | ||
* Clinical tests: | * Clinical tests: | ||
** Flexor Digitorum Profundus (FDP) tendon - patient is unable to flex the distal interphalangeal joint (DIP) in isolation<ref name=":12">Khor WS, Langer MF, Wong R, Zhou R, Peck F, Wong JK. Improving outcomes in tendon repair: a critical look at the evidence for flexor tendon repair and rehabilitation. Plastic and reconstructive surgery. 2016 Dec 1;138(6):1045e-58e.</ref> | ** Flexor Digitorum Profundus (FDP) tendon - the patient is unable to flex the distal interphalangeal joint (DIP) in isolation<ref name=":12">Khor WS, Langer MF, Wong R, Zhou R, Peck F, Wong JK. Improving outcomes in tendon repair: a critical look at the evidence for flexor tendon repair and rehabilitation. Plastic and reconstructive surgery. 2016 Dec 1;138(6):1045e-58e.</ref> | ||
** Flexor Digitorum Superficialis (FDS) tendon - isolate the involved/affected finger and ask the patient to flex the proximal interphalangeal joint (PIP)<ref name=":12" /> | ** Flexor Digitorum Superficialis (FDS) tendon - isolate the involved/affected finger and ask the patient to flex the proximal interphalangeal joint (PIP)<ref name=":12" /> | ||
** Flexor Pollicis Longus tendon - flexing the interphalangeal joint (IP) joint of the thumb in isolation<ref name=":12" /> | ** Flexor Pollicis Longus tendon - flexing the interphalangeal joint (IP) joint of the thumb in isolation<ref name=":12" /> | ||
| Line 137: | Line 137: | ||
=== Surgical Repair === | === Surgical Repair === | ||
Surgical repair is needed for cut or ruptured tendons. When a tendon ruptures, the ends separate as a result of the tension in the tendons. Sometimes this separation between the cut or ruptured ends of the tendon can be several centimetres. Surgical repair is necessary in order to regain function that has been lost. The repair may be performed under general anaesthetic or regional anaesthetic (injection of local anaesthetic at the shoulder). During surgery the wound is enlarged so that the cut ends of the tendon can be found and held together with stitches. After the surgery the hand and forearm are immobilised in a splint that is placed over the bandages with the wrist and fingers in a slightly bent position, in order to protect the repair.<ref name=":1">BSHH [https://www.bssh.ac.uk/patients/conditions/26/flexor_tendon_injury#What_is_the_treatment_ Flexor tendon injuries] Available from: https://www.bssh.ac.uk/patients/conditions/26/flexor_tendon_injury#What_is_the_treatment_ (last accessed 8.12.2019)</ref> | Surgical repair is needed for a cut or ruptured tendons. When a tendon ruptures, the ends separate as a result of the tension in the tendons. Sometimes this separation between the cut or ruptured ends of the tendon can be several centimetres. Surgical repair is necessary in order to regain function that has been lost. The repair may be performed under general anaesthetic or regional anaesthetic (injection of local anaesthetic at the shoulder). During surgery, the wound is enlarged so that the cut ends of the tendon can be found and held together with stitches. After the surgery, the hand and forearm are immobilised in a splint that is placed over the bandages with the wrist and fingers in a slightly bent position, in order to protect the repair.<ref name=":1">BSHH [https://www.bssh.ac.uk/patients/conditions/26/flexor_tendon_injury#What_is_the_treatment_ Flexor tendon injuries] Available from: https://www.bssh.ac.uk/patients/conditions/26/flexor_tendon_injury#What_is_the_treatment_ (last accessed 8.12.2019)</ref> | ||
The tendon repair is a surgeon-dependant process and surgeons will decide on the most appropriate technique for the specific tendon repair. Common repairs are four-strand or six-strand repairs. | The tendon repair is a surgeon-dependant process and surgeons will decide on the most appropriate technique for the specific tendon repair. Common repairs are four-strand or six-strand repairs. | ||
=== Post-Surgical Tendon Healing === | === Post-Surgical Tendon Healing === | ||
The healing stages of tendons | The healing stages of tendons include three phases<ref name=":2">Klifto CS, Bookman J, Paksima N. Postsurgical Rehabilitation of Flexor Tendon Injuries. The Journal of hand surgery. 2019 Aug 1;44(8):680-6.</ref><ref>Legrand A, Kaufman Y, Long C, Fox PM. Molecular biology of flexor tendon healing in relation to reduction of tendon adhesions. The Journal of hand surgery. 2017 Sep 1;42(9):722-6.</ref>: | ||
==== Inflammatory phase ==== | ==== Inflammatory phase ==== | ||
* the first phase | * the first phase | ||
* lasts from day one to day seven post-operatively | * lasts from day one to day seven post-operatively | ||
* in this stage fibroblasts produce type III collagen and macrophages help initiate healing and remodelling | * in this stage, fibroblasts produce type III collagen and macrophages help initiate healing and remodelling | ||
==== Proliferative phase ==== | ==== Proliferative phase ==== | ||
| Line 165: | Line 165: | ||
=== Wound and Scar Management === | === Wound and Scar Management === | ||
After surgery wound management is the first step to address. The post-surgical wound may be dressed with a basic silicone dressing (products such as Mepitel may be used). The finger is wrapped with | After surgery wound management is the first step to address. The post-surgical wound may be dressed with a basic silicone dressing (products such as Mepitel may be used). The finger is wrapped with breathable handy gauze material. Other products that therapists may use include Coban, but a good, comfortable, clean and a dry dressing is acceptable as well. | ||
Compression bandaging is used to control oedema. | Compression bandaging is used to control oedema. | ||
Once the wound is healed, scar management can commence. Silicone gel sheeting can be used on the scar or paper tapes or products for scar management such as Fixomull. Scar | Once the wound is healed, scar management can commence. Silicone gel sheeting can be used on the scar or paper tapes or products for scar management such as Fixomull. Scar massage can be done during therapy sessions and at home to prevent adhesions.<ref name=":7" /> | ||
=== Patient Education === | === Patient Education === | ||
| Line 176: | Line 176: | ||
