Autism Spectrum Disorder and Motor Development: Difference between revisions
No edit summary |
No edit summary |
||
| Line 60: | Line 60: | ||
== Promoting Physical Education and Physical Fitness to ASD Children == | == Promoting Physical Education and Physical Fitness to ASD Children == | ||
One of the reasons of the low participation rate in Physical Education (PE) for children with ASD (53%) and ADHD (38%) could be associated with problems in main diagnosis, by motor impairments.<ref>Kopp S, Beckung E, Gillberg C. Developmental coordination disorder and other motor control problems in girls with autism spectrum disorder and/or attention-deficit/hyperactivity disorder. Research in developmental disabilities. 2010 Mar 1;31(2):350-61.</ref> Cairney et al (2005) found that children with DCD are less likely to be physically active.<ref>Cairney J, Hay JA, Faught BE, Wade TJ, Corna L, Flouris A. Developmental coordination disorder, generalized self-efficacy toward physical activity, and participation in organized and free play activities. The Journal of pediatrics. 2005 Oct 1;147(4):515-20.</ref> | |||
It has been argued that a need for better-tailored PE for children with neuropsychiatric disorder, promoting the development of motor skills, the sense of self-efficacy and physical fitness are crucial.<ref>Chan JM, Lang R, Rispoli M, O’Reilly M, Sigafoos J, Cole H. Use of peer-mediated interventions in the treatment of autism spectrum disorders: A systematic review. Research in autism spectrum disorders. 2009 Oct 1;3(4):876-89.</ref> | |||
The United Nations Sustainable Development Goals | The United Nations Sustainable Development Goals suggested the importance of early childhood development to enable children to reach their full potential, with physical development being the top priority, and a critical component for growth.<ref>Black MM, Walker SP, Fernald LC, Andersen CT, DiGirolamo AM, Lu C, McCoy DC, Fink G, Shawar YR, Shiffman J, Devercelli AE. Early childhood development coming of age: science through the life course. The Lancet. 2017 Jan 7;389(10064):77-90.</ref> <ref>World Health Organization. International Classification of Functioning, Disability, and Health: Children & Youth Version: ICF-CY. World Health Organization; 2007.</ref>It is widely accepted that children are required to perform basic motor skills such as locomotor (running and jumping), balance (standing on one leg), object control (catching, throwing and kicking) and fine motor tasks (using a pencil and scissors)<ref>Robinson LE, Stodden DF, Barnett LM, Lopes VP, Logan SW, Rodrigues LP, D’Hondt E. Motor competence and its effect on positive developmental trajectories of health. Sports medicine. 2015 Sep 1;45(9):1273-84.</ref><ref name=":5">Barnett, L.M., Van Beurden, E., Morgan, P.J., Brooks, L.O. and Beard, J.R., 2009. Childhood motor skill proficiency as a predictor of adolescent physical activity. ''Journal of adolescent health'', ''44''(3), pp.252-259.</ref> | ||
For example, motor skills are said to form the foundation for sport-specific skills are predictive of physical activity participation and have been linked with cognitive outcomes.<ref name=":5" /> | For example, motor skills are said to form the foundation for sport-specific skills are predictive of physical activity participation and have been linked with cognitive outcomes.<ref name=":5" /> Poor motor skills has also been reflected in childhood obesity and which is associated with short and long term adverse health related consequences.<ref>Rivilis I, Hay J, Cairney J, Klentrou P, Liu J, Faught BE. Physical activity and fitness in children with developmental coordination disorder: a systematic review. Research in developmental disabilities. 2011 May 1;32(3):894-910.</ref> Furthermore, a deficit in motor skills may insisted the presence of a developmental or medical condition, requiring specialised interventions.<ref name=":4">Poon JK, Larosa AC, Pai GS. Developmental delay: timely identification and assessment. Indian pediatrics. 2010 May;47(5):415-22.</ref> | ||
In children | In ASD children with poor motor performance, it is recommend that early intervention programmes focus on motor development. Physiotherapists can stimulate the learning of functional motor skills or to help the child to compensate for motor skills disturbances. | ||
[[File:Autism Physical Education .jpg|center|thumb]] | [[File:Autism Physical Education .jpg|center|thumb|324x324px]] | ||
{{#ev:youtube| nJIVChOpVhk}}<ref>The Importance of Motor Function and Physical Activity in Autism Spectrum Disorder Available from: https://www.youtube.com/watch?v=nJIVChOpVhk [last accessed 10/09/2020]</ref> | {{#ev:youtube| nJIVChOpVhk}}<ref>The Importance of Motor Function and Physical Activity in Autism Spectrum Disorder Available from: https://www.youtube.com/watch?v=nJIVChOpVhk [last accessed 10/09/2020]</ref> | ||
Revision as of 08:30, 13 September 2020
Original Editor - Alan Jit Ho Mak
Top Contributors - Alan Jit Ho Mak, Niha Mulla, Ahmed M Diab, Mahbubur Rahman, Aminat Abolade, Kim Jackson and Ines Musabyemariya
