Communication and Learning Disabilities: Difference between revisions
Rucha Gadgil (talk | contribs) No edit summary |
Rucha Gadgil (talk | contribs) No edit summary |
||
| (7 intermediate revisions by the same user not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> '''Original Editor '''- [[User:Rucha Gadgil|Rucha Gadgil]] | |||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> | |||
<div class="editorbox"> | |||
<br> | |||
</div> | |||
== What is Communication? == | == What is Communication? == | ||
50 to 90% of the people with learning difficulties have communication difficulties<ref name=":1">Chadwick DD, Jolliffe J. A pilot investigation into the efficacy of a signing training strategy for staff working with adults with intellectual disabilities. British Journal of Learning Disabilities. 2009;37(1):34–42.</ref><ref name=":2">Jackson C, Cavenagh P and Clibbens J. Communication and self-esteem in adults with down syndrome. International Journal of Language Communication Disorders. 2014;49(3):275–287.</ref><ref name=":3">Veselinova C. Supporting individuals with learning disabilities. Nursing and Residential Care. 2012;14(11):566–9.</ref>. According to Chadwick and Jolliffe<ref name=":1" />, communication is defined as “a mutual interactive process involving adaptation by both the communicative partners”. It is not just a pure transaction of information, but also relationships can be formed and build up in the process.<ref>Higgs J, Smith M, Webb G. Contexts of physiotherapy practice. Sydney: Churchill Livingstone Elsevier, 2008.</ref> | 50 to 90% of the people with learning difficulties have communication difficulties<ref name=":1">Chadwick DD, Jolliffe J. A pilot investigation into the efficacy of a signing training strategy for staff working with adults with intellectual disabilities. British Journal of Learning Disabilities. 2009;37(1):34–42.</ref><ref name=":2">Jackson C, Cavenagh P and Clibbens J. Communication and self-esteem in adults with down syndrome. International Journal of Language Communication Disorders. 2014;49(3):275–287.</ref><ref name=":3">Veselinova C. Supporting individuals with learning disabilities. Nursing and Residential Care. 2012;14(11):566–9.</ref>. According to Chadwick and Jolliffe<ref name=":1" />, communication is defined as “a mutual interactive process involving adaptation by both the communicative partners”. It is not just a pure transaction of information, but also relationships can be formed and build up in the process.<ref>Higgs J, Smith M, Webb G. Contexts of physiotherapy practice. Sydney: Churchill Livingstone Elsevier, 2008.</ref> | ||
| Line 4: | Line 10: | ||
Language is a complex form of communication that involves written or spoken words to convey ideas and symbolise objects. Reading, writing, drawing, speaking, listening, adjusting one’s tone of voice, making eye contact are all involved on communication. Communication involves ‘expression’ and ‘comprehension’ with each aspect being related to a specific neural network. | Language is a complex form of communication that involves written or spoken words to convey ideas and symbolise objects. Reading, writing, drawing, speaking, listening, adjusting one’s tone of voice, making eye contact are all involved on communication. Communication involves ‘expression’ and ‘comprehension’ with each aspect being related to a specific neural network. | ||
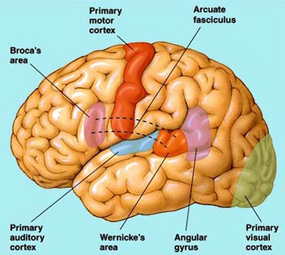
== Physiology of Brain and How it Affects Communication == | |||
[[ | [[Image:Brain-communication.png|thumb|right|291x259px|Figure 4.1 Image of the brain]] | ||
Figure 4.1 Image of the [[Brain Anatomy|brain]] | |||
Figure 4.1 Image of the brain | |||
The language centres are located in the left hemisphere in approximately 95% of human beings. Broca’s area and Wernicke’s area are located in the left hemisphere of the brain (see Figure 4.1).Broca’s area is known as the motor-speech area and it is located adjacent to the precentral gyrus of the motor cortex in the frontal lobes. This area controls the movements required for articulation, facial expression and phonation. | The language centres are located in the left hemisphere in approximately 95% of human beings. Broca’s area and Wernicke’s area are located in the left hemisphere of the brain (see Figure 4.1).Broca’s area is known as the motor-speech area and it is located adjacent to the precentral gyrus of the motor cortex in the frontal lobes. This area controls the movements required for articulation, facial expression and phonation. | ||