* The wound needs to be kept clean and dry. | * The wound needs to be kept clean and dry. | ||
* The splint needs to stay on 24 hours a day, 7 days a week. | * The splint needs to stay on 24 hours a day, 7 days a week. | ||
** If the splint does need to come off, patient needs to be educated about safe hand positioning. | ** If the splint does need to come off, the patient needs to be educated about safe hand positioning. | ||
** For a flexor injury, the patient needs to keep the fingers cupped with the wrist in neutral if the splint is off. | ** For a flexor injury, the patient needs to keep the fingers cupped with the wrist in neutral if the splint is off. | ||
** This position does not put any stretch or tension on the tendons. | ** This position does not put any stretch or tension on the tendons. | ||
| Line 188: | Line 188: | ||
** Zone I, II and III injuries of the flexor digitorum profundus and/or the flexor digitorum superficialis | ** Zone I, II and III injuries of the flexor digitorum profundus and/or the flexor digitorum superficialis | ||
** This promotes the arc of flexion to be activated by the long flexors, rather than the intrinsics<ref name=":13">Seaward JR, Peck F, Lees VC. Impact of Long Flexor Versus Intrinsic Dominance in the Generation of Arc of Finger Flexion. Hand. 2016 Sep;11(3):364-7.</ref> | ** This promotes the arc of flexion to be activated by the long flexors, rather than the intrinsics<ref name=":13">Seaward JR, Peck F, Lees VC. Impact of Long Flexor Versus Intrinsic Dominance in the Generation of Arc of Finger Flexion. Hand. 2016 Sep;11(3):364-7.</ref> | ||
** It allows differential glide between the FDP and FDS tendon, as flexion is | ** It allows differential glide between the FDP and FDS tendon, as flexion is initiated by the FDP tendon in this position. | ||
** If therapists splint patients in greater degree of MCP joint flexion, flexion will be initiated by the intrinsics rather than the long flexors.<ref name=":13" /> | ** If therapists splint patients in a greater degree of MCP joint flexion, flexion will be initiated by the intrinsics rather than the long flexors.<ref name=":13" /> | ||
* Manchester short splint<ref name=":5">Peck FH, Roe AE, Ng CY, Duff C, McGrouther DA, Lees VC. The Manchester short splint: a change to splinting practice in the rehabilitation of zone II flexor tendon repairs. Hand Therapy. 2014 Jun;19(2):47-53.</ref> | * Manchester short splint<ref name=":5">Peck FH, Roe AE, Ng CY, Duff C, McGrouther DA, Lees VC. The Manchester short splint: a change to splinting practice in the rehabilitation of zone II flexor tendon repairs. Hand Therapy. 2014 Jun;19(2):47-53.</ref> | ||
** hand-based splint | ** hand-based splint | ||
| Line 195: | Line 195: | ||
** MCP joints - 30° flexion | ** MCP joints - 30° flexion | ||
** IP joints - neutral | ** IP joints - neutral | ||
** The use of the Manchester | ** The use of the Manchester sports splint appears to enhance the digital arc of flexion in the early phase. This results in improvements in DIP joint flexion and differential glide<ref name=":5" /> | ||
** Use of this type of splint showed improved outcomes, while still preserving repair integrity.<ref name=":5" /> | ** Use of this type of splint showed improved outcomes, while still preserving repair integrity.<ref name=":5" /> | ||
| Line 218: | Line 218: | ||
===== Place-and-hold Flexion Exercises ===== | ===== Place-and-hold Flexion Exercises ===== | ||
Place-and-hold flexion exercises | Place-and-hold flexion exercises consist out of the patient placing the finger or fingers down in passive flexion and then hold it into active flexion. Many flexor tendon rehabilitation protocols include place-and-hold flexion exercises. However, recent research shows that this causes gapping and forces through the tendon when the tendon is suddenly required to activate after passive flexion. Hand therapists are moving away from this exercise and instead prescribe active flexion to a half fist with active extension into the back of the splint.<ref name=":7" /> | ||
This open source article with videos included, provides a good overview of why true active movement is preferred over full fist place-and-hold flexion exercises: [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5142498/ Flexor Tendon Repair Postoperative Rehabilitation: The Saint John Protocol]<ref name=":10">Higgins A, Lalonde DH. Flexor tendon repair postoperative rehabilitation: the Saint John protocol. Plastic and Reconstructive Surgery Global Open. 2016 Nov;4(11).</ref> Be sure to watch the first video in the article. | This open source article with videos included, provides a good overview of why true active movement is preferred over full fist place-and-hold flexion exercises: [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5142498/ Flexor Tendon Repair Postoperative Rehabilitation: The Saint John Protocol]<ref name=":10">Higgins A, Lalonde DH. Flexor tendon repair postoperative rehabilitation: the Saint John protocol. Plastic and Reconstructive Surgery Global Open. 2016 Nov;4(11).</ref> Be sure to watch the first video in the article. | ||
===== Active Flexion ===== | ===== Active Flexion ===== | ||
Instead of place-and-hold exercises, therapists are now using more progressive protocols and are asking patients to perform active flexion to half a fist with active extension into the back of the splint. Active flexion can start from day one post-surgery. However if the patient only sees the therapist after day 8 post-surgery and has had no rehabilitation up until then, it is best not to start with active flexion exercises as the tendon is at its | Instead of place-and-hold exercises, therapists are now using more progressive protocols and are asking patients to perform active flexion to half a fist with active extension into the back of the splint. Active flexion can start from day one post-surgery. However if the patient only sees the therapist after day 8 post-surgery and has had no rehabilitation up until then, it is best not to start with active flexion exercises as the tendon is at its weakest during this stage of healing.<ref name=":7" /> | ||
===== Passive Flexion and Active Extension ===== | ===== Passive Flexion and Active Extension ===== | ||
| Line 258: | Line 258: | ||
==== Early Passive Flexion and Place-and-Hold ==== | ==== Early Passive Flexion and Place-and-Hold ==== | ||
