Femoral Neck Hip Fracture: Difference between revisions
No edit summary |
No edit summary |
||
| Line 731: | Line 731: | ||
Prolonged bed rust can increase the risk of pressure sores and deconditioning. Therefore it’s important to start rehabilitation on the first post-operative day (on patients with a total hip replacement). This includes quadriceps strengthening exercises, isometric exercises, and flexion and extension mobilizations in the hip joint …[13] | Prolonged bed rust can increase the risk of pressure sores and deconditioning. Therefore it’s important to start rehabilitation on the first post-operative day (on patients with a total hip replacement). This includes quadriceps strengthening exercises, isometric exercises, and flexion and extension mobilizations in the hip joint …[13] | ||
On the second and third post-operative day the patient can start with walking between parallel bars, and later on they can walk with a walker or a cane. This walking is supervised. <br>The physiotherapist will begin with range of motion exercises for the hip, knee and ankle because mobility is decreased following immobilization. Mobilization is a very important treatment in the recovery process. <br>The patient can also begin strengthening exercises based on the surgeon's orders (typically six weeks post-op). Patients should also undergo balance and proprioceptive rehab and these abilities are quickly lost with inactivity.[28]<br>Weight-bearing exercises are very important for mobility, balance, activities of daily living and quality of life[5](level of evidence B), examples: | On the second and third post-operative day the patient can start with walking between parallel bars, and later on they can walk with a walker or a cane. This walking is supervised. <br>The physiotherapist will begin with range of motion exercises for the hip, knee and ankle because mobility is decreased following immobilization. Mobilization is a very important treatment in the recovery process. <br>The patient can also begin strengthening exercises based on the surgeon's orders (typically six weeks post-op). Patients should also undergo balance and proprioceptive rehab and these abilities are quickly lost with inactivity.[28]<br>Weight-bearing exercises are very important for mobility, balance, activities of daily living and quality of life[5](level of evidence B), examples:[[Image:Figure6.png|thumb|right]] | ||
*Stepping in different directions | *Stepping in different directions | ||
| Line 767: | Line 767: | ||
Twelve weeks of progressive strength training once a week, as a follow-up to a more intensive training period after hip fracture has no measureable effect upon the BBS (Berg Balance Scale) score, but may improve strength, endurance, self-reported NEADL (The Nottingham Extended Activities of Daily Living score), and self-perceived health.<br>Home-dwelling hip fracture patients seem to constitute a group that needs prolonged follow-up to achieve the improvements that are important for independent functioning.[25] | Twelve weeks of progressive strength training once a week, as a follow-up to a more intensive training period after hip fracture has no measureable effect upon the BBS (Berg Balance Scale) score, but may improve strength, endurance, self-reported NEADL (The Nottingham Extended Activities of Daily Living score), and self-perceived health.<br>Home-dwelling hip fracture patients seem to constitute a group that needs prolonged follow-up to achieve the improvements that are important for independent functioning.[25] | ||
Prevention is also a part of the rehabilitation process to prevent fractures. Prevention of hip fractures should focus on preventing falls and osteoporosis. <br>Several strategies could help reduce the loss of bone density that underlies hip fracture. Among these, a substantial body of evidence indicates that physical activity is the most important, and it is a method of prevention that can be enjoyable and sociable. <br>Regular exercise would reduce the risk of hip fracture by at least half.<br>Stopping smoking is also important, and a woman who stops smoking before the menopause will reduce her risk by about a quarter. [29]<br>Both these policies can be adopted by both sexes and continued into old age. Postmenopausal oestrogen replacement more than halves the risk of hip fracture, but the loss of this protection within a few years of stopping treatment limits its utility. <br>Oestrogen replacement would need to be continued almost indefinitely if it were to do more than reduce the incidence of hip fracture in younger age groups, in whom hip fracture is uncommon and recovery generally uncomplicated. General calcium supplementation is not justified as the likely benefit is too small.[29]<br>Interventions to reduce the risk of falls should target identified risk factors (e.g., muscle weakness; history of falls; use of four or more prescription medications; use of an assistive device; arthritis; depression; age older than 80 years; impairments in gait, balance, cognition, vision, or activities of daily living).(26)<br> | Prevention is also a part of the rehabilitation process to prevent fractures. Prevention of hip fractures should focus on preventing falls and osteoporosis. <br>Several strategies could help reduce the loss of bone density that underlies hip fracture. Among these, a substantial body of evidence indicates that physical activity is the most important, and it is a method of prevention that can be enjoyable and sociable. <br>Regular exercise would reduce the risk of hip fracture by at least half.