| Line 13: | Line 18: | ||
Wernicke’s area includes the auditory comprehension centre. It lies in the posterior superior temporal lobe near the auditory cortex. It plays a role in understanding both spoken and written messages as well as being able to formulate coherent speech. Commands generated in Wernicke’s area are transferred via a fibre tract called the arcuate fasciculus to Broca’s area. Wernicke’s area receives input from both the visual cortex and the auditory cortex. <ref name=":4">McBean D, Van Wijck F. Applied neurosciences for the allied health professions. Edinburgh: Churchill Livingstone Elsevier, 2014.</ref> | Wernicke’s area includes the auditory comprehension centre. It lies in the posterior superior temporal lobe near the auditory cortex. It plays a role in understanding both spoken and written messages as well as being able to formulate coherent speech. Commands generated in Wernicke’s area are transferred via a fibre tract called the arcuate fasciculus to Broca’s area. Wernicke’s area receives input from both the visual cortex and the auditory cortex. <ref name=":4">McBean D, Van Wijck F. Applied neurosciences for the allied health professions. Edinburgh: Churchill Livingstone Elsevier, 2014.</ref> | ||
== Types of Communication Difficulties == | |||
==== Aphasia ==== | ==== Aphasia ==== | ||
| Line 38: | Line 43: | ||
Some people may have difficulty finding their words which will affect the way they answer your questions.<ref name=":4" /> | Some people may have difficulty finding their words which will affect the way they answer your questions.<ref name=":4" /> | ||
== Impact of Communication Difficulties == | |||
Difficulty in communication can lower one’s self-esteem and result in low moods which will further impair communication<ref name=":2" />. This may result in “diagnostic overshadowing”, where people with learning disabilities are often misunderstood as having challenging behaviour when it is in fact their way of trying to communicate, and hence they are less likely to have chances to express their views.<ref name=":5">Kingston K, Bailey C. Assessing the pain of people with a learning disability. British Journal of Nursing. 2009;18(7):420–3.</ref><ref>Lewer A, Harding C. Communication is the key: Improving outcomes for people with learning disabilities. Tizard Learning Disability Review. 2013;18(3):132–40.</ref> | Difficulty in communication can lower one’s self-esteem and result in low moods which will further impair communication<ref name=":2" />. This may result in “diagnostic overshadowing”, where people with learning disabilities are often misunderstood as having challenging behaviour when it is in fact their way of trying to communicate, and hence they are less likely to have chances to express their views.<ref name=":5">Kingston K, Bailey C. Assessing the pain of people with a learning disability. British Journal of Nursing. 2009;18(7):420–3.</ref><ref>Lewer A, Harding C. Communication is the key: Improving outcomes for people with learning disabilities. Tizard Learning Disability Review. 2013;18(3):132–40.</ref> | ||
== Barriers to Communication == | |||
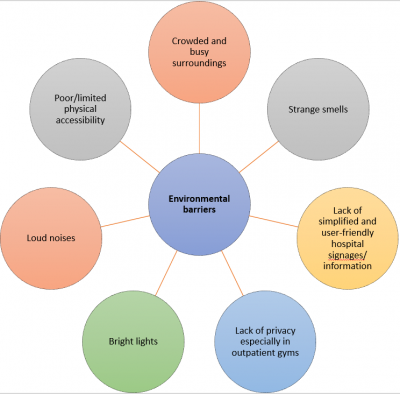
People with learning disability have limited vocabulary, problems expressing themselves and comprehending verbal and written information. They may also feel apprehensive and stressed meeting strangers in new environments. They are also 10 times more likely to have serious sight problems. Below are some barriers identified, in relation to the health professional, the person with a learning disability and the environment:<ref name=":6">Godsell M, Scarborough K. Improving communication for people with learning disabilities. Nursing Standard. 2006;20(30):58–65.</ref>[[ | People with learning disability have limited vocabulary, problems expressing themselves and comprehending verbal and written information. They may also feel apprehensive and stressed meeting strangers in new environments. They are also 10 times more likely to have serious sight problems. Below are some barriers identified, in relation to the health professional, the person with a learning disability and the environment:<ref name=":6">Godsell M, Scarborough K. Improving communication for people with learning disabilities. Nursing Standard. 2006;20(30):58–65.</ref> | ||