A total of four studies investigated and compared early passive flexion and place-and-hold protocols. Moderate evidence was provided that place-and-hold | A total of four studies investigated and compared early passive flexion and place-and-hold protocols. Moderate evidence was provided that place-and-hold exercises lead to significantly better total active motion at 8 weeks compared to passive flexion exercises. This was only the case in patients with two-strand zone II repairs.<ref name=":11" /> | ||
==== Further Findings of Systematic Review ==== | ==== Further Findings of Systematic Review ==== | ||
| Line 267: | Line 267: | ||
In patients older than 30 years with a two-strand repair - greater total active motion was achieved at 12 weeks with a true active protocol than those who followed a passive flexion protocol<ref name=":11" /> | In patients older than 30 years with a two-strand repair - greater total active motion was achieved at 12 weeks with a true active protocol than those who followed a passive flexion protocol<ref name=":11" /> | ||
Well-designed intervention studies | Well-designed intervention studies are necessary to support the movement towards progressive protocols with true active motion and decreased immobilisation of the wrist.<ref name=":11" /> | ||
=== Examples of Rehabilitation Protocols === | === Examples of Rehabilitation Protocols === | ||
After optimising the repair, the therapist team works with the surgeon to select a rehabilitation plan that protects the repair but helps to maintain tendon gliding. The 3 | After optimising the repair, the therapist team works with the surgeon to select a rehabilitation plan that protects the repair but helps to maintain tendon gliding. The 3 types of rehabilitation programs implemented after a flexor tendon repair include: | ||
* Delayed mobilisation or Immobilisation | * Delayed mobilisation or Immobilisation | ||
** Indicated for children and non-compliant patients | ** Indicated for children and non-compliant patients | ||
| Line 302: | Line 302: | ||
Some red flags that therapists need to look out for when treating patients with flexor tendon injuries include<ref name=":7" />: | Some red flags that therapists need to look out for when treating patients with flexor tendon injuries include<ref name=":7" />: | ||
* Rupture | * Rupture | ||
** Look out for ruptures, especially during the first course of the six weeks of splinting. | **[[File:Red flag photo.jpg|thumb]]Look out for ruptures, especially during the first course of the six weeks of splinting. | ||
** Signs of tendon rupture may include: | ** Signs of tendon rupture may include: | ||
** FDP Tendon - patient may show a sign of no active DIP joint flexion when joint is isolated | ** FDP Tendon - the patient may show a sign of no active DIP joint flexion when the joint is isolated | ||
** FDS tendon repair - patient may not have any active PIP joint flexion when the PIP is isolated | ** FDS tendon repair - the patient may not have any active PIP joint flexion when the PIP is isolated | ||
** FPL tendon repair - patient may not have any isolated IP joint flexion | ** FPL tendon repair - the patient may not have any isolated IP joint flexion | ||
** If there is any concern about a patient who may have ruptured their tendon, it is important to | ** If there is any concern about a patient who may have ruptured their tendon, it is important to immediately get in touch with the surgeon. | ||
* Infection | * Infection | ||
** There is always a risk of infection with any surgery and if any signs of infection are present, it is important to get in touch with the surgeon. | ** There is always a risk of infection with any surgery and if any signs of infection are present, it is important to get in touch with the surgeon. | ||
** Signs of infection to look out for: | ** Signs of infection to look out for: | ||
** | ** Redness of and around the wound | ||
** | ** Presence of pus or cloudy wound drainage | ||
** | ** Increased temperature around wound or fever | ||
** | ** Bad odour coming from the wound | ||
* Contractures | * Contractures | ||
| Line 337: | Line 337: | ||
* Know your anatomy | * Know your anatomy | ||
** This helps with treatment planning and understanding the patient's injury. | ** This helps with treatment planning and understanding the patient's injury. | ||
* Be familiar with patient's history | * Be familiar with the patient's history | ||
** Understand the mechanism of injury | ** Understand the mechanism of injury | ||
** Be aware of the date of surgery and the details of the surgery | ** Be aware of the date of surgery and the details of the surgery | ||
** Was it a delayed surgery? Was the tendon frayed? | ** Was it a delayed surgery? Was the tendon frayed? | ||
** Knowing this information will guide your treatment approach. | ** Knowing this information will guide your treatment approach. | ||
** If a tendon is frayed or if it was a tight repair - patient might not be able to regain full range of motion. This is important for developing realistic expectations of the desired outcome, for both the therapist and the patient | ** If a tendon is frayed or if it was a tight repair - the patient might not be able to regain full range of motion. This is important for developing realistic expectations of the desired outcome, for both the therapist and the patient | ||
* Communicate with the surgeon | * Communicate with the surgeon | ||
** This is important to design a joint treatment plan for patients with flexor tendon repairs | ** This is important to design a joint treatment plan for patients with flexor tendon repairs | ||
Revision as of 22:57, 14 September 2020
Introduction[edit | edit source]
Flexor tendon injuries are some of the more common injuries, but yet complex injuries managed by hand surgeons. The flexor tendon mechanism plays a key role in the functionality of the hand. Physiotherapists and occupational therapists are often involved and play a key role in the post-surgical rehabilitation of flexor tendon repairs. A good understanding of the treatment procedures, healing stages, clinically relevant anatomy and rehabilitation of these injuries is necessary for a satisfactory outcome in the patient with a flexor tendon injury.