<br>Stopping smoking is also important, and a woman who stops smoking before the menopause will reduce her risk by about a quarter. [29]<br>Both these policies can be adopted by both sexes and continued into old age. Postmenopausal oestrogen replacement more than halves the risk of hip fracture, but the loss of this protection within a few years of stopping treatment limits its utility. <br>Oestrogen replacement would need to be continued almost indefinitely if it were to do more than reduce the incidence of hip fracture in younger age groups, in whom hip fracture is uncommon and recovery generally uncomplicated. General calcium supplementation is not justified as the likely benefit is too small.[29]<br>Interventions to reduce the risk of falls should target identified risk factors (e.g., muscle weakness; history of falls; use of four or more prescription medications; use of an assistive device; arthritis; depression; age older than 80 years; impairments in gait, balance, cognition, vision, or activities of daily living).(26)<br> | ||
== Key Research == | == Key Research == | ||
Revision as of 15:54, 1 June 2016
Original Editors
Top Contributors - Delmoitie Giovanni, Lucinda hampton, Simisola Ajeyalemi, Jessie Tourwe, Joyce De Gelas, Kim Jackson, Admin, Tolulope Adeniji, Aminat Abolade, Debontridder Jordy, Vidya Acharya, Annelies Beckers, Sara Evenepoel, Yarne Leuckx, Claire Knott, Lauren Lopez, Elien Lebuf and Karen Wilson
Search Strategy[edit | edit source]
Databases searched: Pubmed, PEDro, eMedicine, Medscape,Handbook of fractures, Prometheus, Kapandji
Keywords searched: hip fracture, incidence femoral neck fracture, osteoporotic hip fracture, treatment hip fractures …
Definition/Description[edit | edit source]
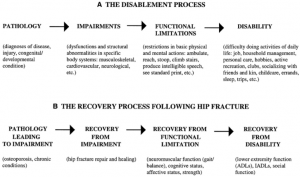
A hip fracture is a condition in which the proximal end of the femur, near the hip joint, is broken. Such a fracture is a serious injury that occurs mostly in elderly people over 65 years and complications can be life threatening. [1](level of evidence A1)
The femur is the largest and strongest bone in the body, so it requires a large or high impact force to break. Most femur fractures are the result of a high energy trauma, such as a motor accident, gunshot wound, or jump/fall from a height. [1]
However, in an older population a simple fall may cause a femoral fracture due to reduced bone mineral density. A femoral fracture is a very serious injury and needs 3-6 months to heal. [1]
High mortality, long-term disability and huge socio-economic burden are the main consequences of a hip fracture. [1]
The biggest risk factors for running up a hip fracture are osteoporosis and cognitive impairment. [1]
Clinically Relevant Anatomy[edit | edit source]
The hip joint is a ball and socket joint, formed by the head of the femur and the acetabulum of the pelvis. [2]
The head of the femur is almost ( for ¾ ) shaped like a sphere. The acetabulum is formed by the three parts of the os Coxae. It is a fusion of illium, ischium and pubis. [2]
Through this fusion the acetabulum is shaped like an hemisphere (the inner section of a sphere). [2]
Thereby the acetabulum is not covering the entire head of the femur. [2]
The convex head fits perfectly in the concave socket of the acetabulum forming a synovial joint. [2]
From an osteological viewpoint, the proximal end of the femur in four major parts, namely: femoral head, femoral neck, greater trochanter and the lesser trochanter. [2]
These parts are most often and most closely involved with hip fractures. The hip joint is a very sturdy joint, due to the tight fitting of the bones and the strong surrounding ligaments and muscles. [2]
So a hip luxation will less likely take place. [2]
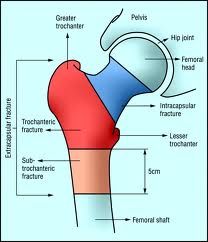
Hip fractures can be classified into intracapsular (femoral neck) fractures and extracapsular fractures .
The intracapsular fractures are contained within the hip capsule itself. Those fractures are subcapital neck fracture, and transcervical neck fracture.
The extracapsular fractures are intertrochanteric and subtrochanteric fracture. You also have a greater and lesser trochanter fractures. (figure1) [3]
Epidemiology /Etiology[edit | edit source]
</blockquote> Etiology:
Risk factors for hip fractures[6][9]:
- Bone density: Decreased bone density is dangerous for causing hip fractures
- Muscle mass: Decreased muscle mass is also dangerous, it could contribute with other causes to cause a hip fracture
- Sex: From all the hip fractures, 70% of them occurs women, so that’s a significant lot more than by men. It’s common after the menopause that the bone density of women decreases very fast, so that’s a main cause for hip fractures
- Fall: All the reasons witch can make you fall: dizziness, vision problems, deaf persons,…
- Medications: Some medications can cause a decrease in bone density like cortisone.
- Nutrition: It is well known that calcium and vitamin D increase bone mass, so a lack of it can cause several fractures, including hip fractures. Some eating disorders like anorexia and bulimia can weaken your bones, zo you become more fragile to have a hip fracture.
- Age: the older you get, the higher the risk is for hip fractures. 90% of these fractures occur in persons over 70 years old.
