Functional Anatomy of the Hand
Original Editor - Ewa Jaraczewska
Top Contributors - Ewa Jaraczewska and Jess Bell
Introduction[edit | edit source]
The hand, positioned at the end of the upper limb, is a combination of complex joints whose function is to manipulate, grip and grasp. These movements are made possible by the opposing movement of the thumb.
Key Terms[edit | edit source]
Axes: lines around which an object rotates. The rotation axis is a line that passes through the centre of mass. There are three axes of rotation: sagittal passing from posterior to anterior, frontal passing from left to right, and vertical passing from inferior to superior. The rotation axes of the foot joints are perpendicular to the cardinal planes. Therefore, motion at these joints results in rotations within three planes. Example: supination involves inversion, internal rotation, and plantarflexion.
Bursae: reduce friction between the moving parts of the joints. A bursa is a fluid-filled sac. There are four types of bursae: adventitious, subcutaneous, synovial, and sub-muscular.
Capsule: one of the characteristics of the synovial joints. It is a fibrous connective tissue which forms a band that seals the joint space, provides passive and active stability and may even form articular surfaces for the joint. The capsular pattern is "the proportional motion restriction in range of motion during passive exercises due to tightness of the joint capsule."
Closed pack position: the position with the most congruency of the joint surfaces. In this position, joint stability increases. For example, the closed pack position for the interphalangeal joints is full extension.
Degrees of freedom: the direction of joint movement or rotation; there is a maximum of six degrees of freedom, including three translations and three rotations.
Ligament: fibrous connective tissue that holds the bones together.
Open (loose) pack position: position with the least joint congruency where joint stability is reduced.
Planes of movement: describe how the body moves. Up and down movements (flexion/extension) occur in the sagittal plane. Sideway movements (abduction/adduction) occur in the frontal plane. The transverse plane movements are rotational (internal and external rotation).
Hand Structure[edit | edit source]
The structure of the human hand includes 27 bones: eight carpal bones, five metacarpal bones, and fourteen digital bones, including fingers and thumb. The bony segments of the hand are arranged in a series of longitudinal and transverse arches. The bones of the five digital rays are part of the longitudinal arches. There are two transverse arches: the proximal and the distal. The proximal transverse arch is made up of carpal bones. The metacarpal heads of the fingers belong to the distal transverse arch.[1]
The Carpus (Carpal Bones)[edit | edit source]
Proximal raw:
The scaphoid (navicular): belongs to the proximal raw of the carpal bones. Located the most laterally. Its palmar surface contains the tubercle, the muscles' attachment point and the anatomical snuffbox floor.
The lunate: part of the proximal raw of the carpal bones. It articulates with the scaphoid on the lateral and the triquetrum on the medial side.
The triquetrum: other names include triquetral, triangular, or cuneiform bone. It is a triangular and pyramidal-shaped bone located in the proximal raw, on the medial side of the wrist. It contains multiple articulation surfaces: lateral for the lunate, anterior for the pisiform, and distal for the hamate.
Distal raw:
The trapezium: located in the distal raw of the carpal bones, on its radial side. It has four articulations for the first metacarpal, second metacarpal, scaphoid and trapezoid bones. This bone is part of the mechanism responsible for the wide mobility of the human hand, where the articulation between the first metacarpal and the trapezium allows for the opposable thumbs function.
The trapezoid: The lesser multangular bone is another name for this bone. This is the smallest bone of the distal raw of the carpal bones. It gives structure to the palm of the hand.
The capitate: the largest and most central carpal bone belonging to the distal raw. It articulates with the bases of the 2nd and 3rd metacarpal bones, forming part of the common carpometacarpal joint in the hand. In addition, it articulates with the following: scaphoid and lunate on the proximal, trapezoid on the lateral, and the hamate on the medial surfaces.
The hamate: sits on the medial side of the distal row of carpal bones. The hook of the hamate is the bony process extending from the palmar surface. This carpal bone forms the medial border of the carpal tunnel.
The Metacarpus (Metacarpal Bones)[edit | edit source]
Five bones- the metacarpals, make up the metacarpus. Each metacarpal bone articulates with one or more carpal bones:
- First metacarpal articulates with the trapezium
- Second metacarpal articulates with the trapezium, trapezoid and capitate
- Third metacarpal articulates with the capitate
- Fourth and fifth metacarpal articulate with the hamate
Additionally, the second to fifth metacarpals articulate with each other.