The below 8-minute video nicely outlines the key features of flexor tendon injuries treatment and anatomy.
Epidemiology of Flexor Tendon Injuries[edit | edit source]
- Incidence rate of 33.2 injuries per 100 00 person-years[2]
- Highest incidence of injury occurs at 20 -29 years of age, and the average age is 35 years[2]
- Higher incidence in males[2][3]
- Significant association between injury and age[2][3]
- Incidence is inversely related to age (injuries decrease with increase in age)[3]
- Extensor tendon injuries occur more frequently than flexor tendon injuries[2]
- Majority of cases involve a single tendon, extensor tendon injuries involves Zone III of the index finger and flexor tendons involve Zone II of the index finger[2]
- Common injury in people working in physical construction jobs, using saws, glass or getting metal lacerations[2][3]
- Also common in people working in food preparation with knife injuries[2][3]
- In recent years, the media has highlighted the increase in tendon injuries as a result of poor avocado de-seeding technique. In research a rising increase in avocado-related knife injuries to the hand has been reported[4]
Clinically Relevant Anatomy[edit | edit source]
The tendons that can be involved include:
- Flexor pollicis longus (flexion tip of the thumb)
- Flexor digitorum profundus (flexion of the fingers)
- Flexor digitorum superficialis (flexes the middle joint of each finger)
- Flexor carpi ulnaris
- Flexor carpi radialis
For the purpose of this page, specific anatomical details will be provided on the major muscles and tendons involved in flexion of the fingers and the ones most commonly injured.
Flexors of the Fingers[edit | edit source]
Flexor Digitorum Superficialis[5][edit | edit source]
- lies in the anterior compartment of forearm, deep to pronator teres, palmaris longus and flexors carpi ulnaris and radialis
- superficial to flexor digitorum profundus and flexor pollicis longus
- muscle has a long linear origin, but considered to arise by two heads
- Origin:
- medial/ humeroulnar head:
- lateral/radial head origin:
- upper two thirds of the anterior border of the radius
- halfway down the forearm, the muscle narrows and forms four separate tendons passing deep to the flexor retinaculum, here they are arranged in two pairs to enter the hand:
- superficial pair pass to the middle and ring fingers
- deep pair pass to the index and ring finger
- Insertion:
- palmar surface of the base of the middle phalanges
- Action:
- flexion of the metacarpophalangeal and proximal interphalangeal joints
- also contributes to flexion of the wrist
Flexor Digitorum Profundus[5][edit | edit source]
- lies deep to flexor digitorum superficialis on medial side of forearm
- Origin:
- arises from medial side of the coronoid process of the ulna, the upper three quarters of the anterior and medial surfaces of the ulna, and the medial, middle third of the adjacent interosseus membrane
- also arises from the aponeurosis that attaches the flexor carpi ulnaris to the posterior border of the ulna
- part of muscle arising from interosseus membrane forms a separate tendon halfway down the forearm, this passes to the index finger
- remaining tendons formed just proximal to the flexor retinaculum
- separate tendons pass below the flexor retinaculum, lying side by side, deep to the tendons of flexor digitorum superficialis, but in the same synovial sheath
- the four tendons pass to their respective fingers in the palm
- Insertion:
- base of the palmar/volar surface of the distal phalanges
- Action:
- flexion of the distal interphalangeal joint
- also aids in flexion of the proximal interphalangeal, metacarpophalangeal and wrist joints, as it crosses several other joints during its course
Flexor Pollicis Longus[5][edit | edit source]
- lies on lateral side of flexor digitorum profundus
- Origin:
- arises from anterior surface of the radius, between the radial tuberosity above and pronator quadratus below, and the adjacent anterior surface of the coronoid process of the ulna
- fibres pass almost to the wrist, before the tendon is formed
- tendon passes below flexor retinaculum
- Insertion:
- palmar/volar surface of the base of the distal phalanx of the thumb
- Action:
- flexor of the interphalangeal joint of the thumb
- vital for all gripping activities of the hand
- also flexes the metacarpophalangeal joint of the thumb and the wrist joint
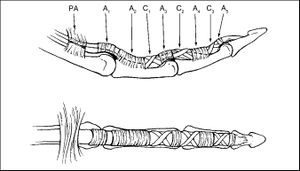
Pulley System in the Hand[edit | edit source]
- The pulley system is an important anatomical structure in understanding the tendon system in the hand.[6]
- The annular pulley system's function is to keep the tendons close to the bone, so that tendons don't bowstring in active flexion.[7]
- The cruciform pulley system is flexible and collapsible to allow for digital flexion without deformation of the pulley system.[7]
- This is key to remember when treating people who had a tendon repair as patients can sometimes present with bowstringing after a tendon repair.[7]
- Knowing the anatomy and function of the pulley system will aid in the clinical reasoning of the therapists as to why this is occurring.[6]
For more information on the Pulley System in the Hand, read this Physiopedia Page: Hand Pulleys
Vincula Tendinum[edit | edit source]
The tendons of flexor digitorum superficialis provide attachments for the vincula tendinum, which convey blood vessels to the tendon. The flexor tendons are encapsulated in a sheath. The flexor digitorum superficialis and flexor digitorum profundus have two vinicula each.[5] These tendons are not well-vascularised and there are some avascular areas that receive nutrition by diffusion.[6]
This mechanisms puts the tendons at risk for adhesions. When adhesions are present, the tendon can not glide freely and this leads to a limited range of motion and limited functional capacity.[6]
Tendon Injury Zones[edit | edit source]
It is important to know and have a good understanding of the different tendon zones as this will:
- inform treatment planning
- the type of splint design that patient will need
Tendon zones differ for the extensors and the flexors. For the finger flexors the zones are as follows[7][8]:
- Zone I - distal to the flexor digitorum superficialis (FDS)
- Zone II - from the FDS insertion to distal portion of the A1 pulley
- Zone III - from the A1 pulley to the transverse carpal ligament
- Zone IV - the carpal tunnel
- Zone V - proximal to carpal tunnel
The thumb has its own zone distrubution:
- Zone I - distal to the interphalangeal joint (IP) in the thumb
- Zone II - between the metacarpophalangeal (MCP) and interphalangeal (IP) joints
- Zone III - proximal to the metacarpophalangeal (MCP) volar/palmar flexion crease
Mechanism of Injury[edit | edit source]
Flexor tendon injuries commonly result from volar/palmar lacerations. This can occur with an accompanying neurovascular injury.[8] Patients often present directly at a hospital as they have most likely sustained a significant laceration.