[[Image:Group 3 Barrier for PT.PNG|center|400x400px]] <br> [[Image:Group 3 Barrier for people with learning disability.PNG|center|400x400px]] | |||
<br> [[Image:Group 3 Environmental barrier.PNG|center|400x400px]] <br> | |||
== Strategies for Effective Communication == | |||
The video below explains ways of communicating with individuals have a learning disability<ref>Mencap. Communication: speaking to people with a learning disability. [Video] 2014 <nowiki>https://www.youtube.com/watch?v=IyV1v-nib38&t=1s</nowiki> (accessed 30 Dec 2016).</ref>: | The video below explains ways of communicating with individuals have a learning disability<ref>Mencap. Communication: speaking to people with a learning disability. [Video] 2014 <nowiki>https://www.youtube.com/watch?v=IyV1v-nib38&t=1s</nowiki> (accessed 30 Dec 2016).</ref>: | ||
| Line 53: | Line 61: | ||
* Observe for common subtle indicators of pain<ref name=":7">Beacroft M, Dodd K. ‘I feel pain’- audit of communication skills and understanding of pain and health needs with people with learning disabilities. British Journal of Learning Disabilities. 201;39(2):139–47.</ref>: Change in behaviour, Change in noise level, Change in body language or facial expressions, Patient is holding the part of the body that hurts. | * Observe for common subtle indicators of pain<ref name=":7">Beacroft M, Dodd K. ‘I feel pain’- audit of communication skills and understanding of pain and health needs with people with learning disabilities. British Journal of Learning Disabilities. 201;39(2):139–47.</ref>: Change in behaviour, Change in noise level, Change in body language or facial expressions, Patient is holding the part of the body that hurts. | ||
== Tools to Enhance Communication and Assessment == | |||
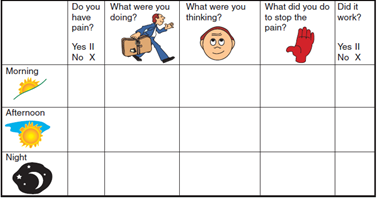
Pictures and symbols assist in the identification of location, type, severity and duration of pain<ref name=":7" />. For example, these tools by Kingston and Bailey <ref name=":5" /> allowed people with learning disabilities the opportunity and freedom to talk and describe their pain:[[ | Pictures and symbols assist in the identification of location, type, severity and duration of pain<ref name=":7" />. For example, these tools by Kingston and Bailey <ref name=":5" /> allowed people with learning disabilities the opportunity and freedom to talk and describe their pain: | ||
[[Image:Pain diary figure 1.png|thumb|left|417x259px|Figure 4.2 Pain diary]] | |||
Pain diary (Figure 4.2) <ref name=":5" />: A tick chart for the person with learning disability to complete. | |||
[[Image:Pain story.png|thumb|left|296x349px|Figure 4.3 Pain story]] | |||
[[Pain Assessment|Pain]] story (Figure 4.3) <ref name=":5" />: A template to help individuals talk about their pain. Includes aspects of the individual’s history, previous experiences of pain, and current influences upon their behaviour. | |||
Augmentative and Alternative Communication Strategies (AACs) can be used for individuals with more complex communication difficulties<ref name=":6" />. Examples by Veselinova<ref name=":3" /> include: | Augmentative and Alternative Communication Strategies (AACs) can be used for individuals with more complex communication difficulties<ref name=":6" />. Examples by Veselinova<ref name=":3" /> include: | ||
| Line 69: | Line 82: | ||
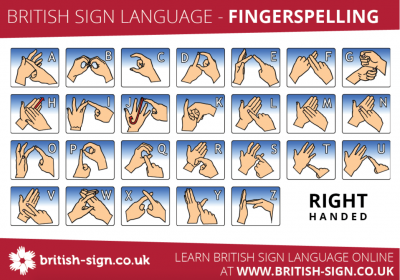
==== British Sign Language (BSL) ==== | ==== British Sign Language (BSL) ==== | ||
[[ | [[Image:Group 3 BSL.png|center|400x300px]] | ||
Sign Language is a means of communicating visually using gestures, facial expression and body language. It is mainly used by people who are deaf or have a hearing impairment. BSL has it’s own grammatical structure and syntax. It is not dependent or strongly related to spoken English. In 2011, it was reported that BSL was the preferred language 145,000 in the UK.<ref>British-sign.co.uk. What is british sign language. <nowiki>http://www.british-sign.co.uk/what-is-british-sign-language/</nowiki> (accessed 20 Jan 2017).</ref> | Sign Language is a means of communicating visually using gestures, facial expression and body language. It is mainly used by people who are deaf or have a hearing impairment. BSL has it’s own grammatical structure and syntax. It is not dependent or strongly related to spoken English. In 2011, it was reported that BSL was the preferred language 145,000 in the UK.<ref>British-sign.co.uk. What is british sign language. <nowiki>http://www.british-sign.co.uk/what-is-british-sign-language/</nowiki> (accessed 20 Jan 2017).</ref> | ||