The Phalanges[edit | edit source]
Long finger bones are known as phalanges. Apart from the thumb (the pollex), which only has distal and proximal bones, each phalanx has three bones: the distal, middle and proximal phalanx. The middle and proximal phalanges consist of a base, a body, and the head, which is the distal part of the phalanx. [2]
The thumb: the typical position of the thumb is pronation and approximately 80 degrees of flexion in relation to the remaining metacarpals of the hand. This position allows opposition of the thumb to the digits.[1]
The index finger: second the most important finger of the hand. It is able to abduct, adduct, flex and extend. The index finger participates in precision pinch and directional grip. [1]
The long finger: is centrally positioned, which makes it involved in power grip and precision movements.[1]
The ring finger: weak and only randomly used in precision grip or pinch manoeuvres. When lost, it leads to the least amount of impairment in the hand.[1]
The small finger: the weakest of all fingers, but important in grasping while spanning an object manoeuvres due to its ability to abduct.[1]
Bones, Articulations and Kinematics of the Hand[edit | edit source]
Bones and Articulations[edit | edit source]
| Bones | Articulations | Characteristics | Key palpation points |
|---|---|---|---|
| Distal row of carpal bones
Proximal bases of five metacarpal bones |
The carpometacarpal joints (CMC):[3]
|
The mobility of the CMC joints increases from radial to ulnar sides of the hand.[3]
1CMC (TMCJ) is located on the radial aspect of the wrist. Does not contain bony stabilizers. Instead, the stability is provided by five internal ligaments: dorsal radial, posterior oblique, the first intermetacarpal, ulnar collateral, and anterior oblique ligaments. 2CMC and 3CMC: belong to the central column of the hand, relatively rigid. 1CMC, 4CMC, 5 CMC: relative mobility, with 4CMC and 5CMC contributing the most to hand mobility. |
Place the patient's hand on the side with the radial side up to palpate the first CMC jointp. Slide your finger along the patient's thumb down tothe first metacarpal. Just below the first metacarpa,l you will feel a divot. The trapezium bone is located just below it. The first metacarpal articulates with the trapezium.
The trapezoid bone is located between the trapezium and the capitate. It articulates with the second metacarpal. To find the capitate, slide your finger down along the middle finger to reach the third metacarpal bone. You have located the capitate bone when your finger drops into a duvet (indentation). It articulates with the third metacarpal. To palpate the hamate bone, first locate the hook of the hamate. Turn the patient's hand with the palmar (volar) side up and place your finger on the hypothenar region. You can palpate the hook and the hamate bone in the hypothenar eminence. The hook of the hamate is tender, and gentle compression on the bone may be unpleasant for the patient. The fourth and the fifth metacarpals articulate with the hamate. |
| Metacarpal bones
Proximal phalanges |
Metacarpophalangeal (MCP) joints | Consider being the most important joint for hand function as they contribute 77% of the total arc of finger flexion[1] | To locate the proximal phalanges, look at the joints associated with them. Flex the patient's finger. The proximal phalanx is located between the proximal and the middle knuckle of this finger or between the palmar crease and the middle crease of the finger.
The joint space of the MCP joint is located at about one centimetre distal to the tip of the knuckle. |
| Proximal, middle, and distal phalanges | Interphalangeal joints
|
The function of the interphalangeal joints of the hand is to permit fine motor movements in the digits. It includes providing flexion towards the palm. | The PIP and DIP joint space correspond to the flexor crease. |
Hand Kinematics[edit | edit source]
Hand biomechanics consists of seven fundamental manoeuvres needed for basic functions. They involve specific motions which must occur at the wrist, thumb and fingers:[1]
- The precision pinch, or the terminal pinch, is used to pick up a small object, like a pen.
- Motion required: flexion of the interphalangeal (IP) joint of the thumb and the distal IP (DIP) joint of the index finger.
- The oppositional pinch, or the subterminal pinch with the thumb opposition. The index finger's pulp connects with the thumb's pulp needed to hold a piece of paper.
