Crohn's Disease
Original Editors - Sarah Bailey from Bellarmine University's Pathophysiology of Complex Patient Problems project.
Top Contributors - Sarah Bailey, Laura Ritchie, Lucinda hampton, Admin, Kim Jackson, Dave Pariser, WikiSysop, Sehriban Ozmen, Elaine Lonnemann, Wendy Walker, Manisha Shrestha and 127.0.0.1
Introduction[edit | edit source]
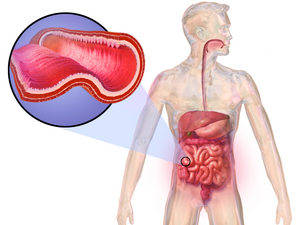
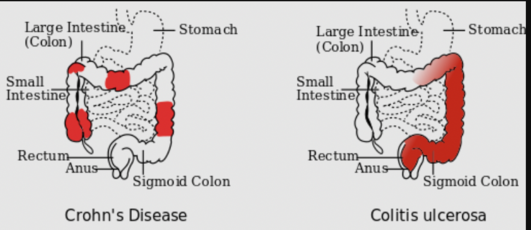
Crohn disease (CD) and ulcerative colitis (UC) are both conditions commonly referred to as inflammatory bowel disease (IBD). CD causes chronic inflammation of the gastrointestinal tract. In Crohn disease, the inflammation extends through the entire thickness of the bowel wall from the mucosa to the serosa.
CD is a serious chronic inflammatory disorder that is difficult to diagnose and manage. The disease has a relapsing and remitting course. Many relapses can cause Crohn disease to progress from mild to moderate to severe penetrating (fistulization) or stricturing disease. There is no cure and most patients experience a poor quality of life..[1]
Etiology[edit | edit source]
The cause of CD is not known but genetics seem to play a role as does the environmental affects on the immune system.
The gut bacteria of people with Crohn’s disease changes but it still isn’t clear if the change is caused by inflammation.
Possibly a diet full of highly processed foods like sugary drinks and fast food, may increase the risk of developing Crohn’s. Crohn’s is not infectious. [2]
Epidemiology[edit | edit source]
CD is most prevalent in the western developed world in North America, northern Europe, and New Zealand.
The incidence of CD is bimodal with the onset occurring most frequently between ages 15 to 30 years and 40 to 60 years old.
It is more prominent in urban than rural areas.[1]
| [3] |
Symptoms of Crohn’s Disease[edit | edit source]
While Crohn’s is a chronic disease, the patients will experience bouts of flare ups and remission with the absence of symptoms [4]. About 50% of individuals with Crohn’s Disease will have mild symptoms. The other half may experience more severe symptoms and pain that appears to come and go. These patients undergo painful exacerbations and potentially symptom free remissions. The remissions might last for months to years but the symptoms will eventually return[4]. This unpredictable nature is part of what makes Crohn's so complicating. Typical symptoms include:
- Diarrhea
- Abdominal cramping generally in the right lower quadrant [5]
- Fever
- Potential rectal bleeding. The rectal bleeding is potentially due to tears or fissures within the anus lining.
- Fistulas or tunnels leading from the intestines to the bladder, vagina or skin may also occur, while most occur around the anal area. The fistula has potential to produce drainage, pus, mucus or stool being excreted from the opening. These symptoms may vary between individuals and may not all be present at the same time.
- Weight loss
- Fatigue [4]
- Perianal lesions
- Stunted growth in children
- Extraintestinal manifestations [6]
Types of Crohn's Disease[edit | edit source]
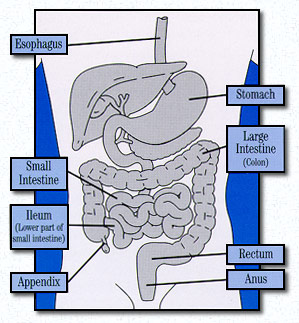
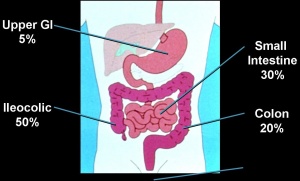
There are different types of Crohn’s Disease dependent upon the location and disease pattern within the GI tract. The different locations of Crohn’s Disease include:
- Gastroduodenal Crohn’s Disease: Located in the upper gastrointenstinal tract and affects the stomach and first part of the small intestine (duodenum). This is uncommon and symptoms occur in 5% of those diagnosed with Crohn’s.
- Jejunoileitis: This is also uncommon in the general population of those diagnosed with Crohn’s disease. Inflammation is located in the Jejunum or Second part of small intestines.