| Line 76: | Line 89: | ||
A form of communication for tactile learners. Substitutes visual reading and writing. Usually for people with visual impairments or deafblindness.<ref>See/hear. Early literacy: braille and the young child. <nowiki>http://www.tsbvi.edu/seehear/summer98/literacy.htm</nowiki> (accessed 20 Jan 2017).</ref> | A form of communication for tactile learners. Substitutes visual reading and writing. Usually for people with visual impairments or deafblindness.<ref>See/hear. Early literacy: braille and the young child. <nowiki>http://www.tsbvi.edu/seehear/summer98/literacy.htm</nowiki> (accessed 20 Jan 2017).</ref> | ||
== Use of Assistive Technology == | |||
Symbols: Symbols can be used by people with communication difficulties to understand what people are saying and use them as a means of expressing themselves. Symbols are mostly available as collections or sets. Usually the word is printed above the symbol.<ref>Communication matters. Symbols. <nowiki>http://www.communicationmatters.org.uk/page/symbols</nowiki> (accessed 20 Jan 2017).</ref> | Symbols: Symbols can be used by people with communication difficulties to understand what people are saying and use them as a means of expressing themselves. Symbols are mostly available as collections or sets. Usually the word is printed above the symbol.<ref>Communication matters. Symbols. <nowiki>http://www.communicationmatters.org.uk/page/symbols</nowiki> (accessed 20 Jan 2017).</ref> | ||
[[ | [[Image:Group 3 Eye Gaze.png|thumb|left|Figure 4.4 Eye gaze]] | ||
Eye gaze: Eye gaze (Figure 4.4) is a method of communicating in which the person controls the mouse of a computer with their eyes. It works by the camera picking up light reflections from a person's pupils and then translating the eye movement into cursor movements.<ref>Inclusive technology. Eye gaze-say it with your eyes. <nowiki>http://www.inclusive.co.uk/articles/eye-gaze-say-it-with-your-eyes-a490</nowiki> (accessed 20 Jan 2017).</ref> | |||
[[ | [[Image:Group 3 VOCA.png|thumb|left|Figure 4.5 VOCA]] | ||
Voice Output Communication Aids (VOCAs) (Figure 4.5): This type of communication aid uses electronically stored speech as a means ofcommunication. Individual words and phrases can be used to form Sentences or longer messages. The vocabulary can contain several thousand words. Speech output may be digitised pre-recorded speech, synthesised (artificial) speech or both. Digitised messages are created by recording spoken words directly into the communication aid. Synthesised speech is computer-generated speech<ref>Living made easy for children. Voice output communication aids. <nowiki>http://www.livingmadeeasy.org.uk/communication/voice-output-communication-aids-1413/</nowiki> (accessed 20 Jan 2017).</ref>. | Voice Output Communication Aids (VOCAs) (Figure 4.5): This type of communication aid uses electronically stored speech as a means ofcommunication. Individual words and phrases can be used to form Sentences or longer messages. The vocabulary can contain several thousand words. Speech output may be digitised pre-recorded speech, synthesised (artificial) speech or both. Digitised messages are created by recording spoken words directly into the communication aid. Synthesised speech is computer-generated speech<ref>Living made easy for children. Voice output communication aids. <nowiki>http://www.livingmadeeasy.org.uk/communication/voice-output-communication-aids-1413/</nowiki> (accessed 20 Jan 2017).</ref>. | ||
| Line 107: | Line 121: | ||
* Have difficulty describing feelings or events, may be explained in sentences that do not make sense. | * Have difficulty describing feelings or events, may be explained in sentences that do not make sense. | ||
* Express very strong emotions that may seem inappropriate to the situation such as anger or frustration. | * Express very strong emotions that may seem inappropriate to the situation such as anger or frustration. | ||
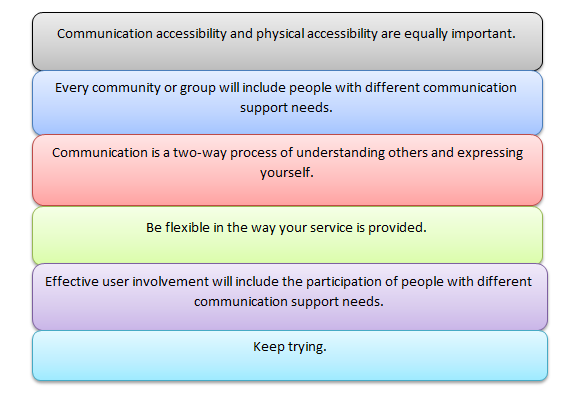
The six principles of inclusive communication are: | The six principles of inclusive communication are: | ||
[[Image:6 principles.png]] | |||
== Acquiring Informed Consent == | == Acquiring Informed Consent == | ||