What is Autism Spectrum Disorder?[edit | edit source]
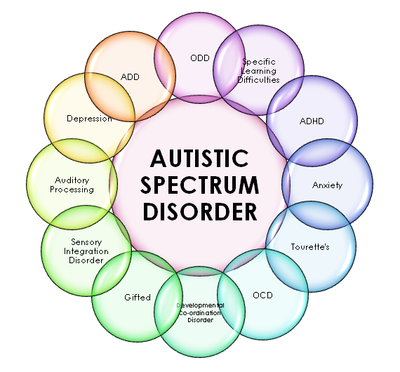
Autism is a complex neurological and developmental disability that appears within early developmental stages of life. Autism affects the normal functioning of the brain, communication development as well as social skills of the child.[1] Autism has been regarded as a life-long condition and it cannot be cured. However, severity may decrease through special education and treatments. Males tends to have a higher prevalence than female.[1]
The Diagnostic and Statistical Manual of Mental Disorders I (DISM-I) had not made autism in its own diagnostic criteria.[2] It is only from DSM-II, Autism has placed in a distinct diagnostic category. [3] In DSM-V, Autism has been altered to Autism Spectrum Disorders (ASD).[4]
According to the DSM, Autism is related to a group of conditions that were included collectively in the diagnosis. In order for an individual to be diagnosed with ASD, he/she must meet all the criteria for the impairment of social interaction, communication and at least two signs of repetitive behaviour.[4] An individual whose condition would have previously met the criteria for Asperger’s Syndrome or a Pervasive Developmental Disorder – Not Otherwise Specified (PDD-NOS) would not be considered as ASD with a lower severity level.
To date, the cause for ASD is still unknown. Some argued it is a result from the abnormalities in the rate of early brain development.[5] Happe and Ronald (2008) explained the most common contributory genetic, cognitive as well as neurodevelopmental factors that contribute to the characteristic triad of symptoms of ASD (For example, language delay, social impairment and repetitive behaviour).[6]
Kinney et al., (2010) has explored nine environmental factors for which exposure prior to conception appears to be associated with increased risk for autism.[7] It is crucial to identify these factors which may include environmental change, medical and physiotherapy interventions which maybe conceivable to limit the activating vulnerability and consequently to lessen the prevalence of the vulnerabilities and their association with ASD.[8]
It is not doubt that the prevalence of ASD around the globe among children is on the rise. Phetrasuwan, Miles and Mesiiboy (2009) indicated that in the United States, there were 0.4 or 0.5 children with ASD among 1,000 children prior 1985 and the recently this has been increased to 1 in 150 children. According to 2010 statistics from the Centres for Disease Control and Prevention, 1/100 children in the US is diagnosed with some form of Autism.[9]
The children with ASD diagnosis presents some core deficits, the symptoms can be diverse, ranging from those severely affected by numerous attributes to fewer characteristics.[9] However, Isaksen, Diseth, Schjølberg and Skjeldal (2013) argued that it maybe unclear as to whether the increase in the prevalence of autism represents a genuine change in the commonality of the disorder or simply due to the methodological issues, broadening of diagnostic criteria, and increase public and professional familiarity with the conditions or better accessibility of services.[10]
Physiotherapy Treatments For Autism Spectrum Disorder Children[edit | edit source]
The developmental delays could possibly affect the children’s gross and fine motor skills. The goals of physiotherapy to gather information from parents, clinical physicians and other multi-disciplinary team members. The role of the physiotherapist is to take care of autistic children with motor impairments in the body (for instance; issues with respiratory control and coordination level, improvement in posture, and addressing misalignments in the musculoskeletal system including chest wall deformities as well as foot and ankle misalignments issues.[11]
Normally, the assessments and treatments can take place in various settings (for examples: home, day care, community centres, clinics, hospitals, rehabilitation centres and fitness centres.) Physiotherapists also involve with rehabilitation after injuries where a child maybe injured from a fractured leg and required rehabilitation treatments. However, the physiotherapists must take the diagnosis of autism into consideration when designing treatments sessions. This is due to the fact that many of the physiotherapy sessions are very structured in nature. Teaching them to be comfortable and competent in their bodies is an essential part of the treatment.[11]
Characteristics For ASD Children with Motor Difficulties[edit | edit source]
Children with ASD may appear awkward in their motor skills and movement. Many of these coordination problems when combined with communication, social skills and behavioural problems can lead to more complex learning difficulties in the later development such as playground and sporting skills.[11]
Exercise based physiotherapy treatments include age-appropriate physical and motor skills, like jumping, clapping hands, skipping, hopping and throwing, kicking or catching a ball.