- Motion required: Extension of the IP and DIP joints.
- The key pinch requires stability provided by the index finger, the optimal length of the digit and a metacarpal phalangeal joint (MCP).
- Motion required: thumb adduction to the radial aspect of the index finger’s middle phalanx.
- The chuck grip, or a directional grip, is used to perform the action that requires an application of rotational and axial forces like when using a screwdriver.
- Motion required: a combined motion of the index finger, long finger, and thumb.
- The hook grip allows one to hold a briefcase by its handle. No thumb function is required in this manoeuvre.
- Motion required: finger flexion at the IP joints and extension at the MCP joints.
- The power grasp is needed to grip a club or a bat.
- Motion required: fingers and thumb flexion, thumb opposition relative to the other digits
- The span grasp manoeuvre is based on the stability of the thumb, metacarpophalangeal (MCP) and interphalangeal (IP) joints. The span grasp is utilised when grabbing a ball.
- Motion required: 30 degrees flexion of DIP joints and the proximal IP (PIP) joints, thumb abduction towards the palm
| Joint | Type of joint | Plane of movement | Motion | Kinematics | Closed pack position | Open pack position |
|---|---|---|---|---|---|---|
| The carpometacarpal joints (CMC) | 1CMC:
Synovial, saddle joint. 2CMC/3CMC: Synarthrotic with almost no movement under physiological conditions. 4CMC/5CMC: Synovial, saddle joint. |
1CMC:
Flexion/extension occurs in the frontal plane as the thumb is rotated at 90 degrees in relation to the plane of the hand [5] Abduction/adduction occurs in the sagittal plane External/internal rotation (axial rotation) where the axis is the length of the thumb Thumb opposition: all thumb movements combined together
2CMC/3CMC: Nonaxial, translational movements. 4CMC/5CMC: Sagittal (flexion/extension) Frontal (abduction/adduction) |
1CMC:
Flexion/extension Abduction/adduction Axial rotation 2CMC/3CMC: Nonaxial, translational movements only. 4CMC/5CMC: Flexion/extension Abduction/adduction |
1CMC: [5] Flexion/extension: total motion of 40-50 degrees
Abduction/adduction: total motion of 80 degrees Axial rotation: total motion of 70-110 degrees 2CMC/3CMC: Nonaxial, translational movements only. 4CMC:[6] Flexion/extension: 10/0 degrees Abduction/adduction: 5/0 degrees. 5CMC:[6] Flexion/extension: 20/0 degrees Abduction/adduction: 13/0 degrees
|
1CMC: maximum opposition
|
1CMC:slight flexion
|
| Metacarpophalangeal (MCP) joints | Condyloid joint | Sagittal
Frontal |
Flexion/extension
Abduction/ adduction Mild to moderate rotation of the digit. |
Thumb MCP:
Flexion/extension: 55 degrees/35 degrees Abduction/adduction: 25-30 degrees total range Second to fifth MCP: Flexion: 90 degrees Extension: 10-30 degrees Abduction/adduction: 25-30 degrees |
Thumb MCP: maximum opposition
|
Slight flexion |
Interphalangeal joints (IP)
|
Hinge | Sagittal | Flexion/Extension | Thumb:
Flexion: 90 degrees Extension: 10-15 degrees Second to fifth PIP: Flexion: 70-100 degrees (depends on the digit, with digit 5 having the least flexion range of motion) Extension: 2-5 degrees Second to fifth DIP: Flexion: 50 degrees Extension: 15 degrees |
Full extension | Slight flexion |
Hand Passive Range of Motion[edit | edit source]
Watch this video to learn about the thumb passive range of motion assessment using a goniometer:
Watch this video to learn about the fingers' passive range of motion assessment using a goniometer:
Ligaments of the Hand[edit | edit source]
Ligaments Supporting Carpometacarpal Joints[edit | edit source]
Trapeziometacarpal Joint (TMCJ) Ligaments[edit | edit source]
| Key ligaments | Origin | Insertion | Action/role |
|---|---|---|---|
Anterior oblique ligament (AOL) ("beak ligament"):[9]
|
Palmar tubercle of the trapezium | Volar beak of the first metacarpal base at the palmar and ulnar surface | A static stabilizer of TMCJ
Prevents dorsoradial subluxation of thumb metacarpal during key pinch[10] Degeneration of AOL frequently leads to osteoarthritis of the first CMC joint.[11] |
