Chronic Low Back Pain: Difference between revisions
Nele Kiekens (talk | contribs) No edit summary |
Nele Kiekens (talk | contribs) No edit summary |
||
| Line 130: | Line 130: | ||
https://www.youtube.com/watch?v=DBh4_7YtLaA<br> | https://www.youtube.com/watch?v=DBh4_7YtLaA<br> | ||
<br> | |||
== Clinical Bottom Line == | == Clinical Bottom Line == | ||
Revision as of 21:37, 1 February 2017
Original Editors - Bryan Jacobson, Tori Westcott, Ashley Bohanan, Alisha Lopez
Lead Authors -
Search Strategy[edit | edit source]
Pubmed, Web of Science, Pedro
Description/Description[edit | edit source]
Low back pain (LBP) is the fifth most common reason for physician visits, which affects nearly 60-80% of people throughout their lifetime. Low back pain that has been present for longer than three months is considered chronic, although there is still no consensus about the definition of CLBP. Specific causes of LBP are uncommon, and in approximately 90% of patients a specific generator cannot be identified with certainty. (1) More than 80% of all health care costs can be attributed to chronic LBP. Nearly a third of people seeking treatment for low back pain will have persistent moderate pain for one year after an acute episode. It is estimated that seven million adults in the United States have activity limitations as a result of chronic low back pain (31).
Chronic low back pain (CLBP) has been associated with neurochemical, structural, and functional cortical changes (28) of several brain regions including the somatosensory cortex. (3) Complex processes of peripheral and central sensitization may influence the evolution of acute to chronic pain. (4)
Clinically Relevant Anatomy[edit | edit source]
The lumbar region is situated under the thoracic region of the spine. The lower back consists of five vertebrae (L1- L5). It has a slight inward curve known as lordosis. The fifth lumbar vertebrae is connected with the top of the sacrum. The vertebrae of the lumbar spine are connected in the back by facet joints, which allow for forward and backward extension, as well as twisting movements.The two lowest segments in the lumbar spine, L5-S1 and L4-L5, carry the most weight and have the most movement, this makes the area prone to injury. In between vertebrae are spinal discs, they provide support. Discs in the lumbar region of the spine are most likely to herniate or degenerate, which can cause pain in the lower back, or radiating pain to the legs and feet. The spinal cord travels from the base of the skull to the joint at T12-L1, where the thoracic spine meets the lumbar spine. At this segment, nerve roots branch out from the spinal cord, forming the cauda equina. Some lower back conditions may compress these nerve roots, resulting in pain that radiates to the lower extremities, known as radiculopathy. The lower back region also contains large muscles that support the back and allow for movement in the trunk of the body. These muscles can spasm or become strained, which is a common cause of lower back pain. (Prometheus)
Epidemiology /Etiology[edit | edit source]
5-10% of all low back pain patients will develop CLBP. CLBP prevalence rates are lower in individuals aged 20-30 years, increasing from the third decade of life, and reaching the highest prevalence between 50-60 years. However the prevalence rates stabilize in the seventh decade of life. There’s no difference in CLBP prevalence at different periods of the year or in different places.(38)
There is higher CLBP prevalence in females, people of lower economic status, people with less schooling and smokers. There’s indication that prevalence has doubled over time. This may be due to important changes in lifestyle (obesity) and in the work industry. Factors as a family history of disabling back pain, radiating pain, advice to rest upon back pain consultation, occupational LBP or LBP caused by traffic injury are all associated with chronic disabling back pain over lifetime.(39) Job satisfaction and psychosocial factors also play a role in the development of CLBP.(40)
Musculoskeletal disorders are a comorbid condition strongly linked to CLBP. A moderate association was found when considering the whole musculoskeletal chapter, a stronger association was found when considering the somatoform symptoms related to the musculoskeletal cluster. (41)
In patients with low back pain (LBP), alterations in fiber typing in Multifidus and erector spinae are assumed to be possible factors in the etiology and/or recurrence of pain symptoms as it negatively affects muscle strength and endurance. In case of the latter, type I fibers have been argued to be more affected by pain and immobilization than type II fibers. (4)
Characteristics/Clinical Presentation[edit | edit source]
Most patients that suffer from CLBP experience pain in the lower area of the back (lumbar and sacroiliac regions) and mobility impairment. Pain can also radiate in the lower extremities, or generalized pain can be present. Patients with CLBP can also experience movement and coordination impairments. This could affect the control of voluntary movements of the patient.