Hydrotherapy For ASD Children[edit | edit source]
In relation to motor skill development, physiotherapists had argued that swim instruction methods for children with an ASD can lead to faster learning of these skills. Some research argued that Hydrotherapy can be a beneficial form of exercise for Autistic children. In addition, exercise-based physiotherapy can be highly beneficial for children with Autism.
Hydrotherapy has been commonly used to treat Autism patients. This usually takes place in a swimming pool. The pressure and temperature of the water pressing against the body can sooth an autistic child. Water as a property form can provide a claiming sensory input while the child preforms exercises designed to improve range of motion and overall mobility. Warm water can recue body weight by 90%, decreases the force of impact on the body, relaxes muscles and reduces spasticity, making water the ideal medium to rehabilitate the body (Russell B. Lang et al., 2010).
Motor Control Difficulties in ASD Children[edit | edit source]
Some children without a clear neurological disorder present with poor motor abilities before 7 years of age. Some of these children could be considered to have DCD in DSM-IV-TR criteria.
However, it appears from the literature that the large majority of children with DCD are identified after starting school. In some cases, poor motor performance at preschool age. Is one of the first clear signs of another (comorbid) developmental disorder with more prominent behavioural features, such as ASD or ADHD.
Although motor disorders can occur in isolation, many studies have described their frequent co-occurrence with ADHD and ASD.
Motor control difficulties are very common in ASD children. Developmental Coordination Disorder (DCD) is found to present in about half of all individuals with ASD and ADHD. Recently, research has increase in the search for the links between DCD and ASD (Dewey et al., 2007; Green et al., 2009; Pan et al., 2009; Piek & Dyck, 2004; Sergeant et al., 2006; Toplak & Tannock, 2005).
Study by Kopp found that school girls with ASD and/or ADHD, with average or near average intellectual level, had more motor coordination problems than girls from the community. Among clinic preschool girls with ASD 4/5 had motor coordination problems. Some differences in motor and sensory performance were found across the main diagnostic groups, with more gross motor and sensation impairments in the ASD group than the group with ADHD.
Motor coordination problems were also related to lower ability in daily living skills. This study has recruited from a sample of girls referred to a specialist clinic. They were not representative of girls with ASD and or ADHD in the general population.
Daily living skills and motor impairments in school girls.
In the study, problems with daily living constitute a well-known phenomenon among children with neuropsychiatric disorders. In the study by Kopp et al., 2009, theyreported low scores on the VABS-DLS for girls with ASD and/or ADHD. The present study by Koop found that there is a significant relationship between motor impairments and lower abilities in daily living skills (VABS-DLS). These result confirm that poor adaptive daily skills are not only related to social, communicative and attention impairments but also to motor problems.
Promoting Physical Education and Physical Fitness to ASD Children[edit | edit source]
One of the reasons of the low participation rate in Physical Education (PE) for children with ASD (53%) and ADHD (38%) could be associated with problems in main diagnosis, by motor impairments.[12] Cairney et al (2005) found that children with DCD are less likely to be physically active.[13]
It has been argued that a need for better-tailored PE for children with neuropsychiatric disorder, promoting the development of motor skills, the sense of self-efficacy and physical fitness are crucial.[14]
The United Nations Sustainable Development Goals suggested the importance of early childhood development to enable children to reach their full potential, with physical development being the top priority, and a critical component for growth.[15] [16]It is widely accepted that children are required to perform basic motor skills such as locomotor (running and jumping), balance (standing on one leg), object control (catching, throwing and kicking) and fine motor tasks (using a pencil and scissors)[17][18]
For example, motor skills are said to form the foundation for sport-specific skills are predictive of physical activity participation and have been linked with cognitive outcomes.[18] Poor motor skills has also been reflected in childhood obesity and which is associated with short and long term adverse health related consequences.[19] Furthermore, a deficit in motor skills may insisted the presence of a developmental or medical condition, requiring specialised interventions.[20]
In ASD children with poor motor performance, it is recommend that early intervention programmes focus on motor development. Physiotherapists can stimulate the learning of functional motor skills or to help the child to compensate for motor skills disturbances.