- Alcohol and tobacco: These products can reduce the bone mass, causing a higher risk to have a hip fracture
- Medical problems: Endocrine disorders can cause fragility of the bones
- Physical activity: Physical activity is very important for the muscle mass and the bone mass, so if you practice enough sports you will have less risk to have hip fractures.
- Stroke disease → high risk factor for falls who can cause a hip fracture.
- Parkinson’s disease → high risk factor for falls who can cause a hip fracture. [6][9]
Causes: [7]
- Trauma or laesion in the femur ( around 10% )
- Local pathologies ( 1% ): example: metastatic malignancy ( A tumor who can affect the bone marrow, it’s a very dangerous disease)
- Fall ( Most of the hip fractures are caused by falls)
- Hip fractures without injuries ( < 5% )
- Osteoporosis: Osteoporosis is a multifactorial, chronic disease that may progress silently for decades until characteristic fractures occur late in life. [7]
Because there are no symptoms prior to fracture, relatively few people are diagnosed in time for effective therapy to be administered (Johnston et al. 1989). [7]
Consequently, a large number of individuals experience hip fracture-related pain, expense, disability, and decreased quality of life. [7]
This number is increasing because fracture incidence rates rise dramatically with age, and populations are ageing rapidly around the world. [7]
The incidence rates themselves are rising in some regions, and any further improvements in life expectancy will compound the problem. [7]
A substantial portion of the population is at risk of hip fracture by virtue of low bone mass and frequent falls. [7]
Due to the sheer size of the affected population, control programs for osteoporosis are likely to be expensive, but effective and efficient prevention efforts have great potential promise. [7]
Epidemiology:
In 1990 there were estimated to be 1.66 million hip fractures around the world, and it’s also estimated that this number will rise to 6.26 million in 2050.
Its known that there will be much more older people in 2050 than in 1990, this is the biggest cause of the big raise. [31]
Most of the hip fractures occur in North Europe and in the USA, the regions with the least hip fractures are Latin America and Africa.
In Asia there are an immediate number of hip fractures. But it’s estimated that most of the hip fractures will occur in Asia by 2050. [8]
Age-standardized hip fracture rates (per 100 000 population) across different continents [8]
|
Continent |
Country |
Men |
Women |
|
Africa |
|
|
|
|
|
Rabat |
57.7 |
79.9 |
|
|
Cameroon |
43.7 |
52.1 |
|
Asia |
|
|
|
|
|
Beijing |
87 |
97 |
|
|
Shenyang |
101.3 |
80.9 |
|
|
Korea |
137 |
262 |
|
|
Iran |
127.3 |
164.6 |
|
|
Malaysia |
87.4 |
212.5 |
|
|
Tottori |
107.3 |
297.3 |
|
|
Japan |
99.6 |
368 |
|
|
Kuwait |
216.6 |
316 |
|
|
Singapore |
152 |
402 |
|
|
Hong Kong |
193 |
484.3 |
|
|
Hong Kong |
50 |
110 |
|
|
Taiwan |
233.4 |
496.8 |
|
South America |
|
|
|
|
|
Mexico |
98 |
169 |
|
|
Sobral, Brazil |
59.3 |
168.4 |
|
|
Argentina |
137 |
405 |
|
|
Venezuela |
37 |
98 |
|
Europe |
|
|
|
|
|
Switzeland |
137.8 |
346 |
|
|
Former East Germany |
137.8 |
354.7 |
|
|
Former West Germany |
154.5 |
399.4 |
|
|
England |
143.6 |
418.2 |
|
|
Greece |
201.7 |
469.9 |
|
|
Sweden |
302.7 |
709.5 |
|
|
Norway |
352 |
763.6 |
|
|
Oslo |
399.3 |
920.7 |
|
|
Austria |
567 |
759 |
|
|
Hungary |
223 |
430 |
|
|
The Nederlands |
308 |
669 |
|
North America |
|
|
|
|
|
Minnesota |
201.6 |
511.6 |
|
|
United States |
197 |
516 |
|
Oceania |
|
|
|
|
|
Maori, New Zealand |
197 |
516 |
|
|
Non-Maori |
288 |
827 |
|
|
New South Wales |
191.8 |
475.1 |
|
|
Australia |
187.8 |
504.2 |
Risk factors other than low bone mineral density (BMD), defined by the National Osteoporosis Foundation (National Osteoporosis Foundation, 1998) are personal history of fracture as an adult, history of fracture in a first degree relative, low body weight, and current cigarette smoking.[14]
<span style="font-size: 13.28px; line-height: 19.92px;" />Another risk factor that is frequently discussed for the last years is the proximal femoral geometry. It is suggested as an important marker for the hip fracture risks.[14]
Fractures can be classified radiographically into intracapsular and extracapsular fractures (figure2). These can be further subdivided, depending on the level of the fracture and the presence or absence of displacement and comminution. [14]
About 3% of hip fractures are related to localized bone weakness at the fracture site. Secondary to tumor, followed by bone cysts, or Paget’s disease. More than half of the remaining patients have osteoporosis, and nearly all are osteopenia. [15]
Characteristics/Clinical Presentation[edit | edit source]
Specific features for patients with hip fracture include:[10][11]
- Dull ache in the groin and/or hip region [12] (level of evidence B)
- Inability to put weight on the injured leg causing immobility right after the fall [13] (level of evidence A1)
- If the femur bone is completely broken the injured leg might be shorter compared to the other leg
- Severe pain
- The patient tends to keep the injured hip as still as possible, positioning it in external rotation [13]
- A swelling might occur