It can be challenging for the patient to maintain the neutral position, malalignment of the body can occur. It can also be found difficult to maintain a standing, sitting or a lying position, especially in case of radiating pain to the lower extremities. Carrying things in the arms, or bending can also provoke complaints. Daily activities, such as cleaning, sports and other recreational occupations can become a big task for people with CLBP.
On the occasion of generalized pain, sensory experiences of the patient can also become altered; fear-avoidance beliefs, pain catastrophizing and depressive thoughts can appear. (17) If symptoms like these occur, central sensitisation can be present. It is important to monitor these yellow flags, as well as it is important to monitor blue flags and black flags.
The complaints are recurring and occur longer than three months. It is possible that CLBP passes in episodes. Some episodes are more severe than others, but overall the patient is affected by the impairments. Eventually, social contact and work environment will suffer from this great impact on the patient's health and wellbeing.
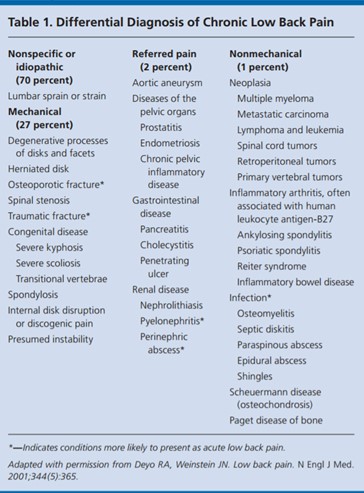
Differential Diagnosis[edit | edit source]
Lower back pain is a frequent condition for patients seeking care from physical therapists in outpatient settings. The challenge for clinicians is to recognize patients in whom lower back pain may be related to underlying pathological conditions.
Table 1 gives a list of differential diagnosis. (13)
For back pain associated with specific spinal cause, such as radiculopathy or spinal stenosis, magnetic resonance imaging (MRI) or CT (computed tomography) may establish diagnosis. (13)
In some differential diagnosis, immediate intervention is required.
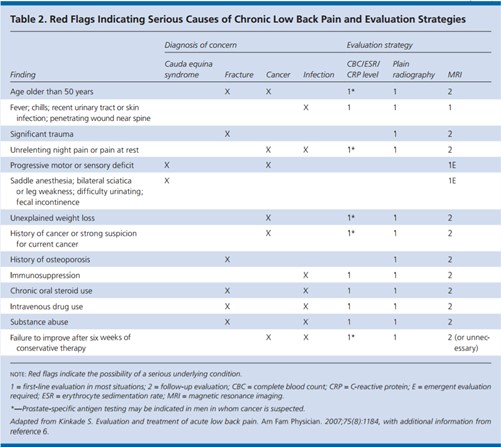
Table 2 shows a list of “red flags”: Red flags in spinal conditions, specific for lower back pain. These are signs or indicators of possible (severe) underlying pathology. (13) When these signs are found present, further screening is required and patients should be checked out as soon as possible.
Diagnostic Procedures[edit | edit source]
Chronic lower back pain is difficult to diagnose on one hand, but on the other hand the definition is very simple. In fact, if the back pain continues to be present for 3 months or more, we can consider it “chronic lower back pain”. Generally, patients are diagnosed based on their history. The specific diagnosis is then formulated based on the examination and clinical outcomes. Questionnaires can be used, as well as a body pain diagram, on which the patient locates his pain and pain distribution. (7)
In case of specific lower back pain, other diagnostic procedures are required to confirm diagnosis. Magnetic Resonance Imaging (MRI) and Computed Tomography (CT-scan) may put these diseases forward (radiculopathy, discopathy …). Nevertheless, patients are frequently misdiagnosed. Normal age-related degenerative changes in the spine can be misinterpreted as an initiator of pain, although we can see the same changes in people with no complaints. For this reason, radiological pictures differ according to age, even in patients with no chronic low back pain (2,3,8)
It is also important to check for any presence of red flags.