Conclusion[edit | edit source]
Physiotherapy treatments and education to ASD children are important due to the motor related difficulties they encounter during their developmental stage. The treatments had been successful in improving and decreasing the severity level of their weak muscle control which result in many other consequences when they grow up. Physiotherapists should engage in plays where they can teach the children to be confident and comfortable of their bodies. This will lead to better outcome in the future for many ASD children.
References[edit | edit source]
- ↑ 1.0 1.1 Durand VM, Barlow DH. Essentials of abnormal psychology. Cengage Learning; 2012 Jul 27.
- ↑ American Psychiatric Association. Mental disorders. American Psychiatric Association; 1952.
- ↑ American Psychiatric Association. Mental disorders (3rd ed).American Psychiatric Association; 1980.
- ↑ 4.0 4.1 American Psychiatric Association. Mental disorders (5th ed). American Psychiatric Association; 2013.
- ↑ Caronna EB, Milunsky JM, Tager-Flusberg H. Autism spectrum disorders: clinical and research frontiers. Archives of disease in childhood. 2008 Jun 1;93(6):518-23.
- ↑ Happé F, Ronald A. The ‘fractionable autism triad’: a review of evidence from behavioural, genetic, cognitive and neural research. Neuropsychology review. 2008 Dec 1;18(4):287-304.
- ↑ Kinney DK, Barch DH, Chayka B, Napoleon S, Munir KM. Environmental risk factors for autism: do they help cause de novo genetic mutations that contribute to the disorder?. Medical hypotheses. 2010 Jan 1;74(1):102-6.
- ↑ Herbert MR. Contributions of the environment and environmentally vulnerable physiology to autism spectrum disorders. Current opinion in neurology. 2010 Apr 1;23(2):103-10.
- ↑ 9.0 9.1 Phetrasuwan S, Miles MS, Mesibov GB. Defining autism spectrum disorders. Journal for Specialists in Pediatric Nursing. 2009 Jul 1;14(3):206.
- ↑ Isaksen J, Diseth TH, Schjølberg S, Skjeldal OH. Autism spectrum disorders–are they really epidemic?. European Journal of Paediatric Neurology. 2013 Jul 1;17(4):327-33.
- ↑ 11.0 11.1 11.2 Zechariah Jebakumar A. Physiotherapy Cures Autism: A Review. International Journal of Pharmacy & Therapeutics, 8(2), 2017, 76-79.
- ↑ Kopp S, Beckung E, Gillberg C. Developmental coordination disorder and other motor control problems in girls with autism spectrum disorder and/or attention-deficit/hyperactivity disorder. Research in developmental disabilities. 2010 Mar 1;31(2):350-61.
- ↑ Cairney J, Hay JA, Faught BE, Wade TJ, Corna L, Flouris A. Developmental coordination disorder, generalized self-efficacy toward physical activity, and participation in organized and free play activities. The Journal of pediatrics. 2005 Oct 1;147(4):515-20.
- ↑ Chan JM, Lang R, Rispoli M, O’Reilly M, Sigafoos J, Cole H. Use of peer-mediated interventions in the treatment of autism spectrum disorders: A systematic review. Research in autism spectrum disorders. 2009 Oct 1;3(4):876-89.
- ↑ Black MM, Walker SP, Fernald LC, Andersen CT, DiGirolamo AM, Lu C, McCoy DC, Fink G, Shawar YR, Shiffman J, Devercelli AE. Early childhood development coming of age: science through the life course. The Lancet. 2017 Jan 7;389(10064):77-90.
- ↑ World Health Organization. International Classification of Functioning, Disability, and Health: Children & Youth Version: ICF-CY. World Health Organization; 2007.
- ↑ Robinson LE, Stodden DF, Barnett LM, Lopes VP, Logan SW, Rodrigues LP, D’Hondt E. Motor competence and its effect on positive developmental trajectories of health. Sports medicine. 2015 Sep 1;45(9):1273-84.
- ↑ 18.0 18.1 Barnett, L.M., Van Beurden, E., Morgan, P.J., Brooks, L.O. and Beard, J.R., 2009. Childhood motor skill proficiency as a predictor of adolescent physical activity. Journal of adolescent health, 44(3), pp.252-259.
- ↑ Rivilis I, Hay J, Cairney J, Klentrou P, Liu J, Faught BE. Physical activity and fitness in children with developmental coordination disorder: a systematic review. Research in developmental disabilities. 2011 May 1;32(3):894-910.
- ↑ Poon JK, Larosa AC, Pai GS. Developmental delay: timely identification and assessment. Indian pediatrics. 2010 May;47(5):415-22.
- ↑ The Importance of Motor Function and Physical Activity in Autism Spectrum Disorder Available from: https://www.youtube.com/watch?v=nJIVChOpVhk [last accessed 10/09/2020]