Signs and symptoms of a hip fracture include:
- Inability to move immediately after a fall [4]
- Severe pain in your hip or groin [4]
- Inability to put weight on your leg on the side of your injured hip [4]
- Stiffness, bruising and swelling in and around your hip area [4]
- Shorter leg on the side of your injured hip [4]
- Turning outward of your leg on the side of your injured hip [4]
- During the physical examination, displaced fractures present with external rotation and abduction, and the leg will appear shortened. [5] (level of evidence C2)
- Patients with hip fractures have pain in the groin and are unable to bear weight on the affected extremity [5]
- During the physical examination, displaced fractures present with external rotation and abduction, and the leg will appear shortened [5]
Differential Diagnosis[edit | edit source]
A hip fracture diagnosis usually is established based on patient history, physical examination, and plain radiography. A patient with hip fracture typically presents with pain and is unable to walk after a fall. [16]
On physical examination, the injured leg is shortened, externally rotated, and abducted in the supine position. Plain radiographs of the hip (a posteroanterior view of the pelvis and a lateral view of the femur) usually confirm the diagnosis. [16]
However, when clinical suspicion for hip fracture is high and plain radiographs are normal, occult fracture should be ruled out with magneticresonanceimaging (MRI). [16]If MRI is contraindicated, a bone scan may be useful in diagnosing fracture, but results may be normal for up to 72 hours after the injury. [16]
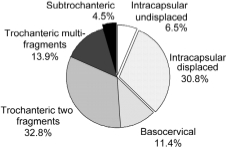
In the scientific research that we use as source, the researchers emphasized different types of hip fractures. [17]
The mean age of the tests subjects (201 in the beginning, 27 patients were lost to follow-up and 32 patients died) is 81,3 years old with a SD of 8,7 years. [17]
The majority of hip fractures are traumatic. Only 1.5% are metastatic fractures. [17]
About 37% of the hip fractures are intracapsular, 58% of the fractures are located in the trochanteric region and less than 5% are subtrochanteric. [17]
Diagnostic Procedures[edit | edit source]
The diagnosis of a hip fracture is established based on patient history, physical examination and radiography.[13]
A patient with hip fracture typically presents with pain and is unable to walk after a fall.Hip fractures encompass a wide range of variety of types and imaging techniques. The most common types of hip fractures include stress fractures and occult fractures (not detectable via radiograph). [3][18][19]
Initially, radiographs are usually taken if fracture is suspected due to ease of use and immediate results. However, radiographs have a poor reliability of picking up fractures in early stages. MRI is considered the gold standard due to high sensitivity in detecting hip fractures. [3][18][19]
The majority of hip fractures are found by plain radiography, the initial imaging modality used in the diagnosis of hip fracture, which has a sensitivity ranging from 90%-95%. Standard x-ray examination of the hip includes an anteroposterior (AP) view of the pelvis and an AP and cross-table lateral view of the involved hip. Plain x-rays without evidence of fracture do not exclude the diagnosis of hip fracture. [3][18][19]
Magnetic resonance imaging (MRI) has become the imaging modality of choice for diagnosing occult hip fractures not detected by radiography. [3][18][19]
MRI has been shown to have 100% sensitivity and 100% specificity in diagnosing occult hip fractures. Another advantage of MRI is its ability to identify other causes of hip pain involving soft tissue injuries and non-femoral pelvic fractures, thus allowing for appropriate, cost-effective treatment. [3][18][19]
Berger et al demonstrated that radiographs had a sensitivity of 15-35% on initial examination of stress fractures, increasing to 30-70% on follow-up visits. The same study also indicated MRI having a specificity of 86%, sensitivity of 100%, accuracy of 95%, positive predictive value of 93%, and negative predictive value of 100%.[3][18][19]
It is suggested that the best method of detecting occult fractures is a combination of a T1 and T2 weighted MRI. This allows the differentiation of fractures versus soft tissue injuries, and is important as it will significantly alter the course of intervention.[3][18][19]
On a MRI one can see that a proximal hip fracture consists many kinds:
Subcapital neck fracture: right below the femoral head
Femoral neck fracture (intracapsular fracture)[20] (level of evidence B)
- Intertrochanteric fracture: between the greater and the small trochanter (extracapsular fracture)[20][11]
- Subtrochanteric fracture: 2 ½ inch below the small trochanter (extracapsular fracture)[11]
- Fracture of the greater trochanter
- Fracture of the small trochanter
Outcome Measures[edit | edit source]
Locomotion (ability to walk and to climb stairs) can be measured with a subscale of the FIM (Functional Independence Measure). It is a predictor for locomotion This test rates the patient's independence in traveling 45 m (150 ft) walking or in a wheelchair and in going up and down 12 to 14 stairs. A higher score on the test represents a better locomotion.