It is imperative to always acquire informed consent from the patients before commencing assessments or treatments. Informed consent is defined by the Law Society as: ‘an individual is always presumed to be competent, or to have mental capacity to enter into a particular transaction, until the contrary is proved’.<ref name=":8" /> Therefore, you should bear in mind that no one, even the parents, can consent to or refuse treatment on behalf of another adult who lacks capacity to consent. Some people will never be able to make decisions, but judgement must not be made until all practicable steps have been taken to help the patient. You must only regard a patient as lacking capacity once it is clear that after all appropriate help and support, they cannot understand, retain, use or weigh up the information needed to make that decision, or communicate their wishes. Therefore, consent can be waived, but only under certain conditions: | It is imperative to always acquire informed consent from the patients before commencing assessments or treatments. Informed consent is defined by the Law Society as: ‘an individual is always presumed to be competent, or to have mental capacity to enter into a particular transaction, until the contrary is proved’.<ref name=":8" /> Therefore, you should bear in mind that no one, even the parents, can consent to or refuse treatment on behalf of another adult who lacks capacity to consent. Some people will never be able to make decisions, but judgement must not be made until all practicable steps have been taken to help the patient. You must only regard a patient as lacking capacity once it is clear that after all appropriate help and support, they cannot understand, retain, use or weigh up the information needed to make that decision, or communicate their wishes. Therefore, consent can be waived, but only under certain conditions: | ||
| Line 154: | Line 167: | ||
== References == | == References == | ||
<references /> | |||
[[Category:Communication]] | |||
[[Category:Paediatrics]] | |||
[[Category:Assistive Technology]] | |||
Latest revision as of 22:25, 9 May 2024
What is Communication?[edit | edit source]
50 to 90% of the people with learning difficulties have communication difficulties[1][2][3]. According to Chadwick and Jolliffe[1], communication is defined as “a mutual interactive process involving adaptation by both the communicative partners”. It is not just a pure transaction of information, but also relationships can be formed and build up in the process.[4]
Language is a complex form of communication that involves written or spoken words to convey ideas and symbolise objects. Reading, writing, drawing, speaking, listening, adjusting one’s tone of voice, making eye contact are all involved on communication. Communication involves ‘expression’ and ‘comprehension’ with each aspect being related to a specific neural network.
Physiology of Brain and How it Affects Communication[edit | edit source]
Figure 4.1 Image of the brain
The language centres are located in the left hemisphere in approximately 95% of human beings. Broca’s area and Wernicke’s area are located in the left hemisphere of the brain (see Figure 4.1).Broca’s area is known as the motor-speech area and it is located adjacent to the precentral gyrus of the motor cortex in the frontal lobes. This area controls the movements required for articulation, facial expression and phonation.
Wernicke’s area includes the auditory comprehension centre. It lies in the posterior superior temporal lobe near the auditory cortex. It plays a role in understanding both spoken and written messages as well as being able to formulate coherent speech. Commands generated in Wernicke’s area are transferred via a fibre tract called the arcuate fasciculus to Broca’s area. Wernicke’s area receives input from both the visual cortex and the auditory cortex. [5]
Types of Communication Difficulties[edit | edit source]
Aphasia[edit | edit source]
Damage to the language centres of the brain can result in aphasia. Aphasia can affect expression and comprehension of speech, reading and writing, gesture and the use of language. There are 3 types of aphasia - expressive, receptive and global.
Expressive aphasia is when a person has difficulty translating their ideas into meaningful sounds which results in non-fluent speech. It is associated with damage in Broca’s area.
Receptive aphasia is associated with damage in Wernicke’s area. People with receptive aphasia have difficulty in the comprehension of language.
