Dry Needling
Original Editor - Ajay Upadhyay
Top Contributors - Sehriban Ozmen, Gayatri Jadav Upadhyay, Daniele Barilla, Irene Leahy, Kim Jackson, Lilian Ashraf, Admin, Redisha Jakibanjar, Melissa Coetsee, WikiSysop, Candace Goh, Claire Knott, Riccardo Ugrin, Rishika Babburu and Bruno Serra
Description[edit | edit source]
Trigger-point dry needling is an invasive procedure where a fine needle or acupuncture needle is inserted into the skin and muscle. It is aimed at myofascial trigger points (MTrP) which are hyperirritable spots in skeletal muscle that are associated with a hypersensitive palpable nodule in a taut band.[1] Trigger point dry needling can be carried out at superficial or deep tissue level.
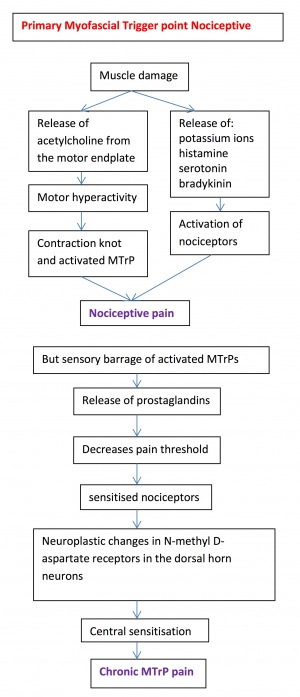
Pathophysiology of MTrPs[edit | edit source]
Trigger points are thought to be due to an excessive release of acetylcholine from selected motor endplates. They can be divided into Active and Latent myofascial trigger points.
- Active trigger points can spontaneously trigger local or referred pain. They cause muscle weakness, restricted ROM and autonomic phenomena.
- Latent trigger points do not cause pain unless they are stimulated. They may alter muscle activation patterns and contribute to restricted ROM.
- Therefore both active and latent trigger points cause allodynia at the trigger point site and hyperalgesia away from the trigger point following applied pressure.[2]
- The formation of trigger points is caused by the creation of a taut band within the muscle. This band is caused by excessive acetylcholine release from the motor endplate combined with inhibition of acetylcholine esterase and upregulation of nicotinic acetylcholine receptors.
- Initially taut bands are produced as a normal protective, physiological measure in the presence of actual or potential muscle damage. They are thought to occur in response to unaccustomed eccentric or concentric loading, sustained postures and repetitive low load stress. However when sustained they contribute to sustained pain.
- Pain caused by trigger points is due to hypoxia and decreased bloodflow within the trigger point. This leads to a decreased pH which activates the muscle nociceptors to restore homeostasis. This causes peripheral sensitization.
- Trigger points are also involved in central sensitization. The mechanism remains unclear but trigger points maintain nocioceptive input into the dorsal horn and therefore contribute to central sensitization.
Deep VS Superficical Dry Needling[edit | edit source]
Superficial dry needling involves inserting the needle up to 10 mm into the subcutaneous tissue, its benefits include ease of administration, decreased risk of significant tissue trauma, reduced risk of nerve and visceral injury and patient comfort.
Deep dry needling involoves the insertion of the needle beyond the subcutaneous tissue into the muscle with the intention of reaching myofascial trigger points.[3]
Mechanisms of Action[edit | edit source]
Dry needling has been shown to immediately increase pressure pain threshold and range of motion, decrease muscle tone, and decrease pain in patients with musculoskeletal conditions.[4] Its suggested mechanisms of action include:
Local Twitch Response: Dry needling can elicit ‘local twitch response’ which is an involunatary spinal reflex resulting in a localized contraction of the affected muscles that are being dry needled. Local twitch response can lead to alteration in the length and tension of muscles fibers and stimulate mechanoreceptors like A Beta fibers.[5]
Effects on Blood Flow: Sustained contraction of taut muscle bands in trigger points might cause local ischemia and hypoxia. Dry needling causes vasodialation in the small blood vessels leading to increased muscle blood flow and oxygenation.[5]
Neurophysiological effects: Dry needling may produces local and centeral nervous responses to restore hemostasis at the site of the trigger point which results in reduction in both centeral and peripheral sensitization to pain.[4]
Remote Effects: Dry needling of distal MTrP has been found to have analgesic effect on proximal MTrP. The literature has conflicting evidence regarding the contralateral effect.[5]
Placebo Effect
Indication[edit | edit source]
Dry needling may be indicated for myofascial pain with the presence of trigger points. Dry needling has also been shown to be beneficial for the management of strains, osteoarthritis and tendinopathies.[6]
Contradindications[edit | edit source]
Absolute contraindications[8]
DN therapy should be avoided in patients under the following circumstances[9][10]:
- In a patient with needle fobia.
- Patient unwillng - fear, patient belief.
- Unable to give consent - communication, cognitive, age-related factors.
- Medical emergency or acute medical condition.
