Differentiating Buttock Pain and Sacroiliac Joint Disorders
Original Editors - Jessie Tourwe
Top Contributors - Mariam Hashem, Kim Jackson, Tarina van der Stockt, Lucinda hampton, Ewa Jaraczewska and Jess Bell
Where is the problem?[edit | edit source]
Gluteal or Buttock pain can be triggered by many causes such as[1]:
- Radicular pain from Lumbar spine origin
- Sciatic nerve entrapment
- Obturator internus/gemellus syndrome
- Piriformis Syndrome
- Quadratus femoris/ischiofemoral pathology
- Problems at the hamstrings
- Gluteal muscles disorders
The complicated anatomy of the SIJ, the Lumbar spine and the buttock area makes the differential diagnosis of pain and dysfunction a challenge. MRI findings are not consistent with LBP history and symptoms[2].
Considerations[edit | edit source]
The presence of chronic pain is not always caused by biopsychosocial causes. Missing the primary structural sources of the pain can lead to catastrophisation and development of fear avoidance and anxiety. Factors such as sleep, hormonal balance, smoking, the presence of comorbidities and activity level have an influence on their perception of the pain and the development of chronicity. The mangement shouldn't focus only on the biospychosocial aspects without ignoring the structural causes.
Impingement of the sciatic nerve occurs mostly in the deep gluteal space and around the piriformis muscle than in the lumbar spine level.
Anatomy[edit | edit source]
The Sacroiliac joint is the joint connection between the spine and the pelvis formed by the fusion of the three bones of the pelvis: the ilium, ischium, and pubic bone[3]. The sacroiliac joint has different functions such as load transfer between the spine and the lower extremities and shock absorption for the spine above and converts torque from the lower extremities into the rest of the body[4].
This region is surrounded by and covered with the dorsal sacral nerve, the iliolumbar ligament, the dorsal sacral ligaments, the erector spinae fascia, which is part of the thoraco-lumbar fascia which makes the palpating specific structures difficult[5].
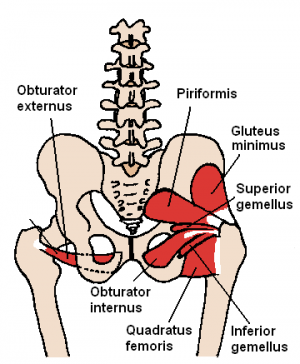
The subgluteal space is located between the middle and deep gluteal aponeurosis layers. It contains Superior/Inferior gluteal nerves, blood vessels, Ischium, Sacrotuberous/sacrospinous ligaments, Sciatic nerve and Piriformis. The piriformis muscle is innervated by the branches of the L5, S1, and S2 spinal nerves. The sciatic nerve has a complicated relationship with the piriformis muscle, passing above, below and through the muscle before and after dividing[1].
Ruling Out the Lumbar Spine[edit | edit source]
Red Flags are serious pathology and should be spotted on the first contact.
spondyloarthropathies and other inflammatory conditions at the lumbar spine level could possibly refer pain to the buttock area. Patients with Ankylosing spondylitis or Reiter's syndrome may present with inflammatory bowel diseases, such as Diverticulitis or Chrohn's disease, prolonged severe morning stiffness, bilateral enthesopathies such as Achilles tendinopathy or plantar fasciitis.
Gynaecological problems, potential infectious diseases, possible malignancies and patients not responding to physiotherapy management can possibly reflect the presence of serious pathologies[5].
Ruling Out the Sacroiliac Joint[edit | edit source]
The thoracolumbar fascia sacroiliac joint, Glute max, Glute min, Piriformis, Obturator Externus and Internus, Gemelli's Superior and Inferior, ischio-gluteal bursa, the long dorsal ligament, sacrotuberous ligament, sacrospinous ligament and the posterior capsule of the hip are all nociceptive structures that can trigger posterior hip pain.
Numerous neural structures can also be involved such as the dorsal sacral nerve, the lumbosacral plexus, including the sciatic nerve and the pudendal nerve which can be highly implicated in sexual dysfunction and pelvic floor dysfunction.
Any pain from the sacroiliac joints or the surrounding myofascial, nerve or neural structures, connective tissues and ligament structures is considered Sacroiliac dysfunction.