| Posterior oblique ligament (POL) | Dorsal-ulnar aspect of the trapezium | The dorsal-ulnar aspect of the thumb metacarpal and the palmar-ulnar tubercle | Secondary role in CMC joint stability
Prevents radial translation |
| Ulnar collateral ligament (UCL) | Distal and ulnar margin of the flexor retinaculum insertion onto the trapezial ridge | Superficial and ulnar to the superficial anterior oblique ligament on the volar-ulnar tubercle of the first metacarpal base. | Prevents the thumb from side-to-side movement |
| First intermetacarpal ligament (1stIMCL) | Dorsoradial aspect of the second metacarpal, radial to the extensor carpi radialis longus tendon insertion | Volar-ulnar tubercle of the first metacarpal base | Connects the thumb metacarpal bone to the index finger metacarpal |
| Dorsoradial ligament (DRL) | Dorsoradial tubercle of the trapezium | Dorsal edge of the base of the thumb metacarpal.[12] | The strongest and stiffest of TMCJ ligaments
The primary stabiliser of the TMCJ. [12] Proprioceptive function due to rich innervation |
Carpometacarpal Joints 2-5 (2CMC-5CMC) Ligaments[edit | edit source]
| Key ligaments | Origin | Insertion | Action/role |
|---|---|---|---|
| Palmar (volar) carpometacarpal ligaments | Palmar (volar) surfaces of the distal row of carpal bones:
2CMC:trapezium and trapezoid 3CMC:trapezium/trapezoid, capitate, hamate 4CMC:capitate and hamate 5CMC:hamate |
Palmar (volar) four medial metacarpal bases | CMC joint stabilisers |
| Dorsal carpometacarpal ligaments | Dorsal surfaces of the distal row of carpal bones:
2CMC:trapezium and trapezoid 3CMC:trapezoid and capitate 4CMC:capitate and hamate 5CMC:hamate |
Dorsal four medial metacarpal bases | |
| Interosseous ligament:
Lateral band(LB) Medial band(MB) |
Inferior aspect of the distal margins of the capitate and hamate bones:
LB: capitate MB: hamate |
Third and fourth metacarpal bases:
LB: third metacarpal base MB: fourth metacarpal base |
Ligaments Supporting Metacarpophalangeal Joints[edit | edit source]
| Key ligaments | Origin | Insertion | Action/role |
|---|---|---|---|
| Collateral ligaments:
Proper collateral ligaments (PCL) Accessory collateral ligaments (ACL) |
PCL: posterior tubercles on the dorsolateral aspect of the metacarpal head
ACL: proximal to the metacarpal head |
PCL: palmar aspect of the adjacent proximal phalanx, distal to the base
ACL: distal third of the palmar (volar) plate |
Stabilises the joint medially and laterally
Limits flexion and extension |
| Deep transverse metacarpal ligaments (2-5MCP only) | Run across the palmar aspect of the second to fifth metacarpophalangeal joints.[13] | Stabilises the transverse metacarpal arch | |
| Palmar ligament (volar plate) | The palmar aspect of the metacarpal neck
The palmar surface of the base of the adjacent proximal phalanx |
Blends with the collateral ligament | Prevents hyperextension of the MCP joint |
Ligaments Supporting Interphalangeal Joints[edit | edit source]
| Key ligament | Origin | Insertion | Action/role |
|---|---|---|---|
Collateral ligaments
|
Head of the more proximal phalanx | Volar third of the middle phalanx bases
AL: Attaches to the fibres of the palmar ligament |
Provide radio-ulnar stability
Prevent excessive adduction-abduction movements of the interphalangeal joints. |
| Palmar ligament (volar plate) | The palmar surface of the base of the distal phalanx | Blends with the accessory collateral ligaments | Prevents hyperextension of each IP joint |
Additional Structures[edit | edit source]
Pulleys of the Hand[edit | edit source]
Thickened areas of the flexor tendon sheath. The sheath holds the flexor tendons near the bone and converts the force generated in the muscle-tendon unit into movement at the phalanges. It helps maintain the tracking of the flexor tendons to the fingers during flexion and extension. There are two types of pulley systems in the hand:
- Annular pulleys are well-defined thickened tendon sheath areas going across the tendons.