- Over an area or limb with lymphedema as this may increase the risk of infection/cellulitis and the difficulty of fighting the infection if one should occur.
- Inappropriate for any other reason.
Relative Contraindications[8]
- Abnormal bleeding tendency
- Compromised immune system
- Vascular disease
- Diabetes
- Pregnancy
- Children
- Frail patients
- Patients with epilepsy
- Phychological status
- Patient allergies
- Patient medication
- Unsuitable patient for any reason
Evidence[edit | edit source]
The effectiveness of this treatment depends greatly on the skill of the therapist to accurately palpate mysofascial trigger points as well as kinaesthetic awareness of the anatomical structures.
A cochrane review (2005) of RCTs concluded that trigger point dry needling may be beneficial for low back pain when used in combination with other treatments. However further higher quality studies are needed to confirm this.[11]
A Crossover study (2016) on the Effect of Dry Needling on Spasticity, Shoulder Range of Motion, and Pressure Pain Sensitivity in Patients With Stroke, concluded that dry-needling decreased localized pressure sensitivity and improving shoulder range of motion in individuals who had experienced stroke, with no significant effect on spactisity.[12]
A systematic review of 23 trials considering needling therapies for myofascial trigger point pain concluded that direct dry-needling (where MTrPs were directly targetted) was as benificial as wet needling.[13] There is no clear evidence that it is beneficial above placebo. More studies of higher quality with a reproducible diagnostic criteria and a valid placebo are needed to draw firm conclusions on this.
A systematic review and meta analysis with level 1a evidence suggests that:[14]
- Very low–quality to moderate quality evidence suggests that dry needling performed by physical therapists is more effective than no treatment, sham dry needling, and other treatments for reducing pain and improving pressure pain threshold in patients presenting with musculoskeletal pain in the immediate to 12-week follow-up period.
- Low-quality evidence suggests superior outcomes with dry needling for functional outcomes when compared to no treatment or sham needling.
- No difference in functional outcomes exists when compared to other physical therapy treatments.
- Evidence of long-term benefit of dry needling is currently lacking.
Electrical Dry Needling[edit | edit source]
Electrical dry needling (EDN) is a technique in which two needles are inserted as electrodes for passing an electric current. One of the main advantages in using EDN in clinical practice or acupuncture research is its capacity to set stimulation frequency and intensity objectively and quantifiably.
In clinical practice, both low- and high-frequency electrostimulation are used often for diverse conditions. Low-frequency stimulation is specifically recommended for muscular atrophy [15], whereas highfrequency stimulation is recommended for spinal spasticity[16].On animals for example EDN with 2-Hz stimulation seems to induce acupuncture analgesia by the release of endomorphin, β-endorphin and enkephalin binding to μ and δ opioid receptors. EDN with 100-Hz stimulation, however, enhances the release of dynorphin binding to the opioid receptor in the spinal cord dorsal horn to produce acupuncture analgesic effect[17].
Most studies demonstrated a broad neuromatrix response that involved the limbic system and limbic-related brain structures including the amygdala, hippocampus, hypothalamus, cingulate, prefrontal and insular cortices, basal ganglia, and cerebellum[17]. On human infact results demonstrated greater effect on the limbic and limbic-related brain structures with real EDN than with nonspecific or placebo stimulation. Specifically, the hemodynamic response produced signal increase in notable limbic-related regions such as the insula, thalamus, cerebellum, and the anterior middle cingulate cortex. Interestingly, however, the subgenual anterior cingulate showed signal decrease[18].
Clinical Relevance[edit | edit source]
- The inclusion of electrical dry needling into a manual therapy and exercise program was more effective for improving pain, function, and related-disability than the application of manual therapy and exercise alone in individuals with painful knee osteoarthritis.[19]
- The inclusion of electrical dry needling into a program of manual therapy, exercise and ultrasound was more effective for improving pain, function and related-disability than the application of manual therapy, exercise and ultrasound alone in individuals with patello-femoral pain at mid-term (3 months).[20]
- EDN and upper cervical and upper thoracic HVLA thrust spinal manipulation were shown to be more effective than nonthrust mobilization and exercise in patients with cronic headache, and the effects were maintained at 3 months. [21]
- EDN combined with cervicothoracic manipulation c resulted in greater reductions in pain, disability, and medication intake than nonthrust peripheral joint/soft tissue mobilization, exercise, and interferential current in patients with subacromial pain syndrome . The effects were maintained at 3 months.[22].
References[edit | edit source]
- ↑ Dommerholt, J., Del Morel, O. and Grobli, C. Trigger point dry needling. The journal of manual and manipulative therapy 2006;14(4), 70-87
- ↑ Dommerholt, J. Dry-needling-peripheral and central considerations. Journal of manual and manipulative therapy. 2011;19(4), 223-238
- ↑ Griswold D, Wilhelm M, Donaldson M, Learman K, Cleland J. The effectiveness of superficial versus deep dry needling or acupuncture for reducing pain and disability in individuals with spine-related painful conditions: a systematic review with meta-analysis. Journal of Manual & Manipulative Therapy. 2019 May 27;27(3):128-40.