Global aphasia occurs where there is widespread brain damage including lesions in the left hemisphere. This results in impairment of both expressive and receptive language functions.
There are also a range of other neurological signs such as hemianopia, hemiplegia, visual impairments, auditory impairments, attention and memory impairments and other cognitive impairments.
Dysarthria[edit | edit source]
Dysarthria refers to difficulty with executing speech. There are five sub-systems that are required in the coordination of speech. These include respiration, phonation, articulation, resonance and prosody. Weakness in any of these systems or incoordination of these systems can cause dysarthria.
Apraxia of Speech[edit | edit source]
Apraxia of Speech is an inability to programme speech movements. It is an impairment in the ability to coordinate the timing, force production and sequencing of movements for the production of speech.
Comprehension Impairments[edit | edit source]
A person may not understand some or all of the instructions that are given to them. A person’s non-verbal communication may suggest that they understand what you are saying but in fact they may not understand what you are saying. A person may mirror you, such that if you smile and nod they may do the same and they may also mirror your body language too.
Expressive Impairments[edit | edit source]
Some people may have difficulty finding their words which will affect the way they answer your questions.[5]
Impact of Communication Difficulties[edit | edit source]
Difficulty in communication can lower one’s self-esteem and result in low moods which will further impair communication[2]. This may result in “diagnostic overshadowing”, where people with learning disabilities are often misunderstood as having challenging behaviour when it is in fact their way of trying to communicate, and hence they are less likely to have chances to express their views.[6][7]
Barriers to Communication[edit | edit source]
People with learning disability have limited vocabulary, problems expressing themselves and comprehending verbal and written information. They may also feel apprehensive and stressed meeting strangers in new environments. They are also 10 times more likely to have serious sight problems. Below are some barriers identified, in relation to the health professional, the person with a learning disability and the environment:[8]
Strategies for Effective Communication[edit | edit source]
The video below explains ways of communicating with individuals have a learning disability[9]:
<iframe title='Play video' src='//www.youtube.com/embed/IyV1v-nib38?' width='640' height='360' frameborder='0' allowfullscreen='true'></iframe>
- Use easy and simplified language, but do not appear supercilious[3].
- Speak at a slow comfortable pace[3].
- Observe for common subtle indicators of pain[10]: Change in behaviour, Change in noise level, Change in body language or facial expressions, Patient is holding the part of the body that hurts.
Tools to Enhance Communication and Assessment[edit | edit source]
Pictures and symbols assist in the identification of location, type, severity and duration of pain[10]. For example, these tools by Kingston and Bailey [6] allowed people with learning disabilities the opportunity and freedom to talk and describe their pain:
Pain diary (Figure 4.2) [6]: A tick chart for the person with learning disability to complete.
Pain story (Figure 4.3) [6]: A template to help individuals talk about their pain. Includes aspects of the individual’s history, previous experiences of pain, and current influences upon their behaviour.
Augmentative and Alternative Communication Strategies (AACs) can be used for individuals with more complex communication difficulties[8]. Examples by Veselinova[3] include:
Makaton[edit | edit source]
Makaton is a language programme designed to provide a means of communication to people who have difficulty communicating by speaking. Research has shown that this language programme has been effectively used with individuals who have autism, Down’s syndrome, multisensory impairment and neurological disorders. Makaton uses signs from British Sign Language. It uses a multimodal approach to teach language and literacy skills. The programme uses a combination of speech, signs and symbols to meet the needs of the student.[11]
British Sign Language (BSL)[edit | edit source]
Sign Language is a means of communicating visually using gestures, facial expression and body language. It is mainly used by people who are deaf or have a hearing impairment. BSL has it’s own grammatical structure and syntax. It is not dependent or strongly related to spoken English. In 2011, it was reported that BSL was the preferred language 145,000 in the UK.[12]
Braille[edit | edit source]
A form of communication for tactile learners. Substitutes visual reading and writing. Usually for people with visual impairments or deafblindness.[13]
Use of Assistive Technology[edit | edit source]
Symbols: Symbols can be used by people with communication difficulties to understand what people are saying and use them as a means of expressing themselves. Symbols are mostly available as collections or sets. Usually the word is printed above the symbol.[14]
Eye gaze: Eye gaze (Figure 4.4) is a method of communicating in which the person controls the mouse of a computer with their eyes. It works by the camera picking up light reflections from a person's pupils and then translating the eye movement into cursor movements.[15]
Voice Output Communication Aids (VOCAs) (Figure 4.5): This type of communication aid uses electronically stored speech as a means ofcommunication. Individual words and phrases can be used to form Sentences or longer messages. The vocabulary can contain several thousand words. Speech output may be digitised pre-recorded speech, synthesised (artificial) speech or both. Digitised messages are created by recording spoken words directly into the communication aid. Synthesised speech is computer-generated speech[16].