Another mechanism of injury is a rupture rather than a laceration, for example the FDP tendon has ruptured from its insertion at the distal phalanx - usually this is caused by a closed mechanism of injury. This usually occurs as a result of forced extension during active flexion. This happens in ball sports where a finger is forced into extension while it is being flexed or where a player grabs an opponent's shirt (jersey finger) or in activities such as rock climbing.[9]
Clinical Presentation[edit | edit source]
Depending on the area of injury symptoms may include:
- Loss of active flexion strength or motion of the involved digit(s)
- Pain when attempting to flex the involved digit
- Swelling
- Tenderness
Diagnostic Procedures[edit | edit source]
- Clinical tests:
- Flexor Digitorum Profundus (FDP) tendon - the patient is unable to flex the distal interphalangeal joint (DIP) in isolation[10]
- Flexor Digitorum Superficialis (FDS) tendon - isolate the involved/affected finger and ask the patient to flex the proximal interphalangeal joint (PIP)[10]
- Flexor Pollicis Longus tendon - flexing the interphalangeal joint (IP) joint of the thumb in isolation[10]
- Radiographs - may have associated fracture
- Ultrasound - used to assess suspected lacerations[8]
- MRI
Outcome Measures[edit | edit source]
- Grip strength
- DASH
- Goniometer measurement
Medical Management[edit | edit source]
Surgical Repair[edit | edit source]
Surgical repair is needed for a cut or ruptured tendons. When a tendon ruptures, the ends separate as a result of the tension in the tendons. Sometimes this separation between the cut or ruptured ends of the tendon can be several centimetres. Surgical repair is necessary in order to regain function that has been lost. The repair may be performed under general anaesthetic or regional anaesthetic (injection of local anaesthetic at the shoulder). During surgery, the wound is enlarged so that the cut ends of the tendon can be found and held together with stitches. After the surgery, the hand and forearm are immobilised in a splint that is placed over the bandages with the wrist and fingers in a slightly bent position, in order to protect the repair.[11]
The tendon repair is a surgeon-dependant process and surgeons will decide on the most appropriate technique for the specific tendon repair. Common repairs are four-strand or six-strand repairs.
Post-Surgical Tendon Healing[edit | edit source]
The healing stages of tendons include three phases[12][13]:
Inflammatory phase[edit | edit source]
- the first phase
- lasts from day one to day seven post-operatively
- in this stage, fibroblasts produce type III collagen and macrophages help initiate healing and remodelling
Proliferative phase[edit | edit source]
- this is the second phase
- this runs from day 8 to about three weeks post-operatively
- tissue modelling via large amounts of disorganised collagen happens during this stage
- angiogenesis also happens during this stage
Remodelling phase[edit | edit source]
- this is the third stage
- occurs up until about 18 months post-operatively
- in this stage, tensile forces lead to tissue remodelling, and type III collagen is replaced with type I collagen
- this happens in a more linear fashion, and this creates cross-linking to build strength in the tendon
Post-Surgical Physiotherapy Management[edit | edit source]
Therapists need to have knowledge about the anatomy, the pulleys, tendon injury zones and the tendon healing stages as this will inform the treatment approach. For example, the tendon injury zone will dictate the splint design and the treatment process. The tendon healing time and stage will influence the type of rehabilitation exercises to commence with. For example, if a patient is referred for therapy at 8 or 9 days post-surgery and the patient has not had any therapy yet, the therapist would probably not want to start with active range of motion exercises as the tendon is at its weakest from day 8 to day 21 post-operatively. Therapists also need to be aware of the importance of the flexor mechanism in the functional use of the hand and how a flexor tendon injury can functionally impact a patient.[6]
Wound and Scar Management[edit | edit source]
After surgery wound management is the first step to address. The post-surgical wound may be dressed with a basic silicone dressing (products such as Mepitel may be used). The finger is wrapped with breathable handy gauze material. Other products that therapists may use include Coban, but a good, comfortable, clean and a dry dressing is acceptable as well.
Compression bandaging is used to control oedema.
Once the wound is healed, scar management can commence. Silicone gel sheeting can be used on the scar or paper tapes or products for scar management such as Fixomull. Scar massage can be done during therapy sessions and at home to prevent adhesions.[6]
Patient Education[edit | edit source]
- Patient education is critical in the management of flexor tendon injuries.[6]
- Patients need to be aware of the necessary precautions.