Age and prefracture residence at a nursing home were significant predictors of locomotion (P = .02 for both).[20] (Level of evidence A2)
Early surgery was not associated with improved function and increased mortality. Though it was associated with reduced pain and length of stay. Early surgery also resulted in fewer complications. These conclusions were obtained by comparing patients having surgery within 24 hours with those having surgery after 24 hours on the following outcomes: [21] (Level of Evidence A2)
- Mean pain scores over the first 5 hospital days;
- Number of days of severe and very severe pain over hospital days 1 to 5 (assessed by asking patients if they were experiencing no pain, or mild, moderate, or severe pain);
- Major postoperative complications;
- LOS;
- mortality through 6 months;
- FIM locomotion (a 2-item subscale focusing on walking and climbing stairs) score at 6 months;
- FIM self-care (a 6-item scale of self-care activities including bathing and dressing); and
- FIM transferring (a 3-item scale focusing on transfers from the bed, toilet, and tub).[21] (Level of Evidence A2)
In the study of Diamond TH et al. are the main outcome measures Prognostic factors (such as pre-existing illness and osteoporotic risk factors) and outcome data (such as fracture-related complications, mortality, and level of function as measured by the Barthel index of activities of daily living at six and 12 months postfracture).
The results of these outcome measures are that fracture-related complications affected similar proportions of men and women (30% v. 32%), and mean length of hospital stay was similar. Fourteen per cent of men died in hospital compared with only 6% of women (P = 0.06). Men had more risk factors for osteoporosis (P < 0.01). [22] (Level of evidence C)
Physical functioning (measured by the Barthel index) deteriorated significantly in men from 14.9 at baseline to 13.4 at six months (P < 0.05) and 12.4 at 12 months (P < 0.05) after fracture.[22] (Level of evidence C)
Jay Magaziner et al. investigated eight areas of function after hip fracture. This eight areas of function (i.e., upper and lower extremity physical and instrumental activities of daily living; gait and balance; social, cognitive, and affective function) were measured by personal interview and direct observation during hospitalization at 2, 6, 12, 18, and 24 months.
Levels of recovery are described in each area, and time to reach maximal recovery was estimated using Generalized Estimating Equations and longitudinal data.
Most areas of functioning showed progressive lessening of dependence over the first postfracture year, with different levels of recovery and time to maximum levels observed for each area. New dependency in physical and instrumental tasks for those not requiring equipment or human assistance prefracture ranged from as low as 20.3% for putting on pants to as high as 89.9% for climbing five stairs.
Recuperation times were specific to area of function, ranging from approximately 4 months for depressive symptoms (3.9 months), upper extremity function (4.3 months), and cognition (4.4 months) to almost a year for lower extremity function (11.2 months) [23]
(Level of evidence C)
On physical examination, the injured leg is shortened, externally rotated, and abducted in the supine position. There is little to no external bruising at the fracture site.[3] Plain radiographs of the hip usually confirm the diagnosis. [13]
Examination[edit | edit source]
On physical examination, the injured leg is shortened, externally rotated, and abducted in the supine position. There is little to no external bruising at the fracture site.[3] Plain radiographs of the hip usually confirm the diagnosis. [13]
Medical Management
[edit | edit source]
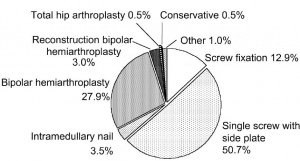
There are many different kinds of operations and treatments if we talk about hip fracture. The sort of operation or treatment that is used is based on the sort of fracture and personal factors. [16]
In the previously used source (16) almost 80% of the subcapital fractures were treated with a cemented bipolar hemiarthroplasty. All but one of the undisplaced subcapital fractures were treated with screw fixation. [16]
Half of the hip fractures were treated with a dynamic hip screw. This represents 87.2% of the fractures in the trochanteric region. Intramedullary nailing was used in less than 4% of the cases. [16]
Cemented bipolar hemiarthroplasties with diaphy- seal support were implanted in six patients with complex inter- or subtrochanteric fractures. [16]
One stable undisplaced subcapital fracture was treated conservatively. (2)
In figure 4 you can find an overview of different type of treatment performed for a hip fracture.[16]
Intracapsular Fractures:
Surgical management is the treatment of choice for the majority of femoral neck fractures, but treatment for nondisplaced femoral neck fractures can be non-operative. [3]
Non operative treatment involves protected weight bearing with crutches for 6 weeks. Non operative repair is usually reserved for patients who present late after a fracture or who have significant comorbidities and a high operative risk. [3]
The treatment of displaced femoral neck fractures is more complex, and surgical repair is usually the treatment of choice. These fractures are not amenable to non-operative management, which should be reserved for patients with extremely high surgical risk or non-ambulatory elderly patients with dementia and very limited life expectancies. [3]
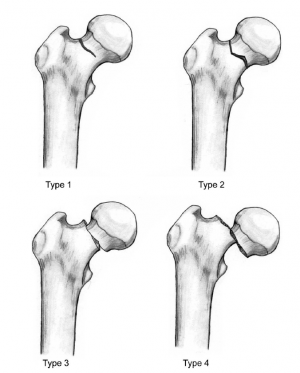
Intracapsular fractures are further classified as nondisplaced or displaced based on radiographic findings. This classification is called: Garden classification (figure 5). [3]
- Type 1: un-displaced and incomplete fracture
- Type 2: un-displaced complete fracture
- Type 3: complete fracture but incompletely displaced
- Type 4: complete fracture and completely displaced
Extracapsular Fractures:
Surgical stabilization is standard treatment, and non-operative measures are only considered for patients who are deemed at very high surgical risk or who have a limited life expectancy.