Outcome Measures[edit | edit source]
Validated self-report questionnaires, such as the Oswestry Disability Index and the Roland‐Morris_Disability_Questionnaire should be used at baseline and throughout the course of treatment to monitor a change in a patient’s status. (17) The Modified Somatic Perceptions Questionnaire (MSPQ) is used to assess pain intensity, disability and somatic pain perception respectively.The MSPQ is relevant and appropriate for use in a CLBP study as it was devised and evaluated specifically for CLBP and an MSPQ score > 13 is one of the clinical predictors of lumbar facet syndrome. (45)
Examination[edit | edit source]
Research has shown that the patient history and biopsychosocial evaluation are crucial to establish chronic LBP. Patient history and self-report forms help rule out serious pathologies such as cauda equina, Ankylosing_Spondylitis, nerve compromise and cancer. The Fear‐Avoidance_Belief_Questionnaire (FABQ) self-report form has been shown to predict chronicity and psychosocial factors influencing patient prognosis (32) The focus of the physical examination is to confirm the hypothesis of chronic LBP by eliminating other pathologies or mechanisms (30)
There are also clinical tests that could be used to sort patients with a higher risk for CLBP from patients with (sub)acute low back pain. The best predictor is the lumbar spine flexion test. Other differences might be seen in functional tests, sensation in the feet, and in the different pain provocation tests. (18)
Prevention
[edit | edit source]
Identifying risk factors allows development of healthcare strategies (and prevention) to reduce the burden of chronic pain. Some risk factors cannot be changed, but others can be modified. Risk factors include socio-demographic, clinical, psychological and biological factors. For example anxiety, depression and catastrophizing beliefs (yellow flags) are associated with chronic pain and with a poor prognosis. (15)
Operant treatment approaches can be integrated into standard pain management for acute/subacute low back pain. Graded activity and behavioural education are promising treatment approaches for the prevention of CLBP and explaining the physiology of pain can also work preventive. (16,17)
Medical managment[edit | edit source]
Pharmacology: For chronic low back pain, pharmacological management can be used on a continuous basis or as needed. (31) (level of evidence 2c) However it’s important to advise patients to use it as a tool to stay active and to engage in treatment, rather than as a solution itself.
- Acetaminophen: The American Pain Society/American College of Physicians guidelines recommend that acetaminophen be used as a first-line option with any duration of low back pain. Acetaminophen is an antipyretic and analgesic medication without anti-inflammatory properties. Risk of hepatotoxicity is the main complication, therefore dosing instruction must be followed carefully.(31) (level of evidence 2c)
Recent research states that there are a lot of uncertainties about the effect of paracetamol so there is a need for further research. There is only low-quality evidence for no effect on immediate pain reduction.(44) (level of evidence 1a)
- NSAIDS: Non-steroidal Anti-Inflammatory drugs are another medication recommended as a first-line medication for short-term use. They are pain relieving and anti-inflammatory medications that block the cyclo-oxygenase (COX)-2 enzyme. Side-effects include gastrointestinal and renal complications, such as bleeding ulcers and perforation. NSAIDS are slightly effective for the improvement of disability. (31, 42) (level of evidence 2c) (level of evidence 1a)
- Opioids: Opioids are considered an option in patients with moderate or severe pain.