- The wound needs to be kept clean and dry.
- The splint needs to stay on 24 hours a day, 7 days a week.
- If the splint does need to come off, the patient needs to be educated about safe hand positioning.
- For a flexor injury, the patient needs to keep the fingers cupped with the wrist in neutral if the splint is off.
- This position does not put any stretch or tension on the tendons.
- Therapy sessions are usually twice a week for the first two weeks post-surgery.
- Thereafter, weekly sessions until around 10 weeks post-surgery.
Orthoses[edit | edit source]
FDP and FDS Tendon Repair[edit | edit source]
- Forearm-based metacarpophalangeal joint (MCP) extension blocking splint with wrist in neutral and MCP's in around 30° of flexion.[6]
- Zone I, II and III injuries of the flexor digitorum profundus and/or the flexor digitorum superficialis
- This promotes the arc of flexion to be activated by the long flexors, rather than the intrinsics[14]
- It allows differential glide between the FDP and FDS tendon, as flexion is initiated by the FDP tendon in this position.
- If therapists splint patients in a greater degree of MCP joint flexion, flexion will be initiated by the intrinsics rather than the long flexors.[14]
- Manchester short splint[15]
- hand-based splint
- allows maximal wrist flexion, blocks wrist extension at 45°
- MCP joints - 30° flexion
- IP joints - neutral
- The use of the Manchester sports splint appears to enhance the digital arc of flexion in the early phase. This results in improvements in DIP joint flexion and differential glide[15]
- Use of this type of splint showed improved outcomes, while still preserving repair integrity.[15]
FPL Repair[edit | edit source]
- Dorsal forearm-based orthosis[6]
- goes to the tip of the thumb up to three quarters of the metacarpal length on the dorsum of the hand
- wrist in neutral
- thumb slightly palmar-flexed into eased opposition with the MCP in about 20° of flexion and IP joint in neutral
The type of orthosis/splint that will be used in a patient is often prescribed by the surgeon and therapists will need to discuss the appropriate choice of splint with the surgeons that they work with.
Rehabilitation Exercises[edit | edit source]
The goal of the rehabilitation exercises after a flexor tendon repair is to[6][12]:
- keep the tendons gliding and promote differential tendon glide
- control early collagen deposition
- facilitate strengthening of the repair site
- prevent adhesions, tendon gapping or re-rupture
- provide patients with the best possible outcome after surgery
Various different protocols have been developed for the rehabilitation of flexion tendon repairs. These programs usually make use of combinations of active and passive range of motion.
Post-Operative Exercises FDS and FDP Repairs (first 6 weeks)[edit | edit source]
Place-and-hold Flexion Exercises[edit | edit source]
Place-and-hold flexion exercises consist out of the patient placing the finger or fingers down in passive flexion and then hold it into active flexion. Many flexor tendon rehabilitation protocols include place-and-hold flexion exercises. However, recent research shows that this causes gapping and forces through the tendon when the tendon is suddenly required to activate after passive flexion. Hand therapists are moving away from this exercise and instead prescribe active flexion to a half fist with active extension into the back of the splint.[6]
This open source article with videos included, provides a good overview of why true active movement is preferred over full fist place-and-hold flexion exercises: Flexor Tendon Repair Postoperative Rehabilitation: The Saint John Protocol[16] Be sure to watch the first video in the article.
Active Flexion[edit | edit source]
Instead of place-and-hold exercises, therapists are now using more progressive protocols and are asking patients to perform active flexion to half a fist with active extension into the back of the splint. Active flexion can start from day one post-surgery. However if the patient only sees the therapist after day 8 post-surgery and has had no rehabilitation up until then, it is best not to start with active flexion exercises as the tendon is at its weakest during this stage of healing.[6]
Passive Flexion and Active Extension[edit | edit source]
- The patient can perform passive flexion of the fingers and then actively extend the fingers into the back of the splint.
- A way to prevent any PIP joint flexion adhesions is to put a ruler down the back of the splint for the patient to actively extend against.[6]
Exercise Frequency and Precautions[edit | edit source]
- Patients should perform these exercises for 10 repetitions, five times a day.[6]
- Patients always do their exercises with the splint, so that there is no risk of extending the fingers and rupturing or putting the tendon at risk.
Post- Operative Exercises FPL Repair (first 6 weeks)[edit | edit source]
- Passive IP joint flexion exercises
- Passive thumb composite flexion
- Active flexion to about half of the patient's active range of motion
- 10 repetitions, 5 times a day
Post-Operative Exercises after 6 weeks[edit | edit source]
For all post-surgical tendon repairs - the splints are worn for 6 weeks
- After the initial 6 weeks, the patient is weaned out of the splint to commence light functional use
- Slowly increase and grade the patient's full active and full passive range of motion
- Strengthening can usually commence at about 8 weeks post-surgery
- Strengthening exercises can include activities such as:
- Squeezing Theraputty, Play-doh or a sponge in hot water
- Can progress to wrist weights and Theraband if appropriate, for complete upper limb strengthening
- Once the patient is able to return to his/her leisure activities, is able to use the hand functionally with few limitations and pain is under control, the patient can be discharged with a home program of continued stretching, scar management and strengthening exercises.[6]
Evidence for Different Types of Rehabilitation Exercises[edit | edit source]
In a recent systematic review by Nieduski and Powell (2019)[17] nine studies were compared. These studies investigated early active motion (EAM) or true active flexion as opposed to early passive or place-and-hold flexion to determine which method is the most appropriate and has the most scientific support. The primary outcome measure was total active motion (TAM).