- Cruciform pulleys provide the necessary flexibility for approximation of the annular pulley at flexion and maintain the integrity of the flexor sheaths.
You can read more on the hand pulleys here.
Muscles of the Hand[edit | edit source]
Hand muscles can be grouped into the extrinsic and intrinsic divisions:[4]
- Extrinsic division: muscles that originate on the forearm
- Intrinsic division: muscles that originate within the hand. They are divided into four groups:
- The interossei: dorsal interossei,palmar interossei
- The lumbricals
- The hypothenar muscles controlling the fifth finger: flexor digiti minimi brevis, abductor digiti minimi, opponens digiti minimi
- The thenar muscles controlling the thumb: flexor pollicis brevis, opponens pollicis, abductor pollicis brevis
Hand muscles can also be grouped according to their function into fingers flexors, extensors, abductors and adductors.
The table below presents the hand muscles according to their function:
Fingers Flexors[edit | edit source]
| Muscle | Origin | Insertion | Innervation | Action |
|---|---|---|---|---|
| Dorsal interossei | Adjacent metacarpal shafts | The bases of the proximal phalanges and the extensor apparatus. | Ulnar nerve | Abduct the fingers
Assist in flexion of the MCP joints Assist in extension of the IP joints |
| Palmar interossei | The first palmar interosseous: the medial side of the second metacarpal
The second and third interossei: the lateral side of the fourth and fifth metacarpals |
The proximal phalanx on the same side and the extensor apparatus | Flexion of the 2,4 and 5 MCP joints
Assist in the extension of the IP joints Assist in adduction in the MCP joints | |
| Lumbricals | Tendons of the flexor digitorum profundus | Extensor apparatus on the second to fifth fingers | First and second lumbricals: Median nerve
Third and fourth lumbricals: Ulnar nerve |
Flexion of MCP joints
Extension of the IP joints When interossei are paralyzed, the lumbrical can initiate flexion of the proximal phalanx.[1] |
| Flexor digitorum profundus | Ulnar shaft
The interosseous membrane |
Distal phalanges of fingers two to five through four tendons | Lateral part (fingers 2and 3): Anterior interosseous nerve (branch of the median nerve)
Medial part (fingers 4 and 5): Ulnar nerve |
Flexion of the MCP, PIP, and DIP joints |
| Flexor pollicis longus | The anterior surface of the shaft of the radius | Distal phalanx of the thumb | The anterior interosseous nerve | Flexion of the thumb MCP and IP joints |
Flexor digitorum superficialis (FDS)
|
HUH: medial epicondyle via the common flexor tendon and the coronoid process
RH: radial tuberosity |
HUH/RH: middle phalanges of fingers two to five | Median nerve | Flexion of the MCP and PIP joints |
Flexor pollicis brevis
|
Trapezium
Flexor retinaculum |
The base of the proximal phalanx of the thumb | SH:Median nerve
DH: Median and ulnar nerves |
Flexion of the CMC and MCP joints of the thumb |
| Opponens pollicis | Trapezium
Flexor retinaculum |
The shaft of the first metacarpal | Recurrent branch of median nerve | Flexion of the CMC joint of the thumb |
| Flexor digiti minimi brevis | Hamate
Flexor retinaculum |
The base of the proximal phalanx of the fifth finger. | Deep branch of ulnar nerve | Flexion of the MCP joint of the fifth finger. |
Fingers Extensors[edit | edit source]
| Muscle | Origin | Insertion | Innervation | Action |
|---|---|---|---|---|
| Dorsal interossei | Adjacent metacarpal shafts | The bases of the proximal phalanges and the extensor apparatus. | Ulnar nerve | Abduct the fingers
Assist in flexion of the MCP joints Assist in extension of the IP joints |