Research has found opioids moderately effective for pain relief, although effects on functional outcomes were small. Slow-release opioids are recommended when compared to immediate-release opioids to prevent adverse effects, and should be given regularly rather than as needed. Due to the addictive nature of opioids, long-term use should be carefully monitored for misuse (31,35) (level of evidence 2c)(level of evidence 1a)
- Antidepressants: Tricyclic antidepressants (TCA) are commonly used to treat numerous chronic pain syndromes. However, there is conflicting evidence on whether there are significant changes in pain relief or disability with CLBP. A recent systematic review found that there is evidence of moderate quality indicating that there is no difference in pain relief between antidepressants and placebo for patients with chronic LBP. (36) (level of evidence 1a) Depression is common in patients with chronic low back pain and should be treated appropriately (30)
- Other medications: Skeletal muscle relaxants, benzodiazepines, and antiepileptic medications are not recommended because of the insufficient evidence towards their effectiveness for chronic low back pain. (31) (level of evidence 2c)
Multidisciplinary approach
When treating patients with chronic LBP it has been shown that having been treated by a multidisciplinary team yields improvements. The multidisciplinary approach includes treating the physical, psychological, emotional, and socio professional aspects of the disorder (33) (level of evidence 2b) "Fear of pain in turn is supposed to initiate worrying about the consequences of pain and hence increases avoidance behavior, leading in the long term to increased pain, functional disability, and depression." (34) (level of evidence 4)
In patients who have already failed a course of conservative treatment, multidisciplinary rehabilitation programmes result in better outcomes with respect to long term pain and disability compared with usual care or physical treatments. Patients in these programmes also have increased odds of being at work compared with patients receiving physical treatment. (14) (level of evidence 1a)
For more information: Behavioral_pain_management_of_chronic_low_back_pain
Physical Therapy Management
[edit | edit source]
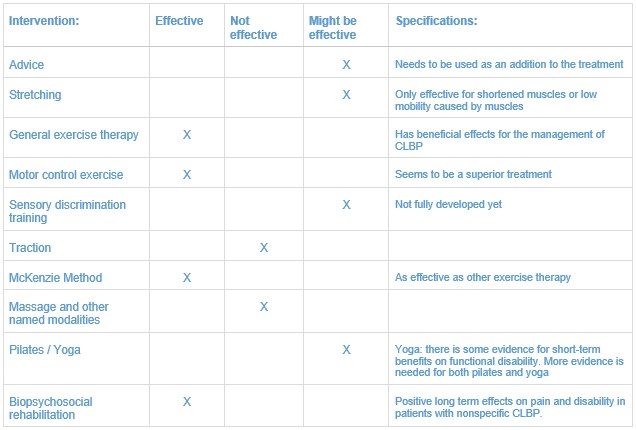
Interventions:
- Advice: For nonspecific low back pain the general advice on self-management is to remain active. This is also the case in CLBP. (30, 17) (resource - guideline based on level 1a and level 1b evidence)
It is frequently assumed that a firm mattress has beneficial effects on low back pain. In fact, for patients with chronic nonspecific low back pain (with no referred pain), a medium-firm mattress is found to be superior. Patients experience less pain and disability during the day and overnight. (43) (level of evidence 1b)
Giving advice only will probably not suffice. It is important to combine multiple treatment means to avoid recurrency. (17)
- Stretching and flexibility exercises: are used to improve hamstring, quadriceps, piriformis, and hip joint capsule range of motion. (10) (level of evidence 2b) The aim is to reduce pain, improve movement, and improve functional limitations of movement.
Exercise therapy:
Exercise therapy has been shown to have beneficial effects for the management of chronic low back pain. (11) (level of evidence 1b)
Utilisation of trunk coordination, strengthening, and endurance exercises reduces low back pain and disability in patients with subacute and chronic low back pain with movement coordination impairments. (17) (resource - guideline based on level 1a and level 1b evidence)
Moderate- to high-intensity exercise will be considered for patients with CLBP without generalized pain. For patients with CLBP with generalized pain incorporating progressive, low-intensity, submaximal fitness and endurance activities into the pain management and health promotion strategies will be considered. (17)
-Core strengthening exercises: are used to restore the coordination and control of the trunk muscles to improve control of the lumbar spine and pelvis. These exercises aim to restore the strength and endurance of the trunk muscles to meet the demands of control. Core exercise may be more effective than general exercise in relieving pain and improving back-specific function for patients with CLBP in the short term. No significant differences were found in the long term. (19) (level of evidence 1a)
- Motor control exercise: motor control exercise protocols have been shown to be an effective treatment of chronic low back pain. Common targeted muscles include transversus abdominis, multifidus, the diaphragm and pelvic floor muscles.The focus of motor control exercises is to improve neuromuscular control of trunk segments involved in movement of the spine.(26, 27, 29, 37) (level of evidence 1a) (27 = resource) (level of evidence 1b) (level of evidence 1b)