Early Active Motion[edit | edit source]
Two studies investigated progressive protocols that entailed modifying the position of the hand in the protective orthosis after a flexor tendon repair. The degree of metacarpophalangeal flexion was decreased to 30° and a hand-based orthosis was incorporated.[15][16]
In the study by Peck et al (2014)[15] wrist mobilisation and immobilisation were compared and light use of the affected hand was allowed in the immediately postoperative phase. No significant difference was found between the two study groups in total active motion or ruptures at 12 weeks. However, the group with the hand-based orthosis did show significant improvements in DIP flexion and PIP extension compared to those participants who wore a forearm-based splint.
Early Passive Flexion and Place-and-Hold[edit | edit source]
A total of four studies investigated and compared early passive flexion and place-and-hold protocols. Moderate evidence was provided that place-and-hold exercises lead to significantly better total active motion at 8 weeks compared to passive flexion exercises. This was only the case in patients with two-strand zone II repairs.[17]
Further Findings of Systematic Review[edit | edit source]
Tendon repair strength of at least four-strands is needed to withstand the forces of true active motion[17]
Moderate to high level evidence that place-and-hold exercises provide better outcomes than passive flexion protocols, including Kleinert and modified Kleinert protocols, in patients with two- to six-strand repairs[17]
In patients older than 30 years with a two-strand repair - greater total active motion was achieved at 12 weeks with a true active protocol than those who followed a passive flexion protocol[17]
Well-designed intervention studies are necessary to support the movement towards progressive protocols with true active motion and decreased immobilisation of the wrist.[17]
Examples of Rehabilitation Protocols[edit | edit source]
After optimising the repair, the therapist team works with the surgeon to select a rehabilitation plan that protects the repair but helps to maintain tendon gliding. The 3 types of rehabilitation programs implemented after a flexor tendon repair include:
- Delayed mobilisation or Immobilisation
- Indicated for children and non-compliant patients
- Casts/splints are applied with the wrist and MCP joints positioned in flexion and the IP joints in extension
- Early passive mobilisation
- Examples of these protocols include:
- Duran protocol: low force and low excursion; active finger extension with patient-assisted passive finger flexion and static splint
- Kleinert protocol: low force and low excursion; active finger extension with dynamic splint-assisted passive finger flexion
- Mayo synergistic splint: low force and high tendon excursion; adds active wrist motion which increases flexor tendon excursion the most
- Examples of these protocols include:
- Early active mobilisation
- Moderate force and potentially high excursion
- Dorsal blocking splint limiting wrist extension
- Early active mobilisation without place-and-hold
- Perform place-and-hold exercises with digits (see earlier evidence about this)
No guidelines for rehabilitation should be followed exactly. Many factors influence therapy decisions such as:
- repair technique
- associated tendon healing
- passive versus active range of motion
- oedema
- tendon adhesions
These factors can assist in guiding rehabilitation progression and promote functional range of motion, safely mobilise the repaired tendon(s) and prevent gapping, rupture, and adhesions.[18]
Here are some examples of flexor tendon injury rehabilitation protocols:
- Brigham and Women's Hospital. Department of Rehabilitation Services. Zones 2-5 Flexor tendon repair Protocol
- Flexor Tendon Repair Postoperative Rehabilitation: The Saint John Protocol
- Flexor Tendon Repairs
- Manchester Protocol
- Hand Therapy Protocols (various protocols are outlined in this document, including the Kleinert, modified Kleinert and Duran protocols)
Red Flags[edit | edit source]
Some red flags that therapists need to look out for when treating patients with flexor tendon injuries include[6]:
- Rupture
- Look out for ruptures, especially during the first course of the six weeks of splinting.
- Signs of tendon rupture may include:
- FDP Tendon - the patient may show a sign of no active DIP joint flexion when the joint is isolated
- FDS tendon repair - the patient may not have any active PIP joint flexion when the PIP is isolated
- FPL tendon repair - the patient may not have any isolated IP joint flexion
- If there is any concern about a patient who may have ruptured their tendon, it is important to immediately get in touch with the surgeon.
- Infection
- There is always a risk of infection with any surgery and if any signs of infection are present, it is important to get in touch with the surgeon.
- Signs of infection to look out for:
- Redness of and around the wound
- Presence of pus or cloudy wound drainage
- Increased temperature around wound or fever
- Bad odour coming from the wound
- Contractures
- Especially in patients who have had FDS and FDP tendon repairs
- If a patient develops a contracture, they will sometimes need dynamic splinting about 8 - 10 weeks post-surgery
- It is important for patients to do their exercises during the first 6 weeks in their dorsal blocking splint and to encourage active extension, especially of the PIP joint into the back of the splint, to prevent contractures. It also prevents flexion adhesions and PIP joint contractures.
- Scar Adhesions
- Scar adhesions can limit a patient's arc of flexion and range of motion in their finger for active and passive movement, and into flexion and extension.
- Massaging the scar as much as possible is necessary and getting the skin to glide freely from the underlying tendons
- It is important to prevent adhesions right from the beginning
- If there are significant adhesions and it is indicated, patients may need tenolysis surgery or tendon releasing surgery.
- Loss of sensation
- Sometimes, patients have some minimal nerve damage at the time of injury, that does not need surgical repair, but through the course of the six weeks of splinting symptoms of nerve damage develop. These symptoms include:
- numbness, tingling or pins and needles in the affected finger
- It is important to discuss these signs and symptoms with the surgeon as further surgery may be required if the nerve has been lacerated and not able to heal conservatively.
- Sometimes, patients have some minimal nerve damage at the time of injury, that does not need surgical repair, but through the course of the six weeks of splinting symptoms of nerve damage develop. These symptoms include:
Key Concepts to Remember[edit | edit source]
Some key messages to remember with flexor tendon injury management[6]:
- Know your anatomy
- This helps with treatment planning and understanding the patient's injury.