Inclusive Communication[edit | edit source]
Inclusive communication[17] is a means of sharing information so that everybody can understand it. For service providers, it means that you understand that people understand and express themselves in different ways. Inclusive communication refers to:
- Written information
- Face to face
- Telephone
- Online information
Inclusive communication aims to ensure that people with communication support needs are able to live independently, access services easily and are able to participate in the wider community.
A person with communication support needs may need support with understanding, expressing themselves and interacting with others. As physiotherapists we need to use other methods of communication so that our patients understand what we are saying to them and are able to express themselves. A person with communication support needs may:
- Avoid services completely.
- Not turn up for an appointment.
- Respond only to some advice given or nodding their head as though they understand.
- Ask lots of repeated questions.
- Give irrelevant, rambling or unclear sentences.
- Have challenging behaviours.
- Appear bored or unable to maintain attention.
- Have difficulty describing feelings or events, may be explained in sentences that do not make sense.
- Express very strong emotions that may seem inappropriate to the situation such as anger or frustration.
The six principles of inclusive communication are:
Acquiring Informed Consent[edit | edit source]
It is imperative to always acquire informed consent from the patients before commencing assessments or treatments. Informed consent is defined by the Law Society as: ‘an individual is always presumed to be competent, or to have mental capacity to enter into a particular transaction, until the contrary is proved’.[18] Therefore, you should bear in mind that no one, even the parents, can consent to or refuse treatment on behalf of another adult who lacks capacity to consent. Some people will never be able to make decisions, but judgement must not be made until all practicable steps have been taken to help the patient. You must only regard a patient as lacking capacity once it is clear that after all appropriate help and support, they cannot understand, retain, use or weigh up the information needed to make that decision, or communicate their wishes. Therefore, consent can be waived, but only under certain conditions:
- To preserve life, health or well being of the person e.g. in emergency situations
- If the patient is being held under the Mental Health Act
- It is agreed during a formal ‘Best Interests’ meeting (a multidisciplinary meeting including all professionals/ carers/family/patient involved in the care of the patient) that a particular intervention was in accordance with best practice, which includes best medical interests and the patient’s general being, wishes, and needs.
Who can give informed consent?[edit | edit source]
Individuals who received an understandable explanation of the following:
- What will happen and why it is necessary in very simple terms?
- The benefits and risks of the treatment and what alternatives are available
- What will happen if the patient does not consent, and
- Being able to retain what you have discussed with them and able to make a decision
Someone with severe learning disability is thought to be unable to make a decision if they can't:
- Understand information about the decision.
- Remember that information
- Use that information to make a decision.
- Communicate their decision by talking, using sign language or by any other means.[19]
Where the patient has never been competent, relatives, carers and friends may be best placed to advise on the patient's needs and preferences. It is good practice to consult with people close to the patient to gain agreement unless the person had good reasons that they would not wish those people to be consulted, or the situation is urgent. If an incompetent patient has clearly indicated in the past, while competent, that they would refuse treatment in certain circumstances (an 'advance refusal'), and those circumstances arise, you must abide by that refusal.
Never ever coerce a patient into making decisions, just because you believe that the patient should have the treatment. If controversial circumstances are involved, decisions around best interests should be made via the court.
To find out whether the individual has the capacity to give informed consent, it is essential to[20]:
- Elicit what skills or knowledge the patient may require to exercise capacity.
- Find out what support and information the patient requires to achieve capacity,
- Involve someone who knows the patient well and their level of communication.
What does capacity to give informed consent mean?[edit | edit source]
Capacity refers to the ability to use and understand information to make a particular decision at a particular time, and can vary in the same person for different decisions. Understanding depends on cognitive abilities, effective communication and accessible information. A person with capacity has the right to refuse treatment, whereas in the case of an adult who lacks capacity, the health professional has a duty to provide treatment and care in the best interests of that adult, even if the person does not agree.[18][21]
Here's an adapted case study to aid your understanding of what it meant by capacity.[20]
50-year-old Mr A has severe cerebral palsy with mild learning disabilities and some swallowing difficulties. He developed epilepsy and was offered tablets by the doctor. After the doctor’s explanation, he said that the epilepsy was not causing him any problems and that he hated to take tablets. He understood that tablets would prevent a seizure, but he did not think the treatment was worth his while. The doctor respected his decision.