This pain could be gradual, due to maladaptive postures, seronegative spondyloarthropathies, osteoarthritis, pregnancy-related pain, or sudden often due to sudden movement, strain or trauma, for example, missing a step or unilateral loading with a twist which can be accompanied by a click,
Symptoms vary from difficulties with standing, walking, walking up the stairs, squatting getting out of the car, turn in bed which causes sleep disturbance.
Psychosocial factors can influence the presentation and the symptoms.
Pain can refer to the pubic symphysis, the groin, the coccyx , and the posterior thigh.
Other associated symptoms: pelvic organ dysfunction, such as urinary incontinence, prolapse, or constipation and sexual dysfunction, It can also be associated with respiratory distress such as aberrant breathing patterns. There is some suggestion of links of the lateral erector spinae, such as iliocostalis linking T12 to L1 down onto the sacrum.
Special Tests[edit | edit source]
March test was validated by Hungerford in 2004. The validation study was published before much was known about other nociceptive structures or pathological structures there are in the lumbar spine or in the buttock. The March test is a load transfer test of the ability of the pelvic girdle to transfer a load when lifting the opposite leg, A positive test however doesn't show where the failure of load transfer happened (on which level).
Active straight leg raise test. Is used clinically to isolate the sacroiliac joint. Often there is a palpable lump over the affected side which still doesn't indicate the SIJ involvement. So the pain could be arising from the joint, the fascia, the ligament, the nerve, all of them, some of the above, or none of the above.
Same applies to Laslett's composite tests and tests that are based on palpation or positional faults
X-rays don't rule out which tissue is involved.
Sacroiliac Joint Infiltration can ease the symptoms when injecting an anesthetic, it doesn't differentiate what the pathological structure is.
The one-legged squat test, femoral glide test. passive accessory tests: AP glide and the longitudinal glide to assess stability at the joint. However, these tests are unvalidated but you can compare glide within the same patient between the right and left sides.
The active straight leg raise test is a validated test but doesn't rule out other pelvic girdle dysfunctions
The Pelvic joint compression with the use of a sacroiliac belt can be very helpful to help control and increase force closure across that lumbar-pelvic area.
Management[edit | edit source]
The language we use is important. Diagnosing the joint as locked, out of alignment, or positional fault which is not supported by evidence. Patients often develop fears and anxieties in response to the beliefs explained by the physiotherapists and consequently catastrophise their symptoms. of the patient.
A suggested alternative is explaining the symptoms to the patient using motor control examples, fr xample:, here is a little bit of less control around this region and we need to restore it.
Ruling Out Gluteal Tendinopathy[edit | edit source]
Pain originates from Glute med and min inserting onto the superior aspect of the greater trochanter.
Ruling Out Deep Gluteal pathology[edit | edit source]
symptoms are mainly located in the inferior gluteal aspect '' retro-trochanteric'' between the ischial tuberosity and the surrounding structures radiating onto the back of the greater trochanter.
The pain might also be originating at the lesser trochanter which could possibly reflect ischio-femoral impingement,
Resources[edit | edit source]
References[edit | edit source]
- ↑ 1.0 1.1 Carro LP, Hernando MF, Cerezal L, Navarro IS, Fernandez AA, Castillo AO. Deep gluteal space problems: piriformis syndrome, ischiofemoral impingement and sciatic nerve release. Muscles, ligaments and tendons journal. 2016 Jul;6(3):384.
- ↑ Tonosu J, Oka H, Higashikawa A, Okazaki H, Tanaka S, Matsudaira K. The associations between magnetic resonance imaging findings and low back pain: A 10-year longitudinal analysis. PLoS One. 2017 Nov 15;12(11):e0188057.
- ↑ Dutton M. Orthopaedic Examination, Evaluation, and Intervention. 2nd ed. New York: McGraw Hill, 2008.
- ↑ Sacroiliac Joint. Physiopedia Page (last accessed 20/09/2020) Available from: https://physio-pedia.com/Sacroiliac_Joint#cite_note-Dutton-2
- ↑ 5.0 5.1 Bell-Jenje T. Differentiating Buttock Pain and Sacroiliac Joint Disorders. Physioplus Course 2020