Instructions: An independent contraction of the deep stabilizing muscles, such as the transversus abdominis and multifidus, facilitated by pelvic floor contraction, which leads to their co-contraction, whilst instructing to control breathing by maintaining resting tidal volumes throughout deep trunk activation maneuvers. Progression is achieved when mastery of contraction in static tasks is achieved. Then move on to implementation of deep muscle contraction during dynamic tasks. Daily practice at home for 30 minutes is instructed. (11) (level of evidence 1b)
Motor control exercises seem to be superior to several other treatments, such as general exercise (with regard to disability in the short-, intermediate, and long-term and pain in the short- and intermediate term), spinal manual therapy (with regard to disability during all time periods) and minimal intervention (during all time periods with regard to pain and disability). (20) (level of evidence 1a)
- Sensory discrimination training: cortical reorganization presents a barrier to successful recovery; however the plasticity that underpins cortical reorganization also suggests that it might be responsive to targeted treatments, such as sensory discrimination training (SDT). SDT comprises tactile discrimination and sensorimotor retraining approaches, which involve the recognition of the location and the type of the stimuli by the patient (localization training). However, these approaches are not fully developed from a pathoanatomical perspective, since the processes involved in cortical reorganization in CLBP are not fully understood . (3) (level of evidence 1a)
- Traction: Summary evidence concludes that mechanical lumbar traction is not effective for treating acute or chronic nonspecific low back pain (LBP) Few trials evaluated the effectiveness of treatments for radicular low back pain, but the available evidence showed traction and spinal manipulation were not effective or were associated with small effects. (22) (level of evidence 2b)
- Mckenzie Method: Has been shown to be as effective as other exercise therapy. Compared to motor control exercises there is no significant difference in pain and function scores. However patients reported greater improvement in sense of recovery in the short term compared to patients who received motor control exercises. This obviously might differ across different groups of patients. (11) (level of evidence 1b)
- Massage and modalities such as electrical nerve stimulation, low-level laser therapy, shortwave diathermy and ultrasonography have not been shown to be effective interventions. (30) Exercise focusing on general improvement of strength and cardiovascular endurance is not suggested for optimal outcomes in patients with chronic low back pain. (29) (level of evidence 1b)
- Pilates: there is inconclusive evidence that pilates is effective in reducing pain and disability in people with CLBP. More research is necessary. (21) (level of evidence 1a)
- Yoga: may be an efficacious adjunctive treatment for CLBP. Strongest and most consistent evidence is there for the short-term benefits on functional disability. More research is necessary. (24) (level of evidence 1a)
Biopsychosocial rehabilitation (cognitive behavioural therapy)
For patients with nonspecific chronic low back pain, more specifically patients who have already had full conservative treatment, a biopsychosocial rehabilitation program might result in positive long term effects on pain and disability. (14) (level of evidence 1a) For more information see: CBT approach to Chronic Low Back Pain
Also pain education and graded exercise therapy could play an important role. There has not been found a significant difference between the effect of motor control exercises and graded exercise therapy, but subgroups of patients might respond better to one of these interventions. (23) (level of evidence 1b)
Key Research[edit | edit source]
Evidence for Cognitive-Behavioral Approach for Management of Chronic Low Back Pain, Bill Garcia, Evidence in Motion, OMPT Fellowship, 2009
Resources
[edit | edit source]
https://www.youtube.com/watch?v=DBh4_7YtLaA
Clinical Bottom Line[edit | edit source]
A multidisciplinary approach in treating chronic low back pain is advised. Especially in patients who have already failed a course of conservative treatment, multidisciplinary rehabilitation programmes result in better outcomes with respect to long term pain and disability compared with usual care or physical treatments. Physical therapy should consist of exercise therapy (and no manual therapy). The exercise therapy might be general exercise therapy, the Mckenzie method, or motor control exercises. Pilates and yoga could be used if the patient has interest in this. Biopsychosocial rehabilitation is advised in patients with nonspecific chronic low back pain, education and graded exercise could also play an important role for these patients. Above all, it’s important to choose a therapy that fits the individual patient.
Recent Related Research (from Pubmed)
[edit | edit source]
References[edit | edit source]