| Palmar interossei | The first palmar interosseous: the medial side of the second metacarpal
The second and third interossei: the lateral side of the fourth and fifth metacarpals |
The proximal phalanx on the same side and the extensor apparatus | Flexion of the 2,4 and 5 MCP joints
Assist in the extension of the IP joints Assist in adduction in the MCP joints | |
| Lumbricals | Tendons of the flexor digitorum profundus | Extensor apparatus on the second to fifth fingers | First and second lumbricals:
Median nerve Third and fourth lumbricals: Ulnar nerve |
Flexion of MCP joints
Assist in extension of the IP joints When interossei are paralyzed, the lumbrical can initiate flexion of the proximal phalanx.[1] |
| Extensor indicis | The shaft of the ulna and the interosseous membrane | The extensor apparatus of the index finger | Posterior interosseous nerve | Extension of the finger at the MCP and IP joints |
| Extensor pollicis brevis | The shaft of the radius and the interosseous membrane | The base of the proximal phalanx of the thumb | Thumb extension at the CMC and the MCP joints | |
| Extensor pollicis longus | The shaft of the radius and the interosseous membrane | The base of the distal phalanx of the thumb | Extension of the CMC, MCP, and IP joints | |
| Extensor digiti minimi | Lateral epicondyle of the humerus via the common extensor tendon | Extensor apparatus of the fifth finger | Extension of the fifth finger at the MCP and IP joints | |
| Extensor digitorum | Lateral epicondyle via the common extensor tendon | Extensor expansions of fingers two to five via four tendons | Extension of the MCP and IP joints of the second to fifth fingers |
Fingers Abductors[edit | edit source]
| Muscle | Origin | Insertion | Innervation | Action |
|---|---|---|---|---|
| Dorsal interossei | Adjacent metacarpal shafts | The bases of the proximal phalanges and the extensor apparatus. | Ulnar nerve | Abduct the MCP joints of the fingers
Assist in extension of the IP joints |
| Abductor digiti minimi | Pisiform and the flexor retinaculum | The base of the proximal phalanx of the fifth finger
The extensor apparatus |
Deep branch of the ulnar nerve | Abducts the fifth MCP joint |
| Abductor pollicis longus | posterior aspect of the radius and ulna and the interosseous membrane | The base of the first metacarpal | Posterior interosseous nerve | Abducts the thumb at the CMC joint |
| Abductor pollicis brevis | Scaphoid, trapezium, and flexor retinaculum | The base of the proximal phalanx of the thumb
The extensor apparatus. |
Recurrent branch of the median nerve | Abducts the thumb at the CMC and MCP joints |
Fingers Adductors[edit | edit source]
| Muscle | Origin | Insertion | Innervation | Action |
|---|---|---|---|---|
| Palmar interossei | The first palmar interosseous: the medial side of the second metacarpal
The second and third interossei: the lateral side of the fourth and fifth metacarpals |
The proximal phalanx on the same side and the extensor apparatus | Ulnar nerve | Flexion of the 2,4 and 5 MCP joints
Assist in adduction in the MCP joints |
The adductor pollicis :
|
OH: the bases of the second and third metacarpals, trapezoid, and capitate
TH: third metacarpal shaft |
OH/TH: the base of the proximal phalanx of the thumb | Deep branch of the ulnar nerve | Adduct the thumb at the CMC and MCP joints. |
Opposition[edit | edit source]
Opposition is the movement that brings the tip of the thumb to the tip of any of the other fingers. It is foundational for a pinch grip where you hold an object between the thumb and fingers of your hand.