- Ileitis: Inflammation located in the last part of small intestine or ileum and affects 30% of individuals diagnosed with Crohn’s disease.
- Ileocolitis: This is the most common form of Crohn’s disease and affects 50% of those diagnosed with inflammation located in the ileum and colon.
- Crohn’s Colitis: This affects 20% of individuals diagnosed with Crohn’s disease with inflammation located in the colon. The perianal disease and extraintestinal complications are more commonly associated in these individuals.
- Perianal Disease: This occurs in 1/3 of individuals diagnosed with Crohn’s disease. These individuals can have fistulae, fissures, abscesses or skin tags (fleshy growths outside the anus) [6]
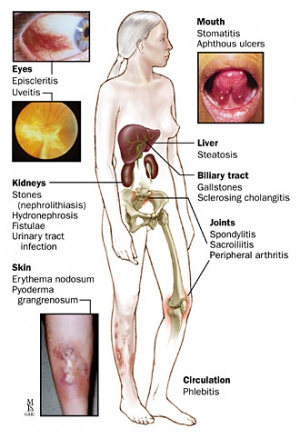
Complications[edit | edit source]
CD is a systemic disease and has manifold intestinal and extra-intestinal complications. Examples include:
- Stricture formation, fistulae and abscesses
- Colorectal carcinoma
- Ankylosing spondylitis
- Erythema nodosum, pyoderma gangrenosum
- Kidney and gall stones
- Anemia
- Hypercoagulable state
- Osteoporosis
- Eye inflammation[1]
Diagnosis[edit | edit source]
The diagnosis of Crohn’s disease is made by ruling out other potential causes to explain the patient’s signs and symptoms. Investigations help to work out which parts of the bowel are affected to determine the best treatment options. Some of the tests include blood tests, fecal occult blood test (FOBT), colonoscopy, flexible sigmoidoscopy, barium enema or small bowel imaging, CT of the GI tract, or a capsule endoscopy.[6]
Most CD patients who develop complications require surgery and as the disease progresses, some need multiple procedures. Once a patient has had surgery, surveillance endoscopy is recommended in six to 12 months. If there is no endoscopic recurrence, ileocolonoscopy should be repeated in 1 to 3 years.[1]
Treatment/Management[edit | edit source]
The medical treatment is roughly grouped into two classes:
- Mild to moderate disease can be treated by oral mesalamine, immunomodulators, methotrexate, and steroids.
- Moderate to severe disease will be best treated using a combination of immunomodulators and biologics or biologics alone.
Dietician involvement is recommended and nutritional supplementation are highly recommended before and during the treatment of Crohn disease.
Physical Therapy Management[edit | edit source]
Crohn’s disease is associated with periumbilical pain and referred low back pain. Individuals may also experience pain in the lower right quadrant and potential associated iliopsoas abscess due to an inflammatory mass that may create hip, buttock, thigh, or knee pain. When a patient presents to physical therapy with unknown origin of low back, sacroiliac or hip pain, it is vital for the therapist to screen for potential organic sources of the pain and is even more important in patients with a history of inflammatory bowel disease.
Since individuals with Crohn’s disease might also have associated low bone mineral content and a high potential for osteoporosis, it is important for the therapist to provide education on osteoporosis and its prevention.
Hydration is very important in patient’s with Crohn’s disease so the therapist should be aware of signs of dehydration, including headache, dry lips, brittle nails and hair, dry hands and disorientation.
Due to the complexity of Crohn’s Disease, patients might be predisposed to emotional stress that could exacerbate the prior symptoms. In knowing this, the therapist has the availability to accept the patient’s feelings, validate the disease to the patient as well as prescribing an exercise program to better the outcome for the patient. These exercises have the ability to boost the immune system, reduce depression, and improve the body image of the patient. In addition to providing this exercise program, therapists can better create coping mechanisms as well as techniques to manage the unexpectedness of Crohn’s Disease[8].
Outcome Measures[edit | edit source]
An outcome measure has been created to track the progress or lack of progress for individuals affected with Crohn’s disease called Crohn’s Disease Activity Index (CDAI). A score below 150 indicates a better prognosis than higher scores. This measure helps to track an individual’s progress from week to week to determine if the symptoms are better or worse. This is more of a gauge of progress and not a prognosis tool[9].
Dietary Management[edit | edit source]
An elemental diet that includes food broken down into basic components like amino acids, vitamins, sugars, etc can help improve the symptoms associated with Crohn’s disease. There has also been improvements found in individuals who are placed on diets free of dairy, gluten and yeast products. Herbs have also been studied to determine effectiveness of relief of symptoms.