1 year later, Mr A’s dysphagia got worse (NB this was not caused by non-treatment of the epilepsy). He had repeated chest infections. If he continued oral intake of food, he was likely to develop aspiration pneumonia, or die o undernutrition. He was offered a feeding gastronomy, but he refused. Did Mr A really understand what a gastronomy involved? Did he realise that he might die without one?
References[edit | edit source]
- ↑ 1.0 1.1 Chadwick DD, Jolliffe J. A pilot investigation into the efficacy of a signing training strategy for staff working with adults with intellectual disabilities. British Journal of Learning Disabilities. 2009;37(1):34–42.
- ↑ 2.0 2.1 Jackson C, Cavenagh P and Clibbens J. Communication and self-esteem in adults with down syndrome. International Journal of Language Communication Disorders. 2014;49(3):275–287.
- ↑ 3.0 3.1 3.2 3.3 Veselinova C. Supporting individuals with learning disabilities. Nursing and Residential Care. 2012;14(11):566–9.
- ↑ Higgs J, Smith M, Webb G. Contexts of physiotherapy practice. Sydney: Churchill Livingstone Elsevier, 2008.
- ↑ 5.0 5.1 McBean D, Van Wijck F. Applied neurosciences for the allied health professions. Edinburgh: Churchill Livingstone Elsevier, 2014.
- ↑ 6.0 6.1 6.2 6.3 Kingston K, Bailey C. Assessing the pain of people with a learning disability. British Journal of Nursing. 2009;18(7):420–3.
- ↑ Lewer A, Harding C. Communication is the key: Improving outcomes for people with learning disabilities. Tizard Learning Disability Review. 2013;18(3):132–40.
- ↑ 8.0 8.1 Godsell M, Scarborough K. Improving communication for people with learning disabilities. Nursing Standard. 2006;20(30):58–65.
- ↑ Mencap. Communication: speaking to people with a learning disability. [Video] 2014 https://www.youtube.com/watch?v=IyV1v-nib38&t=1s (accessed 30 Dec 2016).
- ↑ 10.0 10.1 Beacroft M, Dodd K. ‘I feel pain’- audit of communication skills and understanding of pain and health needs with people with learning disabilities. British Journal of Learning Disabilities. 201;39(2):139–47.
- ↑ CMS S. About Makaton. https://www.makaton.org/aboutMakaton/ (accessed 17 Jan 2017).
- ↑ British-sign.co.uk. What is british sign language. http://www.british-sign.co.uk/what-is-british-sign-language/ (accessed 20 Jan 2017).
- ↑ See/hear. Early literacy: braille and the young child. http://www.tsbvi.edu/seehear/summer98/literacy.htm (accessed 20 Jan 2017).
- ↑ Communication matters. Symbols. http://www.communicationmatters.org.uk/page/symbols (accessed 20 Jan 2017).
- ↑ Inclusive technology. Eye gaze-say it with your eyes. http://www.inclusive.co.uk/articles/eye-gaze-say-it-with-your-eyes-a490 (accessed 20 Jan 2017).
- ↑ Living made easy for children. Voice output communication aids. http://www.livingmadeeasy.org.uk/communication/voice-output-communication-aids-1413/ (accessed 20 Jan 2017).
- ↑ The Scottish Government. Principles of inclusive communication: An information and self-assessment tool for public authorities. Edinburgh, 2011.
- ↑ 18.0 18.1 Daniels S. Dartford and Gravesham NHS Trust. Consent. http://www.dvh.nhs.uk/for-patients-and-visitors/learning-disabilities/consent/ (accessed 12 Jan 2017).
- ↑ NHS Choices. Consent to treatment - capacity. http://www.nhs.uk/Conditions/Consent-to-treatment/Pages/Capacity.aspx (accessed 17 Jan 2017).
- ↑ 20.0 20.1 Consent and people with intellectual disabilities: The basics. http://www.intellectualdisability.info/how-to-guides/articles/consent-and-people-with-intellectual-disabilities-the-basics (accessed 13 Jan 2017).
- ↑ General Medical Council. Consent and capacity. http://www.gmc-uk.org/learningdisabilities/237.aspx (accessed 13 Jan 2017).