| Muscle | Origin | Insertion | Innervation | Action |
|---|---|---|---|---|
| Opponens digiti minimi | Hamate and the flexor retinaculum | The shaft of the fifth metacarpal | Deep branch of ulnar nerve | Opposes the fifth finger to the thumb |
| Opponens pollicis | Tubercle of trapezium bone
and the flexor retinaculum |
Radial border of the first metacarpal | Recurrent branch of median nerve | Opposes the thumb to the other fingers |
| Palmaris brevis | Palmar aponeurosis | Skin of the palm on the ulnar border | Superficial branch of the ulnar nerve | Tenses the skin on the ulnar side to aid grip. |
Innervation of the Hand[edit | edit source]
The hand innervation is found to be highly variable due to presence of the anatomical variations within the ulnar and the median nerves. [14]The example of these variations include anastomoses that exist in the hand impacting the management and the outcome of median or ulnar nerve damage or entrapment. [15] Among all nerves innervating the hand, the median nerve presents a significant number of variations in its formation.[16]
| Nerve | Origin | Branches | Motor fibres | Sensory fibres |
|---|---|---|---|---|
| Radial nerve | Brachial plexus posterior cord | Superficial branch:
Deep branch:
Posterior brachial cutaneous nerve Inferior lateral brachial cutaneous nerve Posterior antebrachial cutaneous nerve Muscular branches |
Extrinsic extensors of the hand | Thumb's radial dorsal aspect
Dorsum of the hand |
| Ulnar nerve | Brachial plexus medial cord | Articular branches
Muscular branches The palmar and dorsal cutaneous branches Terminal branches in the hand:
|
The medial half of flexor digitorum profundus, hypothenar muscles, third and fourth lumbricals, the interossei, and adductor pollicis, extensor muscles, and abductor pollicis longus via a posterior interosseous nerve | Dorsomedial and ventromedial aspect of the hand |
| Median nerve | Brachial plexus lateral and medial cords | Palmar cutaneous branch:
Medial branch
Anterior interosseous |
Flexor digitorum superficialis, radial half of flexor digitorum profundus, flexor pollicis longus, first and second lumbricals, thenar eminence muscles | Lateral palm
Ventral lateral aspects of the thumb Ventral aspect of the index finger |
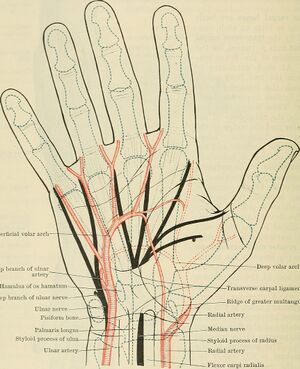
Vascular Supply of the Hand[edit | edit source]
The hand receives its blood supply from the radial, ulnar, and interosseous arteries. At the carpal level, the forearm arteries form three dorsal and three palmar arches:[17]
Palmar arches: radiocarpal arch, palmar intercarpal arch, distal palmar arch.
- The radiocarpal arch receives branches from the radial, ulnar, and the anterior interosseous arteries
- The palmar intercarpal arch receives blood supply from the radial, ulnar, and the anterior interosseous arteries
- The distal palmar arch receives vascular supply from recurrent arteries ( small branches from the radial and ulnar arteries).
Dorsal arches: dorsal radiocarpal arch, dorsal intercarpal arch, dorsal proximal metacarpal arch.
- The dorsal radiocarpal arch receives contributions from the radial artery, the ulnar artery, and a dorsal branch of the anterior interosseous artery
- The dorsal intercarpal arch receives contributions from the radial, ulnar, and the anterior interosseous arteries
- The dorsal proximal metacarpal arch is located at the carpometacarpal joints and supplies the dorsal skin of the hand
| Artery | Origin | Branches | Supply |
|---|---|---|---|
| Radial artery | Terminal branch of brachial artery |
|
Radial nerve, carpal bones and joints, thumb, and lateral side of the index finger, thenar muscles |
| Ulnar artery | Terminal branch of brachial artery |
|
Four fingers, forearm muscles, ulnar nerve, wrist bones and joints. |
| Interosseous artery | Common interosseous artery (branch of the ulnar artery) | Anterior and posterior interosseous arteries | Bones and muscles of the forearm |
Clinical Relevance[edit | edit source]
- Swan neck deformity is a condition characterised by flexion at the distal interphalangeal joint (DIP) and hyperextension at the proximal interphalangeal joint (PIP). This type of deformity can be caused by PIP extensors over-activity or a laxity at the volar plate.
- Boutonniere deformity is a fingers flexion deformity, in which the proximal interphalangeal joint (PIP) is flexed and the distal interphalangeal joint (DIP) is hyperextended. It is the result of the rupture of the central slip of the extensor tendon of a finger. Traumatic injury, rheumatoid arthritis, osteoarthritis, prolonged flexion contracture (Dupuytren's contracture), flexor pulley disruptions, and burns are all common causes that can lead to this deformity.[18]
- Finger pulley injuries are the most common in rock climbers. They are overuse type of injuries that occur during sporting activities due to demands placed on the finger.