The goal of surgery is to achieve a stable fracture reduction and fixation, allowing early weight bearing and mobilization of the patient.
Non-operative management is only considered for non-ambulatory patients with minimal pain and for medically unstable patients with major un-correctable comorbid disease or terminal illness [3].
Delirium may be the most common medical complication after hip fracture. Delirium may interfere with recovery and rehabilitation, increase duration of hospitalization, and increase mortality after one year. [16]
Common precipitating factors include electrolyte and metabolic abnormalities, inadequate pain control, infection, and psychoactive medications.
Physicians can help prevent delirium by avoiding polypharmacy, minimizing the use of anticholinergic and psychoactive medications, removing urinary catheters and intravenous lines as soon as possible, and minimizing sleep interruptions.
If delirium occurs, a thorough evaluation and treatment of the underlying cause is needed. Patients who do not respond to conservative measures may benefit from low-dose tranquilizers (e.g., haloperidol [Haldol]) or atypical antipsychotics (e.g., risperidone [Risperdal], olanzapine [Zyprexa]).
These agents should be discontinued as soon as possible after the delirium is resolved [16].
Physical Therapy Management
[edit | edit source]
Prolonged bed rest can increase the risk of pressure sores, atelectasis, pneumonia, deconditioning, and thromboembolic complications. Weight bearing immediately after hip fracture surgery is safe in most patients.[16]
Doing your physical therapy “homework” after a hip fracture can save your life. Within two years of a hip fracture, more than half of men and 40% of women are either dead or living in a long-term care facility.
The sooner you return to daily physical tasks after surgery or being injured, the healthier you’ll be . “Complications following hip surgery involve blood clots, pneumonia, wound infections, and more, all of which can be reduced with activity,” Dr. Salamon says. [27]
Prolonged bed rust can increase the risk of pressure sores and deconditioning. Therefore it’s important to start rehabilitation on the first post-operative day (on patients with a total hip replacement). This includes quadriceps strengthening exercises, isometric exercises, and flexion and extension mobilizations in the hip joint …[13]
On the second and third post-operative day the patient can start with walking between parallel bars, and later on they can walk with a walker or a cane. This walking is supervised.
The physiotherapist will begin with range of motion exercises for the hip, knee and ankle because mobility is decreased following immobilization. Mobilization is a very important treatment in the recovery process.
The patient can also begin strengthening exercises based on the surgeon's orders (typically six weeks post-op). Patients should also undergo balance and proprioceptive rehab and these abilities are quickly lost with inactivity.[28]
Weight-bearing exercises are very important for mobility, balance, activities of daily living and quality of life[5](level of evidence B), examples:
- Stepping in different directions
- Standing up and sitting down
- Tapping the foot and stepping onto and off a block.