- Be familiar with the patient's history
- Understand the mechanism of injury
- Be aware of the date of surgery and the details of the surgery
- Was it a delayed surgery? Was the tendon frayed?
- Knowing this information will guide your treatment approach.
- If a tendon is frayed or if it was a tight repair - the patient might not be able to regain full range of motion. This is important for developing realistic expectations of the desired outcome, for both the therapist and the patient
- Communicate with the surgeon
- This is important to design a joint treatment plan for patients with flexor tendon repairs
- These patients can have quite complex injuries and having good and clear communication with the surgeon, will help in understanding the required rehabilitation protocol and also will benefit the patient
- Keep tendons gliding to prevent adhesions
- Aim for an active range of motion protocol where possible
- Try to get a patient started with rehabilitation exercises before day 7 post-surgery
- This will help prevent scar tissue formation and creating adhesions.
- Be aware of and look out for red flags
- ruptures
- infection
- possible complications
References[edit | edit source]
- ↑ J Knight Flexor tendon surgery Available from: https://www.youtube.com/watch?v=nrZdYJdrSCo&app=desktop (last accessed 8.12.2019)
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 2.7 de Jong JP, Nguyen JT, Sonnema AJ, Nguyen EC, Amadio PC, Moran SL. The incidence of acute traumatic tendon injuries in the hand and wrist: a 10-year population-based study. Clinics in orthopedic surgery. 2014 Jun 1;6(2):196-202.
- ↑ 3.0 3.1 3.2 3.3 3.4 Manninen M, Karjalainen T, Määttä J, Flinkkilä T. Epidemiology of flexor tendon injuries of the hand in a Northern Finnish population. Scandinavian journal of surgery. 2017 Sep;106(3):278-82.
- ↑ Farley KX, Aizpuru M, Boden SH, Wagner ER, Gottschalk MB, Daly CA. Avocado-related knife injuries: describing an epidemic of hand injury. The American journal of emergency medicine. 2020 May 1;38(5):864-8.
- ↑ 5.0 5.1 5.2 5.3 Palastanga NP, Field D, Soames R. Anatomy and Human Movement: Structure and Function. 5th Edition. Edinburgh: Butterworth Heinemann, Elsevier. 2006.
- ↑ 6.00 6.01 6.02 6.03 6.04 6.05 6.06 6.07 6.08 6.09 6.10 6.11 6.12 6.13 6.14 6.15 6.16 Thorn, K. Flexor Tendon Injury Management. Course, Physioplus. 2020.
- ↑ 7.0 7.1 7.2 7.3 Klifto CS, Capo JT, Sapienza A, Yang SS, Paksima N. Flexor tendon injuries. JAAOS-Journal of the American Academy of Orthopaedic Surgeons. 2018 Jan 15;26(2):e26-35.
- ↑ 8.0 8.1 8.2 Ortho bullets Flexion tendon injuries Available from: https://www.orthobullets.com/hand/6031/flexor-tendon-injuries (last accessed 8.12.2019)
- ↑ Cole KP, Uhl RL, Rosenbaum AJ. Comprehensive review of rock climbing injuries. JAAOS-Journal of the American Academy of Orthopaedic Surgeons. 2020 Jun 15;28(12):e501-9.
- ↑ 10.0 10.1 10.2 Khor WS, Langer MF, Wong R, Zhou R, Peck F, Wong JK. Improving outcomes in tendon repair: a critical look at the evidence for flexor tendon repair and rehabilitation. Plastic and reconstructive surgery. 2016 Dec 1;138(6):1045e-58e.
- ↑ BSHH Flexor tendon injuries Available from: https://www.bssh.ac.uk/patients/conditions/26/flexor_tendon_injury#What_is_the_treatment_ (last accessed 8.12.2019)
- ↑ 12.0 12.1 Klifto CS, Bookman J, Paksima N. Postsurgical Rehabilitation of Flexor Tendon Injuries. The Journal of hand surgery. 2019 Aug 1;44(8):680-6.
- ↑ Legrand A, Kaufman Y, Long C, Fox PM. Molecular biology of flexor tendon healing in relation to reduction of tendon adhesions. The Journal of hand surgery. 2017 Sep 1;42(9):722-6.
- ↑ 14.0 14.1 Seaward JR, Peck F, Lees VC. Impact of Long Flexor Versus Intrinsic Dominance in the Generation of Arc of Finger Flexion. Hand. 2016 Sep;11(3):364-7.
- ↑ 15.0 15.1 15.2 15.3 15.4 Peck FH, Roe AE, Ng CY, Duff C, McGrouther DA, Lees VC. The Manchester short splint: a change to splinting practice in the rehabilitation of zone II flexor tendon repairs. Hand Therapy. 2014 Jun;19(2):47-53.
- ↑ 16.0 16.1 Higgins A, Lalonde DH. Flexor tendon repair postoperative rehabilitation: the Saint John protocol. Plastic and Reconstructive Surgery Global Open. 2016 Nov;4(11).
- ↑ 17.0 17.1 17.2 17.3 17.4 17.5 Neiduski RL, Powell RK. Flexor tendon rehabilitation in the 21st century: A systematic review. Journal of Hand Therapy. 2019 Apr 1;32(2):165-74.
- ↑ Kannas S, Jeardeau TA, Bishop AT. Rehabilitation following zone II flexor tendon repairs. Techniques in hand & upper extremity surgery. 2015 Mar 1;19(1):2-10. Available from: https://www.ncbi.nlm.nih.gov/pubmed/25700105 (last accessed 9.12.2019)