Resources[edit | edit source]
- Tan RES, Lahiri A. Vascular Anatomy of the Hand in Relation to Flaps. Hand Clin. 2020 Feb;36(1):1-8
- Physical Exam of the Hand
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 1.8 1.9 Duncan SFM, Saracevic CE, Kakinoki R. Biomechanics of the Hand. Hand Clinics 2013; 29(4): 483-492
- ↑ Hacking C, Gaillard F, Worsley C, et al. Phalanges of the hands. Reference article, Radiopaedia.org. Available from https://radiopaedia.org/articles/phalanges-of-the-hands [last access 7.09.2023]
- ↑ 3.0 3.1 Ayhan Ç, Ayhan E. Chapter 13 - Kinesiology of the wrist and the hand. Angin S, Şimşek IE (editors). Comparative Kinesiology of the Human Body. Academic Press, 2020: pages 211-282.
- ↑ 4.0 4.1 Xuan D. Exploring Hand Anatomy. Plus 2023
- ↑ 5.0 5.1 Vasković J. Trapeziometacarpal joint. Available from https://www.kenhub.com/en/library/anatomy/trapeziometacarpal-joint. [last access 14.09.2023]
- ↑ 6.0 6.1 Rad A. Carpometacarpal (CMC) joints. Available from https://www.kenhub.com/en/library/anatomy/carpometacarpal-cmc-joints [last access 14.09.2023]
- ↑ TheUpperHand. Thumb (Range of Motion) Goniometry. Available from: https://www.youtube.com/watch?v=OzukYU2OIKg [last accessed 16/9/2023]
- ↑ TheUpperHand. Finger (Range of Motion) Goniometry. Available from: https://www.youtube.com/watch?v=JX5dO7n4-Lg [last accessed 16/9/2023]
- ↑ Ladd AL, Weiss AP, Crisco JJ, Hagert E, Wolf JM, Glickel SZ, Yao J. The thumb carpometacarpal joint: anatomy, hormones, and biomechanics. Instr Course Lect. 2013;62:165-79
- ↑ Iyengar K, Sree DV, Loh WYC. Clinical practice algorithm for Eaton's injury of the thumb. J Clin Orthop Trauma. 2020 Jul-Aug;11(4):537-541.
- ↑ Kamalasekar K, Ravikanth R. First Carpometacarpal Joint Anatomy and Osteoarthritis: MR Imaging Overview. Indian J Radiol Imaging. 2022 Jan 10;31(4):1012-1015
- ↑ 12.0 12.1 Cardoso FN, Kim HJ, Albertotti F, Botte MJ, Resnick D, Chung CB. Imaging the ligaments of the trapeziometacarpal joint: MRI compared with MR arthrography in cadaveric specimens. AJR Am J Roentgenol. 2009 Jan;192(1):W13-9.
- ↑ Grujičić R. Metacarpophalangeal (MCP) joints. Available from https://www.kenhub.com/en/library/anatomy/metacarpophalangeal-mcp-joints [last access 16.09.2023]
- ↑ Wynter S, Dissabandara L. A comprehensive review of motor innervation of the hand: variations and clinical significance. Surg Radiol Anat. 2018 Mar;40(3):259-269.
- ↑ Caetano EB, Vieira LA, Sabongi Neto JJ, Caetano MF, Sabongi RG. Riché-Cannieu Anastomosis: Structure, Function, and Clinical Significance. Rev Bras Ortop (Sao Paulo). 2019 Sep;54(5):564-571.
- ↑ Encarnacion M, Nurmukhametov R, Barrientos RE, Melchenko D, Goncharov E, Bernard E, Huerta JM, Uhl JF, Efe IE, Montemurro N, Ramirez I. Anatomical Variations of the Median Nerve: A Cadaveric Study. Neurol Int. 2022 Aug 23;14(3):664-672.
- ↑ Tan RES, Lahiri A. Vascular Anatomy of the Hand in Relation to Flaps. Hand Clin. 2020 Feb;36(1):1-8
- ↑ Lee JK, Lee S, Kim M, Jo S, Cho JW, Han SH. Anatomic Repair of the Central Slip with Anchor Suture Augmentation for Treatment of Established Boutonniere Deformity. Clin Orthop Surg. 2021 Jun;13(2):243-251.