It is ordinarily suggested that patients who underwent a prosthetic replacement have to avoid for approximately 12 weeks:[24] (level of evidence 5)
- Hip flexion greater than 70–90°
- External rotation of the leg
- Adduction of the leg past midline
- Should not bend forward from the waist more than 90
The patient training begins the day after surgery from a sitting position, with abducted hip during transfer from bed to chair.[24]
Progressive weight-bearing as tolerated till full weight-bearing should start soon after surgery according to general physical status.[24]
When internal fixation is performed, partial weight-bearing is recommended for a period of 8–10 weeks (according to the radiological evaluation of fracture healing), and after 3 months full weight-bearing should be allowed.[24]
A warming up on a stationary bicycle for 10 to 15 minutes is recommended.[25]
Among patients who had completed standard rehabilitation after hip fracture, the use of a home-based functionally oriented exercise program resulted in modest improvement in physical function at 6 months after randomization.[26] (level of evidence B1)
Program components [26]:
- Hip extension (theraband and manual exercise)
- Heel raises onto toes (theraband and manual exercise)
- Resisted rowing (double arm lifting) (theraband and manual exercise)
- Standing diagonal reach (theraband and manual exercise)
- Modified get up and go (theraband and manual exercise)
- Overhead arm extensions (theraband and manual exercise)
- Repeated chair stands (vest and manual exercise)
- Lunges - forward and back (vest and manual exercise)
- Stepping up and down step (vest, manual exercise and plyometric step)
- Calf raises - both legs and one leg (manual exercise)
Twelve weeks of progressive strength training once a week, as a follow-up to a more intensive training period after hip fracture has no measureable effect upon the BBS (Berg Balance Scale) score, but may improve strength, endurance, self-reported NEADL (The Nottingham Extended Activities of Daily Living score), and self-perceived health.
Home-dwelling hip fracture patients seem to constitute a group that needs prolonged follow-up to achieve the improvements that are important for independent functioning.[25]
Prevention is also a part of the rehabilitation process to prevent fractures. Prevention of hip fractures should focus on preventing falls and osteoporosis.
Several strategies could help reduce the loss of bone density that underlies hip fracture. Among these, a substantial body of evidence indicates that physical activity is the most important, and it is a method of prevention that can be enjoyable and sociable.
Regular exercise would reduce the risk of hip fracture by at least half.
Stopping smoking is also important, and a woman who stops smoking before the menopause will reduce her risk by about a quarter. [29]
Both these policies can be adopted by both sexes and continued into old age. Postmenopausal oestrogen replacement more than halves the risk of hip fracture, but the loss of this protection within a few years of stopping treatment limits its utility.
Oestrogen replacement would need to be continued almost indefinitely if it were to do more than reduce the incidence of hip fracture in younger age groups, in whom hip fracture is uncommon and recovery generally uncomplicated. General calcium supplementation is not justified as the likely benefit is too small.[29]
Interventions to reduce the risk of falls should target identified risk factors (e.g., muscle weakness; history of falls; use of four or more prescription medications; use of an assistive device; arthritis; depression; age older than 80 years; impairments in gait, balance, cognition, vision, or activities of daily living).(26)
Key Research[edit | edit source]
add links and reviews of high quality evidence here (case studies should be added on new pages using the case study template)
Resources
[edit | edit source]
http://www.sint-trudo.be/downloads/Behandeling%20heupfracturen.pdf
https://en.wikipedia.org/wiki/Hip_fracture
https://en.wikipedia.org/wiki/Hip_replacement
Clinical Bottom Line[edit | edit source]
The amount of hip fractures worldwide will increase up to 7-21 million incidences each year in 2050. [31]
Mortality associated with a hip fracture is about 5-10% after one month. One year after fracture about a third of patients will have died, compared with an expected annual mortality of about 10% in this age group. [31]
Thus, only a third of the deaths are directly attributable to the hip fracture itself, but patients and relatives often think that the fracture has played a crucial part in the final illness. More than 10% of survivors will be unable to return to their previous residence. [31]
Most of the remainder will have some residual pain or disability. Most people who sustain the injury require surgery followed by a period of rehabilitation. [31]
Treatment is generally surgical to replace or repair the broken bone. [31]
Some loss of function is to be expected in most patients. Some loss of function is to be expected in most patients.[31]