Additional ways to better manage the symptoms may include changes to your diet. Some key points include:
- Eating smaller meals and at more frequent intervals
- Reducing the amount of greasy, fatty foods that may produce diarrhoea and gas
- Limit consumption of milk and dairy products
- Reduce the amount of carbohydrates that are poorly digested that may cause diarrhoea, gas, bloating, cramps
- Restrict the intake of high-fiber foods such as nuts, seeds, corn, and popcorn[4].
Differential Diagnosis[edit | edit source]
The symptoms above are not specific to Crohn’s disease and have potential to be seen in other conditions. Differential diagnoses can include the following:
- Infectious causes – bacterial, viral, or parasitic infection.
- Ischemia – low blood flow to the small intestine or colon, usually seen in older patients
- Medication – non-steroidal anti-inflammatories, antibiotics, birth control pills
- Diverticulitis – infection of a diverticulum (outpouching of colon) that can present with left lower quadrant pain and fever
- Appendicitis – usually presents with right lower quadrant abdominal pain and fever
- Irritable bowel syndrome – can cause severe diarrhea and abdominal pain
- Lactose intolerance – can cause diarrhea, bloating, and abdominal pain. Patients with Crohn’s disease can also have lactose intolerance.
- Celiac disease – sensitivity to gluten (wheat) which can cause diarrhea and bloating.
- Gallstones
- Cancer, lymphoma
- Diseases that affect other organs in the abdomen also need to be considered such as:
- Endometriosis, pelvic inflammatory disease, ectopic pregnancy, ruptured ovarian cyst
- Kidney stones, bladder or kidney infections[6]
Case Reports[edit | edit source]
- Holaday M, Smith KE, Robertson S, Dallas J. An atypical eating disorder with Crohn's disease in a fifteen-year-old male: A case study. Adolescence [serial online]. 1994;29:865-73. Available from: Research Library Core. Accessed April 6, 2010, Document ID: 1499994.An atypical eating disorder with Crohn's disease in a fifteen-year-old male: A case study
- Ogram AE, Sobanko JF, Nigra TP. Metastatic cutaneous Crohn's disease of the face: a case report and review of the literature. Cutis. 2010;85:25-7. Available from: Pubmed. Acessed April 6, 2010. Metastatic cutaneous Crohn's disease of the face: a case report and review of the literature
Resources[edit | edit source]
CDAI Calculator: Crohn's Disease Activity Index Calculator
Presentations[edit | edit source]
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 Ranasinghe IR, Hsu R. Crohn disease. Available: https://www.ncbi.nlm.nih.gov/books/NBK436021/(accessed 1.10.2022)
- ↑ Crohns and Colitis Australia CD Available:https://crohnsandcolitis.org.au/about-crohns-colitis/crohns-disease/about-crohns-disease/ (accessed 1.10.2022)
- ↑ Thomas Craig. A Frank discussion on Crohn's Disease. Available at http://www.youtube.com/watch?v=Npda8xr2G-Y (last accessed 4/510)
- ↑ 4.0 4.1 4.2 4.3 Crohn’s and Colitis Foundation of America (CCFA). About Crohn’s Disease. http://ccfa.org/info/about/crohns (accessed 4 March 2010)
- ↑ National Digestive Diseases Information Clearinghouse (NDDIC). Crohn’s disease. http://digestive.niddk.nih.gov/ddiseases/pubs/crohns/ (accessed 4 March 2010).
- ↑ 6.0 6.1 6.2 6.3 6.4 Cheifetz Adam, Moss Alan, Peppercorn Mark. Crohn’s Disease. Knol Beta. Available at http://knol.google.com/k/crohn-s-disease#. Accessed 5 April 2010.
- ↑ Crohn’s Disease: Introduction. John Hopkins Medicine. Available at http://www.hopkins-gi.org/GDL_Disease.aspx?CurrentUDV=31&GDL_Disease_ID=291F2209-F8A9-4011-8094-11EC9BF3100E&GDL_DC_ID=D03119D7-57A3-4890-A717-CF1E7426C8BA (accessed 5 April 2010).
- ↑ Goodman CC, Fuller KS. Pathophysiology: Implications for the Physical Therapist. 3rd ed. St. Louis, MO: Saunders-Elsevier; 2009.
- ↑ Crohn’s Disease Activity Index (CDAI) calculator. CDAI Online Calculator. <ref="http://www.ibdjohn.com/cdai/"Crohn's Disease Activity Index, CDAI (accessed 4 March 2010)