- ↑ 4.0 4.1 Gattie E, Cleland JA, Snodgrass S. The effectiveness of trigger point dry needling for musculoskeletal conditions by physical therapists: a systematic review and meta-analysis. Journal of Orthopaedic & Sports Physical Therapy. 2017 Mar;47(3):133-49.
- ↑ 5.0 5.1 5.2 Cagnie B, Dewitte V, Barbe T, Timmermans F, Delrue N, Meeus M. Physiologic effects of dry needling. Current pain and headache reports. 2013 Aug;17(8):1-8.
- ↑ McAphee D, Bagwell M, Falsone S. Dry Needling: A Clinical Commentary. International Journal of Sports Physical Therapy. 2022;17(4):551.
- ↑ Tim Trevail. Dry Needling: Trapezius. Available from: https://www.youtube.com/watch?v=MB4mVDqU1y0
- ↑ 8.0 8.1 Dommerholt J., Fernandez-de-las-Penas C. Trigger Point Dry Needling. An Evidenced and Clinical-Based Approach. Edinburgh: Churchill Livingstone-Elsevier, 2013
- ↑ Australian Society of Acupunture Physioterapists Inc. Guidelines for safe acupuncture and dry needling practice, 2007.
- ↑ White, A., Cummings M., Filshie, J. Evidence of safety of acupuncture. An introduction to Western medical acupuncture. Edinburgh: Churchill Livingstone, 2008.
- ↑ Furlan AD, van Tulder MW, Cherkin D, Tsukayama H, Lao L, Koes BW, Berman BM. Acupuncture and dry-needling for low back pain. Cochrane Database of Systematic Reviews 2005, Issue 1.
- ↑ Ana Mendigutia-Gómez, PT, PhD, Carolina Martín-Hernández, PT, Jaime Salom-Moreno, PT, PhD, César Fernández-de-las-Peñas, PT, PhD. Effect of Dry Needling on Spasticity, Shoulder Range of Motion, and Pressure Pain Sensitivity in Patients With Stroke: A Crossover Study. DOI: http://dx.doi.org/10.1016/j.jmpt.2016.04.006
- ↑ Cummings, T.M. and White, A.R. Needle therapies in the management of myofascial trigger point pain: a systematic review. Achive of physical medicine and rehabilitation 2011;82, 986-992
- ↑ Gattie E, Cleland JA, Snodgrass S. The effectiveness of trigger point dry needling for musculoskeletal conditions by physical therapists: a systematic review and meta-analysis. journal of orthopaedic & sports physical therapy. 2017 Mar;47(3):133-49.
- ↑ Liu G.Techniques of acupuncture and moxibustion. Beijing: Huaxia Publishing House. 1998:177 p.
- ↑ Yuan Y, Yan S, Chen X, Han JS X: The effect and mechanism of electroacupuncture in treating spinal spasticity: a clinical study. Nat Med J Chin, 1992;73:5932.
- ↑ 17.0 17.1 Napadow V, Makris N, Liu J, Kettner NW, Kwong KK, Hui KK. Effects of electroacupuncture versus manual acupuncture on the human brain as measured by fMRI. Hum Brain Mapp. 2005; 24: 193-205
- ↑ Wu MT, Sheen JM, Chuang KH, Yang P, Chin SL, Tsai CY, Chen CJ, Liao JR, Lai PH, Chu KA, Pan HB, Yang CF. Neuronal specificity of acupuncture response: a fMRI study with electroacupuncture. Neuroimage, 2002; 16:1028 –1037.
- ↑ Dunning J, Butts R, Young I, Mourad F, Galante V, Bliton P, Tanner M, Fernández-de-Las-Peñas C. Periosteal Electrical Dry Needling as an Adjunct to Exercise and Manual Therapy for Knee Osteoarthritis: A Multicenter Randomized Clinical Trial. Clin J Pain. 2018 Dec;34(12):1149-1158.
- ↑ Dunning J, Butts R, Henry N, Mourad F, Brannon A, Rodriguez H, Young I, Arias-Buría JL, Fernández-de-Las-Peñas C. Electrical dry needling as an adjunct to exercise, manual therapy and ultrasound for plantar fasciitis: A multi-center randomized clinical trial. PLoS One. 2018 Oct 31;13(10)
- ↑ Dunning J, Butts R, Zacharko N, Fandry K, Young I, Wheeler K, Day J, Fernández-de-Las-Peñas C. Spinal manipulation and perineural electrical dry needling in patients with cervicogenic headache: a multicenter randomized clinical trial. Spine J. 2021 Feb;21(2):284-295
- ↑ Dunning J, Butts R, Fernández-de-Las-Peñas C, Walsh S, Goult C, Gillett B, Arias-Buría JL, Garcia J, Young IA. Spinal Manipulation and Electrical Dry Needling in Patients With Subacromial Pain Syndrome: A Multicenter Randomized Clinical Trial. J Orthop Sports Phys Ther. 2021 Feb;51(2):72-81.