Recent Related Research (from Pubmed)[edit | edit source]
http://www.physio-pedia.com/Diagnostic_Imaging_of_the_Hip_for_Physical_Therapists
http://www.physio-pedia.com/Acetabulum_fracture
http://www.physio-pedia.com/Femur
http://onlinelibrary.wiley.com.ezproxy.vub.ac.be:2048/doi/10.1002/pds.3863/full
https://bmcmusculoskeletdisord.biomedcentral.com/articles/10.1186/s12891-016-0988-9
References[edit | edit source]
1.↑ ANTAPUR ET AL. Fractures in the elderly: when is a hip replacement a necessity? Clinical Interventions in Aging. 2011
2. ↑ KAPANDJI I.A. Bewegingsleer Deel II De Onderste Extremiteit. Bohn Stafleu Van Loghum. Houtem/Diegem 1986
3. Bateman, Laura, et al. "Medical management in the acute hip fracture patient: a comprehensive review for the internist." The Ochsner Journal 12.2 (2012): 101-110. (Level of Evidence B2)
4. http://www.mayoclinic.org/diseases-conditions/hip-fracture/basics/symptoms/con-20021033 (visited on march 2016)
5. EDWARD LeBLANC, K. I. M., and LEANNE L. LeBLANC. "Hip fracture: diagnosis, treatment, and secondary prevention." American family physician89.12 (2014).(level of evidence C2)
6. Grisso, Jeane Ann, et al. "Risk factors for falls as a cause of hip fracture in women." New England Journal of Medicine 324.19 (1991) (level of evidence 2A)
7. Melton, LJd. "Hip fractures: a worldwide problem today and tomorrow." Bone 14 (1993): 1-8. (level of evidence 2A)
8. Dhanwal, Dinesh K., et al. "Epidemiology of hip fracture: Worldwide geographic variation." Indian journal of orthopaedics 45.1 (2011): 15. (level of evidence 2A)
9. ↑ 7.0 7.1 http://www.mayoclinic.com/health/hip-fracture/DS00185/DSECTION=risk-factors (visited on april 2016)
10. ↑ 9.0 9.1 9.2 http://orthoinfo.aaos.org/topic.cfm?topic=A00392 (visited on april 2011)
11. ↑ DORNE and LANDER. Spontaneous Stress Fractures of the Femor Neck. AJA 144:343-347, February 1985
12. ↑ 11.0 11.1 11.2 11.3 11.4 SHOBHA S. RAO, M.D., and MANJULA CHERUKURI, M.D. Management of Hip Fracture: The Family Physician’s Role. www.aafp.org/afp Volume 73, Number 12, June 15, 2006
13. Dinçel, V. Ercan, et al. "The association of proximal femur geometry with hip fracture risk." Clinical Anatomy 21.6 (2008): 575-580. (Level of Evidence B3)
14. Parker, Martyn, and Antony Johansen. "Hip fracture." British Medical Journal 7557 (2006): 27. (Level of Evidence A3)
15. Rao, Shobha S., and Manjula Cherukuri. "Management of hip fracture: the family physician’s role." Am Fam Physician 73.12 (2006): 2195-2200. (level of evidence 2A)
16. Scheerlinck, T., et al. "Hip fracture treatment: outcome and socio-economic aspects: a one-year survey in a Belgian university hospital." Acta orthopaedica belgica 69.2 (2003): 145-156(level of evidence 2A)
17. Berger FH, de Jonge MC, Maas M. Stress fractures in the lower extremity. The importance of increasing awareness amongst radiologists. European journal of radiology. 2007;62(1):16-26. Available at: (level of evidence 2A)
18. http://www.physiopedia.com/Diagnostic_Imaging_of_the_Hip_for_Physical_Therapists
19. ↑ 12.0 12.1 12.2 LANCE C. BRUNNER,M.D., and LIZA ESHILIAN-OATES,M.D. Hip Fractures in Adults. www.aafp.org/afp February 1, 2003 Volume 67, Number 3
20. EDWARD L HANNAN ET AL., Mortality and Locomotion 6 Months After Hospitalization for Hip FractureRisk Factors and Risk-Adjusted Hospital Outcomes
(Level of Evidence A2)
21. GRETCHEN M OROSZ ET AL., Association of Timing of Surgery for Hip Fracture and Patient Outcomes. JAMA. 2004;291(14):1738-1743.
(Level of Evidence A2)
22. DIAMOND TH ET AL., Hip fracture in elderly men: prognostic factors and outcomes. The Medical Journal of Australia [1997, 167(8):412-415]
(Level of Evidence C)
23. JAY MAGAZINER ET AL., Recovery From Hip Fracture in Eight Areas of Function. Journal of Gerontology: MEDICAL SCIENCES 2000, Vol. 55A, No. 9, M498–M507.
(Level of Evidence C)
24. Luciani, D., et al. "The importance of rehabilitation after lower limb fractures in elderly osteoporotic patients." Aging clinical and experimental research 25.1 (2013): 113-115. (level of evidence 5)
25. Sylliaas, Hilde, et al. "Progressive strength training in older patients after hip fracture: a randomized controlled trial." Age and ageing (2011): afq167. (level of evidence 2A)
26. Latham, Nancy K., et al. "Effect of a home-based exercise program on functional recovery following rehabilitation after hip fracture: a randomized clinical trial." Jama 311.7 (2014): 700-708. (Level of evidence B1)
27. Daniel Pendick. ‘’After hip fracture, exercise at home boosts day-to-day function’’ Harvard health publication (2014) (level of evidence 2A)
28. http://www.physio-pedia.com/Femoral_Fractures,
29. Mr Law et al. ‘’Strategies for prevention of osteoporosis and hip fracture’’ (1991) 453-459 (level of eveidence 2A)
30. http://pmmp.cnki.net/Resources/CDDPdf/evd/200801/British%20Medical%20Journal/%E4%B8%B4%E5%BA%8A%E5%AE%9E%E8%B7%B5%E6%8C%87%E5%8D%97/bmj20063330727.pdf) (Level of evidence A1)
31. Kannus, P., et al. "Epidemiology of hip fractures." Bone 18.1 (1996): S57-S63. (level of evidence 2A)